Graphical Abstract
Graphical Abstract.
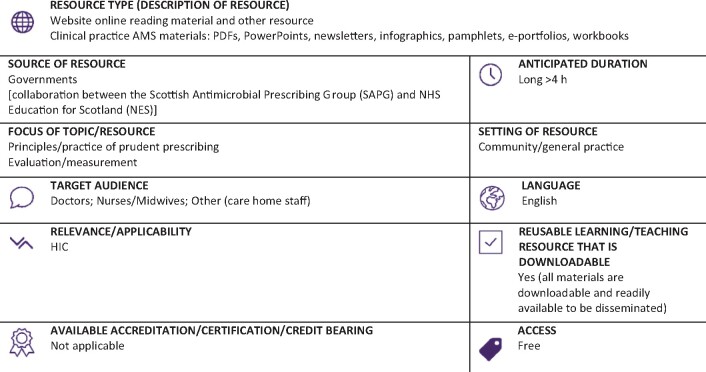
LI, low-income countries; LMIC, low- and middle-income countries; HMI, high- and middle-income countries; HIC, high-income countries.
Resource web link: https://www.nes.scot.nhs.uk/education-and-training/by-theme-initiative/healthcare-associated-infections/training-resources/scottish-reduction-in-antimicrobial-prescribing-(scrap).aspx (Full classification scheme available at: http://bsac.org.uk/wp-content/uploads/2019/03/Educational-resource-review-classification-scheme.pdf)
WHO region and country (World Bank): Europe, UK (HIC)
Peer review commentary
The Scottish Reduction in Antimicrobial Prescribing (ScRAP) programme is an educational toolkit that aims to support initiatives to reduce unnecessary antibiotic prescribing in primary care. The present version was updated in 2016–17. It is designed to be used by GP practices but can also be used by other relevant stakeholders in the management of infection in the community. The core materials are PowerPoint slide sets with facilitator notes that are meant to support facilitated learning sessions. There are six slide sets that can be divided in four groups: Antimicrobial resistance and Healthcare Associated Infection; Public understanding and expectations; Targeting prescribing for respiratory tract infections; and Managing urinary tract infections (three parts). A support pack is available and provides detailed information about the objectives and insights on how to deliver the content. The slide sets are well constructed and provide unbiased and accurate information. A question and answer approach was used and that strategy makes the materials more engaging. Each slide set was designed to be used in 30 to 60 min learning sessions. Additional materials such as leaflets, audit tools, decision support tools and links for other resources are also available.
The programme focuses on respiratory tract and urinary infections, two of the main causes of prescription of antibiotics in the community setting and which deserve attention in most countries. The questions raised and principles promoted can be easily adapted for other countries and only some of the data used for context are specific for Scotland. Addition of other areas of frequent antibiotic prescribing in the community could enrich this programme even more. Overall this is a very interesting educational resource, with clear messages and objectives and robust content. The adaptability and ease of use of this content to disseminate good practice are in my view the two major strengths. It deserves a careful look from everyone interested in improving the quality of antibiotic prescription in the community setting.