Abstract
Background
Covid‐19 has caused many complications for both the infected and those in need of medical care. This may be due to infection‐related prognosis worsening or the patients’ avoidance of referring to the hospital for fear of contracting the infection. The decline of acute referral to the ER of many significant conditions with severe results on both the well‐being and life‐expectancy is a serious concern. To address these concerns, we designed this study to evaluate the recent pandemic's impact on “in‐hospital mortality” caused by neurological disorders pre and postpandemic.
Methods and material
The inclusion criteria were any acute neurological condition and the consent of the patients eligible for our study. The definitions of all assessed conditions and the comorbidities are ICD‐10 based. Hypertension and diabetes mellitus, due to their high prevalence, were evaluated separately from other internal comorbidities. The total number of the enrolled patients was 1742, 671 of whom had been during the COVID‐19 pandemic, and 1071 had attended the ER during the prepandemic era.
Results
The overall mortality was significantly higher during the pandemic, and the covid infected had suffered higher mortality rates. (p‐value < 0.05)
Conclusion
During the pandemic, those with minor strokes and other nonlife‐threatening ailments had avoided hospital care leading to a significantly higher rate of critical conditions. Increased incidence of strokes and ICHs during the pandemic, too, caused significant increased in‐hospital mortality.
Keywords: neurology, stroke
During the pandemic, those with minor strokes and other non‐life‐threatening ailments had avoided hospital care leading to a significantly higher rate of critical conditions. Increased incidence of strokes and ICHs during the pandemic, too, caused significant increased in‐hospital mortality.
1. INTRODUCTION
The recent covid‐19 pandemic led to many unexpected situations and resulted in the severe loss for the people. The pandemic scarred society's psyche in a lasting manner. Many have outlined these losses and evaluated the mental impact of the pandemic (Zandifar & Badrfam, 2020; Zandifar, Badrfam, Khonsari, Assareh, et al., 2020; Zandifar, Badrfam, Khonsari, Mohammadi, et al., 2020). However, with all focus on the covid‐19 pandemic, it has led to un‐diagnosing and missing some life‐threatening yet curable conditions.
Nonetheless, another theory is that the fear of the condition itself and the person's fear of acquiring the infection while visiting the hospital will lead to avoiding the hospital at all costs, losing precious treatment time, and dramatically worsening their prognosis. Thus after the pandemic, the number of referrals to the hospital markedly declined (Hartnett, 2020; Woodruff & Frakt, 2020; Zadnik et al., 2020; Whaley et al., 2020). This phenomenon has been addressed in other studies and includes emergency and outpatient visits (Borrelli et al., 2020; Wosik et al., 2020).
The decline in the usual numbers of referred patients to our hospital, the neurology referral center of an entire province, raised the question as to what had caused the patients decreased inflow. Since limited studies have evaluated the effect of the Covid‐19 pandemic and infection on neurological disorders, we designed this study to assess the impact of the COVID‐19 pandemic on “in‐hospital mortality” due to neurological disorders. In the Covid period, we evaluated covid infection's effect on all cause‐specific and stroke in‐hospital mortality.
2. METHODS AND MATERIALS
2.1. Data collection
In this before and after comparative study, Rajaee hospital's data was used as a referral center for all neurological conditions in Alborz province, Iran, to compare the effect of the covid‐19 pandemic on neurological diseases. All admission data from the March 20th till the end of June of 2019, the prepandemic period, and the similar months of 2020, and the postpandemic period were chosen.
Inclusion criteria were any neurological diagnosis and consent to use their data for research and publication purposes.
2.2. Neurological disorders and comorbidity definition and diagnosis
We obtained the data from the hospital's data files. All of the included diagnoses are ICD‐10 based.
In addition to conditions such as stroke and intracranial hemorrhages with high prevalence, for proper assessment and to provide an adequate population size for analysis, conditions such as tension headaches, migraine, non‐life‐threatening seizure episodes, multiple sclerosis flares, transient ischemic attacks, neuralgia, and non‐life‐threatening polyneuropathies were considered as “Other non‐life‐threatening conditions” (ONLT) ICD‐10 codes (H44.60, M54.81, G50.0, B02.22, G90.09, E11.40, G35, G45.9, G44.021, G44.89, G44.209, G43, G40, and G36).
Categorized as “other life‐threatening” (OLT) were conditions such as bacterial meningitis, encephalitis, Guillain barre syndrome, life‐threatening polyneuropathies, myelitis conditions, status epilepticus, and neurotoxins poisonings with ICD‐10 codes (G00.9, G04, G05, B00.4, G61.0, G40.901, G92, G37.4).
Internal conditions defined as rheumatologic disorders by ICD‐10 codes were as follows: (M05, L93) chronic pulmonary conditions ICD‐10 codes (J44.9, J45, j47), endocrine conditions ICD‐10 codes (E34.9, E24.9, E27.1, E03, E05, E22.1), chronic hepatic diseases ICD‐10 codes (K74.60, K70.3, K75.4, K73.9, B94.2, B18), and renal dysfunctions (N18, Q61.2).
Stroke was defined based on ICD‐10 codes: I63.X and I64.X and intracranial hemorrhage (in this study ICH was defined as all types of bleeding in cranium) as ICD‐10 codes: I60.X and I61.X.
Hypertension (HTN), defined as a consistently measured systolic blood pressure above 130 mm Hg or diastolic blood pressure above 80 mmHg, had an ICD‐10 code (I10).
ICD‐10 codes (E10, E11) defined diabetes mellitus as a fasting blood sugar above 126 mg/dl or blood glucose levels above 200 mg/dl at any time, or hemoglobin A1c level of 6.5% and higher.
Due to large numbers of hypertension and diabetes cases, for means of a better comparison, these conditions were grouped and analyzed separately from other internal disorders (World Health Organization, 2004).
2.3. Ethical consideration
The Ethics committee of Alborz University of Medical Sciences approved this study.
2.4. Statistical analysis
We analyzed the data using SPSS software version 22. The quantitative and qualitative variables are expressed as mean with SD and frequency with percentages. The mortality rates were reported with a 95% confidence interval (CI).
We used an independent t‐test to compare the quantitative and chi‐square tests to compare the qualitative variables. We assessed the effect of the covid era on in‐hospital mortality due to neurological disorders in different logistic regression models. Model I evaluates a crude association between the mentioned variables. In model II, the association adjusted the variables for sex and age, and in the third model, we modified any additional underlying conditions.
In the covid period, we assessed covid infection's effect on all cause‐specific and stroke in‐hospital mortality. The results of logistic regression analysis are reported as odds ratio (OR) and 95% CI. We considered a p‐value below 0.05 as statistically significant.
3. RESULTS
Overall, 1742 patients with neurological diseases participated in the study consisting of 1071 patients of the precovid era and 671 patients of the covid era. Demographic and disease‐related characteristics of patients during the covid period are presented in Table 1. The mean age of the patients for the two periods was not statistically different (p‐value: 0.24). Sex distribution before and in the covid era was statistically significant; the percentage of male patients with neurological diseases in the covid era has increased dramatically compared to female participants.
TABLE 1.
Demographic and disease‐related characteristics of patients according to covid‐19 period
| Before covid n = 1071 | After covid n = 671 | p‐value | ||
|---|---|---|---|---|
| Age | mean ± standard deviation | 61.42 ± 18.67 | 62.45 ± 17.23 | 0.24 |
| Sex | Male, n (%) | 563 (52.5) | 393 (58.5) | 0.01* |
| Female, n (%) | 508 (47.5) | 278 (41.5) | ||
| Mortality | Alive n (%) | 973 (90.8) | 550 (81.9) | <0.001* |
| Dead n (%) | 98 (9.2) | 121 (18.1) | ||
| Neurological condition | Stroke n (%) | 427 (39.9) | 301 (44.8) | <0.001* |
| ICH n (%) | 79 (7.3) | 92 (13.7) | ||
| OLT n (%) | 90 (8.4) | 51 (7.7) | ||
| ONLT n (%) | 475 (44.4) | 227 (33.8) | ||
| Underlying internal condition | Yes n (%) | 84 (7.8) | 99 (14.8) | <0.001* |
| No n (%) | 987 (92.2) | 572 (85.2) | ||
| Hypertension and diabetes | HTN n (%) | 172 (16) | 78 (11.6) | 0.001* |
| Diabetes n (%) | 31 (3.1) | 18 (2.6) | ||
| Both n (%) | 41 (3.8) | 50 (7.6) | ||
| None n (%) | 826 (77.1) | 525 (78.2) | ||
Abbrevations: ICH, intracranial hemorrhage; OLT, other life‐threatening; ONLT, another non‐life‐threatening; HTN, hypertension.
The mortality rate and having underlying internal condition nearly doubled significantly in the covid era.
The percentage of neurological conditions differed significantly between the two eras, as the percentage of strokes and ICHs were significantly higher within the covid era.
The chances of developing neurological conditions in patients with underlying internal conditions and those with a history of HTN and diabetes were significantly higher in the covid era.
Table 2 shows the effect of the Covid‐19 era on all‐cause‐specific neurological in‐hospital mortality rate in the logistic regression model. In the multivariate logistic regression model, the effect of the covid era on all‐cause neurological diseases mortality rate (OR: 1.95, 95%:1.42–2.68), strokes (OR: 2.23, 95%:1.42–3.5), and ICHs mortality rate (OR: 3.28, 95%:1.64–6.54) was statistically significant and mortality rate increase during the COVID‐19 era in comparison to the precovid era. However, the mortality rate of other non‐life‐threatening and life‐threatening conditions did not differ significantly.
TABLE 2.
Effect of the covid‐19 era on all and cause‐specific neurological in‐hospital mortality rate in logistic regression
| OR | 95% CI | p‐value | |||
|---|---|---|---|---|---|
| All‐cause neurological mortality | Model 1 | 2.18 | 1.64 | 2.9 | <0.001* |
| Model 2 | 2.23 | 1.66 | 3 | <0.001* | |
| Model 3 | 1.95 | 1.42 | 2.68 | <0.001* | |
| Stroke | Model 1 | 2.1 | 1.39 | 3.18 | <0.001* |
| Model 2 | 2.42 | 1.57 | 3.76 | <0.001* | |
| Model 3 | 2.23 | 1.42 | 3.5 | <0.001* | |
| ICH | Model 1 | 3.02 | 1.56 | 5.84 | <0.001* |
| Model 2 | 3.05 | 1.56 | 5.96 | <0.001* | |
| Model 3 | 3.28 | 1.64 | 6.54 | <0.001* | |
| OLT | Model 1 | 0.8 | 0.33 | 1.93 | 0.62 |
| Model 2 | 0.73 | 0.29 | 1.83 | 0.5 | |
| Model 3 | 0.83 | 0.31 | 2.25 | 0.72 | |
| ONLT | Model 1 | 0.89 | 0.33 | 2.35 | 0.82 |
| Model 2 | 0.87 | 0.32 | 2.35 | 0.79 | |
| Model 3 | 0.85 | 0.31 | 2.32 | 0.75 | |
Notes: Model 1 = crude.
Model 2 = adjusted for sex and age.
Model 3 = adjusted for all.
Abbrevations: ICH, intracranial hemorrhage; OLT, other life‐threatening; ONLT, other non‐life‐threatening; OR, odds ratio, 95%; CI, 95 % confidence interval.
Moreover, in the multivariate logistic regression model, COVID‐ 19 infection significantly increased the odds of all‐cause neurological mortality rate (OR: 3.75, 95%:2.22–6.35) and mortality rates due to stroke (OR: 2.49, 95%:1.19–5.21) (Table 3). Furthermore, mortality rates across neurological conditions are illustrated in Figure 1, illuminating the mortality percentage differences between the covid‐infected and noninfected patients across neurological conditions.
TABLE 3.
Effect of covid‐19 infection on all and stroke in‐hospital mortality during the covid‐19 era in logistic regression analysis
| OR | 95% CI | p‐value | |||
|---|---|---|---|---|---|
| All neurological diseases | Model 1 | 4.14 | 2.55 | 6.72 | <0.001* |
| Model 2 | 3.44 | 2.07 | 5.69 | <0.001* | |
| Model 3 | 3.75 | 2.22 | 6.35 | <0.001* | |
| Stroke | Model 1 | 2.69 | 1.34 | 5.38 | 0.005* |
| Model 2 | 2.46 | 1.18 | 5.14 | 0.01* | |
| Model 3 | 2.49 | 1.19 | 5.21 | 0.01* | |
Notes: Model 1 = crude.
Model 2 = adjusted for sex and age.
Model 3 = adjusted for all.
OR: odds ratio, 95% CI: 95 % confidence interval.
FIGURE 1.
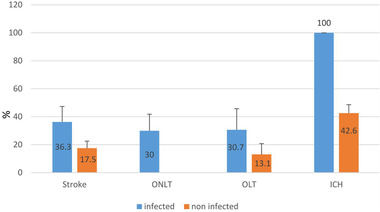
Effect of COVID‐19 infection on mortality rates according to neurological conditions alongside their standard error.
ICH: intracranial hemorrhage, OLT: other life‐threatening, ONLT: other non‐life‐threatening
4. DISCUSSION
Based on our results, it seems that the COVID‐19 pandemic may have led to an increase in some neurological conditions such as ICH by unknown means. Nevertheless, the critical point that needs attention is that these conditions lethality has increased during the covid era. A straightforward explanation can be COVID‐19 infection itself, as it has shown to increase significantly in‐hospital mortality; nonetheless, this cannot explain the main reason for mortalities within the covid era. As it is noticeable, the number of referrals in the covid period has nearly dropped to half compared to a similar timeline before the covid period. This might be due to fear of covid infection, causing avoidance of hospitals. As demonstrated in the results, the percentage of strokes and ICHs increased dramatically, while fear of covid contraction led to a decline in referral. According to our findings, patients with ONLT conditions or those with minor strokes and other non‐life‐threatening ailments avoided visiting hospitals, whereas patients with critical illnesses and more severe symptoms had no choice but to visit the hospital.
This refusal to seek care increased the percentage of critical patients, as shown in Table 1. The increased rate in strokes and ICHs and patients with coexistent internal diseases presumably being in a more critical situation than the similar timeline before the pandemic may have led to increased in‐hospital mortality.
Nonetheless, we must not forget another factor that people with a neurological condition avoiding hospitals and staying home lose valuable time, especially in ICH and strokes, thus dramatically increasing the condition's mortality. Hence, we think the fear alongside the infection has led to an increase in mortality.
5. STUDY LIMITATIONS
One should note that the most significant limitation of this study was that we only could assess in‐hospital mortality, and mortalities outside the hospital, including all those who did not visit the hospital or all those discharged from the hospital, could not be assessed; thus, we presume a significant underestimation of neurological diseases’ mortality. Therefore, it is imperative to educate the public of medical emergencies and when they must visit the hospital, despite being at risk of infection.
6. CONCLUSION
It seems health crises and pandemics can result in direct fatalities, as the general population avoids hospital visits, even for medical emergencies, resulting in death or irreparable damage that could have easily been avoided by a timely visit to the hospital. Thus we recommend public education on medical emergencies and teach them when they must visit the hospital and when it is better to avoid visits to the hospital.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Ethics Committee of Alborz University of Medical Sciences approved this study
AVAILABILITY OF DATA AND MATERIALS
The datasets generated and analyzed during the current study are not publicly available; however, the data can be shared for research and authentication purposes upon reasonable request.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
FUNDING
Alborz University of Medical Sciences funded this study.
AUTHORS CONTRIBUTIONS
MQ and NMK conceived the study, participated in study design, data collection, and data analysis. NAK, NMK, and AMF conceived the study, participated in data collection, and wrote the manuscript. SMPN participated in data collection and data analysis. NMK, SMPN, NAK, AM,F and MQ assisted with the preparation of the document and interpretation of the results. All the authors have read and approved the final submitted manuscript.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1002/brb3.2246.
Khoshsirat, N. A., Qorbani, M., Farivar, A. M., Mohammadpoor Nami, S., & Mohammadian Khonsari, N.. Effects of the covid‐19 pandemic on neurological diseases. Brain Behav 2021;11:e2246. 10.1002/brb3.2246
REFERENCES
- Borrelli, E., Grosso, D., Vella, G., Sacconi, R., Querques, L., Zucchiatti, I., Prascina, F., Bandello, F., & Querques, G. (2020). Impact of COVID‐19 on outpatient visits and intravitreal treatments in a referral retina unit: Let's be ready for a plausible “rebound effect. Graefe's Archive for Clinical and Experimental Ophthalmology, 258(12), 2655–2660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartnett, K. P. (2020). Impact of the COVID‐19 Pandemic on Emergency Department Visits—United States, January 1, 2019–May 30, 2020. MMWR Morbidity and Mortality Weekly Report (2020), 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whaley, C. M., Pera, M. F., Cantor, J., Chang, J., Velasco, J., Hagg, H. K., Sood, N., & Bravata, D. M. (2020). Changes in health services use among commercially insured us populations during the COVID‐19 pandemic. JAMA Network Open, 3(11), e2024984‐e. 10.1001/jamanetworkopen.2020.24984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodruff, A., & Frakt, A. B. (2020). COVID‐19 pandemic leads to decrease in emergency department wait times. JAMA Health Forum, 1(9). 10.1001/jamahealthforum.2020.1172 [DOI] [PubMed] [Google Scholar]
- World Health O (2004). ICD‐10: International statistical classification of diseases and related health problems: Tenth revision. 2nd edn. World Health Organization. [PubMed] [Google Scholar]
- Wosik, J., Clowse, M. E. B., Overton, R., Adagarla, B., Economou‐Zavlanos, N., Cavalier, J., Henao, R., Piccini, J. P., Thomas, L., Pencina, M. J., & Pagidipati, N. J. (2020). impact of the COVID‐19 pandemic on patterns of outpatient cardiovascular care. American Heart Journal, 231, 1–5. 10.1016/j.ahj.2020.10.074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zadnik, V., Mihor, A., Tomsic, S., Zagar, T., Bric, N., Lokar, K., & Oblak, I. (2020). Impact of COVID‐19 on cancer diagnosis and management in Slovenia–preliminary results. Radiology and Oncology, 54(3), 329–334. 10.2478/raon-2020-0048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandifar, A., & Badrfam, R. (2020). Iranian mental health during the COVID‐19 epidemic. Asian Journal of Psychiatry, 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandifar, A., Badrfam, R., Khonsari, N. M., Assareh, M., Karim, H., Azimzadeh, M., Noori Sepehr, M., Tajbakhsh, R., Rahimi, F., Ghanipour, N., Agoushi, A., Hassani Gelsefid, S., Etemadi, F., & Qorbani, M. (2020). COVID‐19, and medical staff's mental health in educational hospitals in Alborz Province, Iran. Psychiatry and Clinical Neurosciences, 74(9), 499–501. 10.1111/pcn.13098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandifar, A., Badrfam, R., Khonsari, N. M., Mohammadi, M. R., Asayesh, H., & Qorbani, M. (2020). Prevalence and associated factors of posttraumatic stress symptoms and stigma among health care workers in contact with COVID‐19 patients. Iranian Journal of Psychiatry, 15(4), 355–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are not publicly available; however, the data can be shared for research and authentication purposes upon reasonable request.


