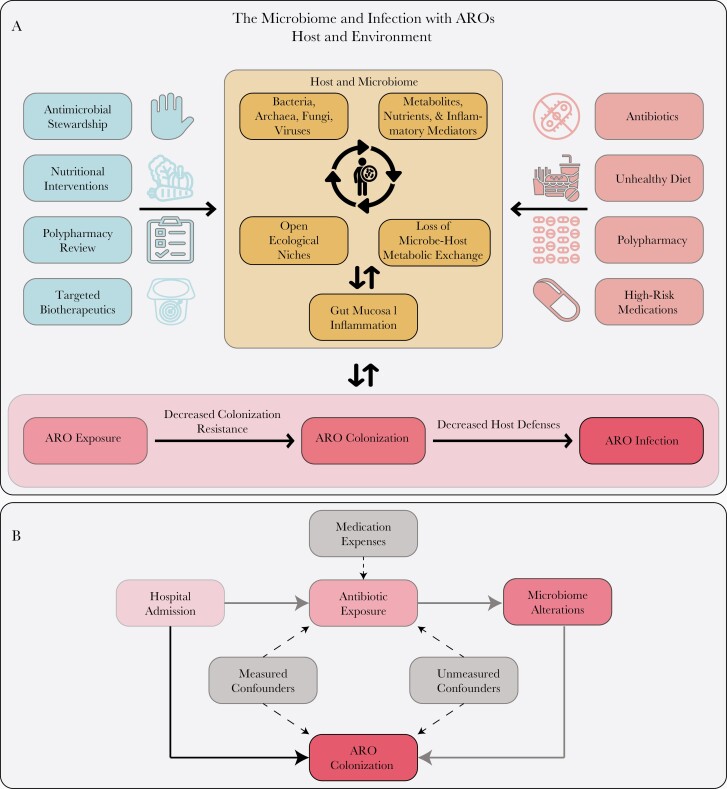
Figure 1.
A, Example conceptual framework for testing hypotheses about the microbiome and subsequent risk of infection with antibiotic-resistant organisms (AROs). Beneficial and detrimental host/environmental factors are shown on the left and right, respectively. The microbiome is modeled as a system of microbes and local environmental factors that interact to fill ecological niches and maintain metabolic exchange with the host, disruption of which can influence gut mucosal inflammation. The main hypothesis being tested should progress from a risk factor/predictor through the various components leading to ARO infection. Alternate pathways distinct from the main hypothesis that also lead from host factors to ARO infection should prompt consideration of these as putative confounders or mediators. Modeling the microbiome itself may require special techniques due to cyclic or nonlinear dynamics. ARO colonization here is modeled to be in the causal pathway between loss of colonization resistance and infection and, thus, it should be modeled as a mediator in multivariable analyses. However, colonization itself can lead to microbiome alterations, so this simplified framework may not apply in all scenarios. B, Here we see a specific putative causal inference diagram from hospital admission to ARO colonization. The direct pathway is shown in solid black and the indirect in solid gray. Antibiotic exposure and microbiome alterations are mediators, while medication expenses could serve as instrumental variables. Here confounders are depicted between antibiotic exposure and ARO colonization, but confounding can exist for each variable in the causal pathway and must be accounted for before formal mediation analysis can proceed.