Abstract
Background:
Mental health conditions impose a major burden worldwide, especially in low- and middle-income countries (LMICs), where health specialists are scarce. A challenge to closing LMICs’ mental health treatment gap is determining the most cost-effective task-shifting pathway for delivering mental health services using evidence-based interventions (EBIs). This article discusses the protocol for the first study implementing comprehensive mental health services in LMICs.
Methods:
In partnership with the Mozambican Ministry of Health, this cluster-randomized, hybrid implementation effectiveness type-2 trial will evaluate implementation, patient, and service outcomes of three task-shifting delivery pathways in 20 Mozambican districts (population 4.7 million). In pathway 1 (usual care), community health workers (CHWs) and primary care providers (PCPs) refer patients to district-level mental health clinics. In pathway 2 (screen, refer, and treat), CHWs screen and refer patients to PCPs for behavioral and pharmacological EBIs in community clinics. In pathway 3 (community mental health stepped care), CHWs screen patients and deliver behavioral EBIs in the community and refer medication management cases to PCPs in clinics. Mixed-methods process evaluation will be used to examine factors affecting pathway implementation, adoption, and sustainability. Clinical activities will occur without research team support. Ministry of Health personnel will coordinate training and supervision.
Results:
The most cost-effective pathway will be scaled up in all districts for 12 months.
Next steps:
This novel study integrating comprehensive mental health services into primary care will inform a toolkit to help the Mozambican Ministry of Health scale up the most cost-effective pathway for mental health services and can be a template for other LMICs.
An effective national planning and programming strategy to implement comprehensive evidence-based mental health services must address common mental disorders, severe mental disorders, substance use disorders, and suicide risk and identify optimal delivery strategies (1). This is especially important in low- and middle-income countries (LMICs), where prudent allocation of scarce resources is fundamental. Because LMICs often do not have the capacity to deliver mental health services through a specialized workforce, research has recommended task-shifting, the rational and supervised redistribution of tasks between specialists and nonspecialists, integrated into primary and community care (2). Similar to support for models of integrating depression treatment into primary care in high-income countries (e.g., collaborative care model) (3), evidence has documented that trained lay personnel such as teachers and community health workers (CHWs) in LMICs can recognize mental disorders (4) and effectively deliver psychotherapeutic treatments (5–9) and that trained and supervised primary care providers (PCPs) can effectively deliver psychopharmacological treatments (8). Finally, human resource shortages can be addressed by using stepped-care approaches (10) in which first-line treatment is low intensity, cost effective, time efficient (i.e., short-term evidence-based interventions [EBIs]), and conducted by CHWs, whereas more complex cases require “stepping up” care delivered by PCPs or mental health specialists, as appropriate (11). Given the shortages and cost of specialized mental health personnel in LMICs (12), innovatively adapting EBIs to be delivered by existing non–mental health personnel (i.e., CHWs and PCPs) through task-shifting can help narrow the mental health treatment gap (13), which is defined as the difference between the number of individuals with a disorder and the proportion of individuals affected by the disorder who receive treatment (14).
Most mental health trials conducted in LMICs and high-income countries have focused on testing the treatment of a single condition (e.g., depression) (15–19) or a combination of a few conditions (e.g., transdiagnostic) (20). However, public health systems must cover all mental health diagnoses, often in combination. Studying implementation and scale-up of comprehensive mental health services that simultaneously address common and severe mental disorders, substance use disorder, and suicide risk in LMICs can generate needed information for policy makers to provide multidimensional care in low-resource settings. To our knowledge, this is the first study to examine implementing such comprehensive mental health services.
Mozambique is the fourth poorest country in the world (21), with over 70% of the population living in rural areas with no or limited access to mental health care (22, 23). Mental and substance use disorders are the leading causes of years lived with disability (24, 25). Yet, resources to treat mental disorders are insufficient. Only 391 mental health professionals (18 psychiatrists, 109 psychologists, 264 midlevel health professionals) serve over 29 million inhabitants. About 75% of people with mental disorders receive no care (26).
Mozambique is committed to transforming its mental health system, which requires new policies from the Ministry of Health to scale up government-funded comprehensive community mental health services (27). As in other LMICs, the usual mental health delivery in Mozambique depends on one specialty clinic per district. These urban, district-level clinics are staffed by psychiatric technicians (PsyTs), midlevel health professionals trained in a 30-month program to deliver mental health services and epilepsy care who are supervised by mental health specialists (psychiatrists and psychologists), with limited community outreach (28). Thus, a majority of people with psychiatric disorders are not served because of scarcity and geographic distribution of providers. Motivated by the burden of neuropsychiatric disorders, the Ministry of Health recently implemented a program, funded by the World Health Organization (WHO) to provide task-shifted care for epilepsy within the public health system (29). These efforts demonstrate the readiness of the system to expand its focus to all mental disorders.
The Partnerships in Research to Implement and Disseminate Sustainable and Scalable Evidence-Based Practices in Sub-Saharan Africa—Mozambique (PRIDE SSA–Mozambique) protocol was designed in partnership with the Mozambican Ministry of Health to ensure that interventions, training, and supervision systems are sustainable and consistent with human resources and local treatment guidelines. This three-arm, longitudinal scale-up study uses a mixed-methods, hybrid type-2 effectiveness-implementation design (30) in 20 districts of Mozambique. It aims to compare the effectiveness of implementing comprehensive mental health care at the primary care and community levels with the effectiveness of usual care (pathway 1), in which CHWs and PCPs refer all suspected cases to mental health specialists at district-level mental health clinics. The treatments will be interpersonal counseling (31, 32) for common disorders; motivational interviewing (33–36) for substance use disorders; the suicide safety planning intervention (37) for suicide risk; and psychiatric medication for severe disorders, which only mental health specialists could prescribe prior to our study. The two experimental delivery pathways harness existing human resources, including 696 CHWs, supervised by 181 PCPs (approximately two per community clinic) responsible for primary care needs, and 18 PsyTs in specialty district clinics, comprising a catchment area with a patient population of 4.7 million (Table 1). Although CHWs receive less training than PCPs, they have a wider reach and closer connection to the community. PCPs and CHWs have competing demands. In pathway 2 (screen, refer, and treat), CHWs screen and refer all identified patients to PCPs for pharmacological and nonpharmacological EBIs in community clinics. In pathway 3 (community mental health stepped care), CHWs and PCPs screen patients, and, as needed, CHWs deliver behavioral EBIs in the community while PCPs deliver psychopharmacological treatment in the clinic. Studying these three delivery pathways using mixed-methods process evaluation will help identify the most effective pathway for the Mozambican system of care and inform subsequent scale-up efforts.
TABLE 1.
Overview of pathways for delivering comprehensive mental health services in the PRIDE SSA–Mozambique Scale-Up Studya
| Pathway | Community (CHWs, N=696) | Community clinic (PCPs, N=181) | District mental health clinic (PsyTs, N=18) |
|---|---|---|---|
| 1. Usual care: district-level care | Refer patients with suspected mental disorder to district mental health clinic | Refer patients with suspected mental disorder to district mental health clinic | Provide all mental health services |
| 2. Screen, refer, and treat: clinic-level care | Screen and refer identified patients to community clinic | Screen and deliver nonpharmacological EBIs and psychopharmacology | Supervise and manage patients with complex cases |
| 3. Community mental health care: community- and clinic-level care | Screen, deliver nonpharmacological EBIs, and refer to community clinic for psychopharmacology | Screen and deliver psychopharmacology | Supervise and manage patients with complex cases |
CHW, community health worker; EBI, evidence-based intervention; N, proposed number of provider type; PCP, primary care provider; PRIDE SSA–Mozambique, Partnerships in Research to Implement and Disseminate Sustainable and Scalable Evidence-Based Practices in Sub-Saharan Africa—Mozambique; PsyT, psychiatric technician.
With this research, we aim to produce generalizable knowledge about how best to scale up comprehensive mental health services in LMICs. Box 1 highlights the key challenges and advantages of the study setting as well as design solutions to be implemented and evaluated.
BOX 1. Key challenges, advantages, and design solutions of PRIDE SSA–Mozambiquea.
Challenges
Limited specialized mental health workforce, available only in urban areas (district level)
Limited training of primary care providers to recognize and treat mental illness; prescribing of psychiatric medications is limited to mental health specialists
Very limited financial resources to increase mental health services
Limited training and supervision resources to support fidelity to evidence-based interventions used by nonspecialists
Untested implementation strategies
Ensuring sustainability of mental health services
Caseload capacity of primary care clinic personnel to accept new practices and patients
Advantages
A committed Ministry of Health involved in capacity building and implementation science research
Task-shifting strategic policy already in place; psychiatric technicians, supervised by mental health specialists, provide mental health services in urban areas
Successful implementation of the WHO-funded epilepsy program that trained community health workers and primary care providers to recognize and treat epilepsy, respectively
A strong and productive partnership between researchers and the Ministry of Health that trained local experts and trainers and developed an innovative and efficient screening tool for all mental disorders
Design Solutions
Expand current mental health task-shifting strategy by developing sustainable training supervision systems for community health workers and nonurban clinics’ primary care providers and another Mozambican task-shifting workforce comprising medicine technicians and nurses in order to provide comprehensive mental health services to detect and manage common and severe mental disorders, substance use disorders, and suicide risk.
Use mobile health technologies for nonspecialist training and supervision to screen and triage patients and to provide evidence-based treatments.
Measure effectiveness of two fully task-shifted implementation strategies at the patient, provider, clinic, system, and implementation levels.
Research budget funds only the initial training of providers, not implementation and supervision of clinical services, to ensure sustainability of implementation strategies.
a PRIDE SSA–Mozambique, Partnerships in Research to Implement and Disseminate Sustainable and Scalable Evidence-Based Practices in Sub-Saharan Africa; WHO, World Health Organization.
We will test whether one of the three delivery pathways is superior on the basis of implementation, patient, and service outcomes, reflecting each of the levels of Proctor’s implementation framework (38, 39) (Figure 1). The framework denotes these three distinct yet interrelated outcomes, acknowledging the multilevel nature of the implementation process required to address overall system-level impact.
FIGURE 1. PRIDE SSA–Mozambique implementation-, service-, and patient-level outcomes, and mediators/moderators across levelsa.
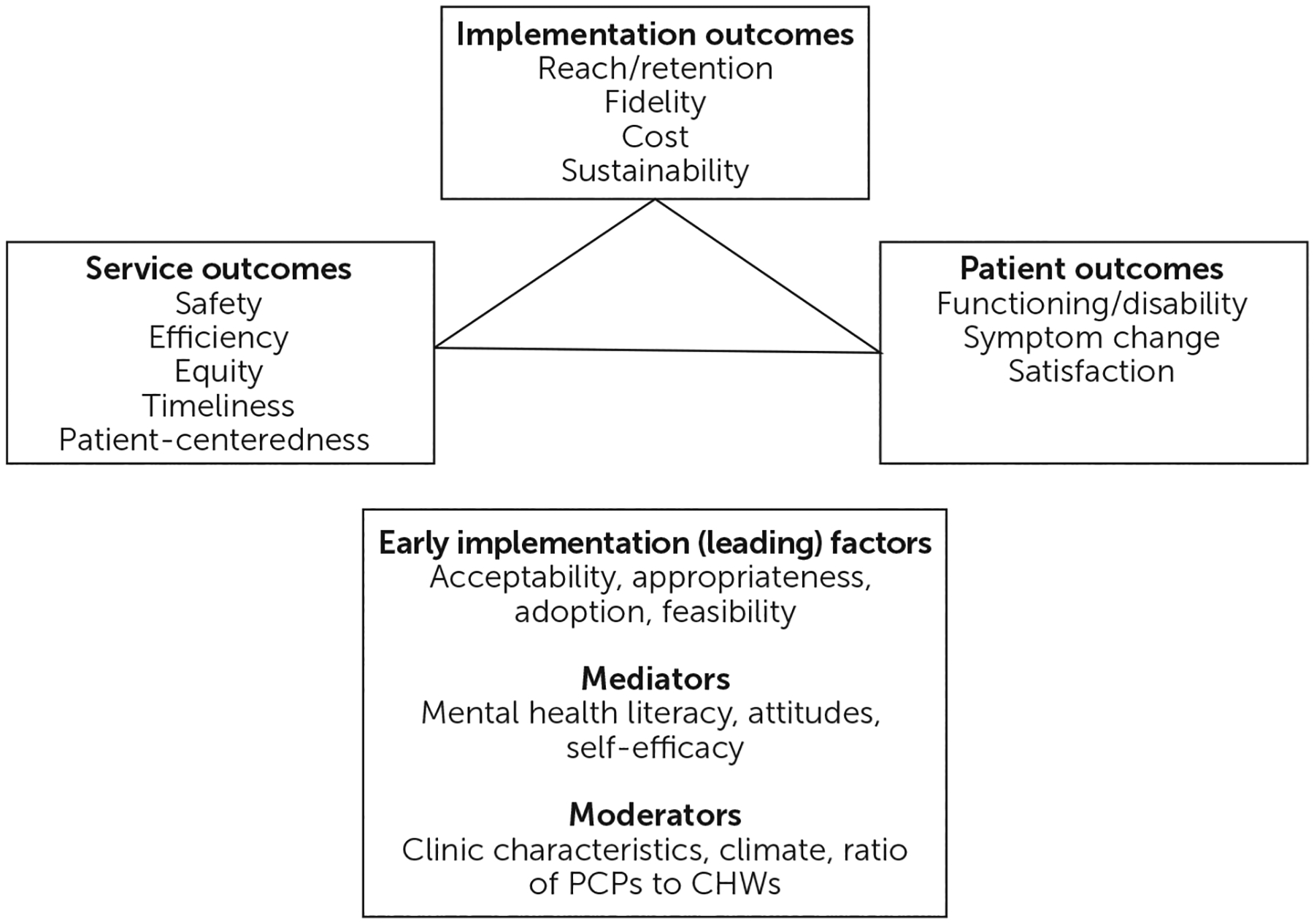
a Source: Adapted from Proctor et al. (39). CHW, community health worker; PCP, primary care provider; PRIDE SSA–Mozambique, Partnerships in Research to Implement and Disseminate Sustainable and Scalable Evidence-Based Practices in Sub-Saharan Africa—Mozambique.
Our three hypotheses are as follows. Hypothesis 1 (implementation) is that districts assigned to pathway 3 (community mental health care) will achieve greater mental health service reach and retention than those assigned to pathway 2 (screen, refer, and treat), which will, in turn, have greater reach and retention than those assigned to pathway 1 (usual care). Furthermore, we hypothesize that districts in pathways 2 and 3 will have similar but higher implementation costs than districts assigned to pathway 1. Hypothesis 2 (services) is that districts assigned to pathway 3 will have better service outcomes than will districts assigned to pathways 1 and 2. Hypothesis 3 (patient outcomes) is that districts assigned to pathway 3 will have better patient outcomes than will those assigned to pathways 1 and 2.
METHODS
Overview
We will conduct a two-phase (phase 1, implementation; phase 2, sustainability), 2-year, three-arm, cluster-randomized, hybrid effectiveness-implementation, type-2 trial in Mozambique (40). To prevent contamination, cluster randomization will occur at the district level; all clinics and providers in the same district participate in only one of the three delivery pathways. Random assignment of districts will be at a 1:2:2 ratio, with four districts in pathway 1 and eight each in pathways 2 and 3. Random assignment will be stratified on the basis of district size (i.e., number of CHWs) to ensure balance. The study will determine the most cost-effective delivery pathway in terms of implementation outcomes (reach, retention, cost), service-level outcomes (efficiency, timeliness, equity), and patient-level outcomes (symptoms, functioning, satisfaction). The delivery pathway showing the highest overall cost-effectiveness will then be implemented in all districts during a scale-up phase. Throughout the trial and the scale-up phase, a rigorous, mixed-methods process evaluation will be used to examine implementation, sustainability, and scale-up parameters.
Partnership Development and Training of Trainers
Since 2014, a U.S.-Mozambique-Brazil mental health implementation science capacity-building program funded by the Fogarty International Center and the National Institute of Mental Health (NIMH) (D43-TW009675) (41) has trained local psychologists and psychiatrists in strategies to scale up interventions for neuropsychiatric disorders and in training other trainers to deliver EBIs. Semiannual in-person seminars and weekly online supervision qualified 25 Mozambican mental health specialists to be trainers and supervisors in interpersonal counseling, motivational interviewing, suicide safety planning intervention, and neuropsychiatric medication management. To promote sustainability, this cadre of local trainers will conduct all study training and supervision activities, including training of PsyTs as supervisors and trainers.
Study Sites
The study will be conducted in two provinces in Mozambique. Nampula is the northernmost and most populous province in the country (population 5.76 million) and contains both vast rural areas and the third-largest city in the country. Sofala (population 2.22 million) is in the central region and is the site of several recent devastating cyclones (42–44). Research will be conducted across 20 districts, comprising approximately 60% of the population, in the two provinces (4.79 million individuals). Every district contains clinics with varying degrees of urbanicity (rural, semiurban, and urban). Currently, mental health services are provided only at mental health specialty clinics by one or two PsyTs per district and between one and five mental health specialists (psychiatrists or psychologists) per province. Each district has about seven primary care clinics (range 2–17), each with between two and five PCPs (nurses, preventive medicine technicians, and medical technicians). CHWs, approximately five per clinic (range 3–12) depending on the catchment area population, visit 250–400 households in their community at least once per year, depending on the family’s health needs. CHWs focus on infectious disease (HIV, tuberculosis, malaria) testing and treatment as well as maternal-child health services. Neither PCPs nor CHWs are trained or certified to provide mental health services; some PCPs are trained to treat epilepsy as part of the ministry’s previous task-shifting effort.
Study Phases and Procedures
The first phase of the trial is devoted to implementation, in which staff are trained according to the assigned pathway (Table 1). Specifically, all staff in pathways 2 and 3 will be trained to use a brief comprehensive, tablet-based mental disorders assessment tool, the Electronic Mental Wellness Tool (e-mwTool) (45, 46), which screens for and identifies the presence of common disorders (e.g., depression, anxiety), substance use disorders, severe disorders (e.g., psychosis, mania), and acute suicide risk. CHWs will administer the e-mwTool to screen every household in their catchment area during annual visits. PCPs and PsyTs will administer the e-mwTool to screen all patients in their care and at every clinical encounter thereafter. In pathways 2 and 3 (Table 1), CHWs and PCPs tasked with carrying out treatment will be trained to provide care on the basis of results of the screen and will be supervised by their district PsyT. Training certification for each EBI will comprise didactics, role-plays, case discussions, and successful completion of three supervised individual cases, followed by ongoing weekly group supervision. Supervisors will be trained PsyTs and mental health specialists during the initial 1-year implementation phase and then PsyTs only during the 1-year sustainability phase. Competency and sustainability of pathway delivery and outcomes will be measured during the sustainability phase. To preserve current usual care procedures as much as possible, pathway 1 staff will administer the e-mwTool for data collection purposes only. Although the tool will not provide them with any information or guidance, it will record their conduct. These implementation and sustainability phases occur within the context of the cluster-randomized trial. At the end of these 2 years, the more effective condition (based on clinical and cost outcomes) will then be implemented in districts that received the less effective condition for 12 more months, during the scale-up phase.
Outcome Measures
Pathway effectiveness will be determined by measuring implementation, service, and patient outcomes (39) (Figure 1). Table 2 outlines the specific measures and the timing of data collection to evaluate the performance of the three delivery pathways at each of these outcome levels. Measures were selected and/or developed through collaboration and formative work with local stakeholders involved in the capacity-building grant funded by the Fogarty International Center and NIMH (41). All measures (47–57) (Table 2) were culturally adapted, translated, and back-translated according to WHO-recommended procedures. As in the process evaluation, the Consolidated Framework for Implementation Research (CFIR) (58, 59) will be used to guide qualitative data collection on outcomes.
TABLE 2.
Outcomes and measures for mixed-methods data collection
| Measure | Description | Administered by | Respondenta |
|---|---|---|---|
| Patient outcomes | |||
| Symptom improvement since last visitb | 1 yes/no item | Provider | Patient |
| Electronic Mental Wellness Tool (e-mwTool)b (45, 46) | 3 items to screen for any mental disorder; 9 items for diagnostic categorization | Provider | Patient |
| 12-item Short-Form Health Surveyb (48) | 12 items measuring health-related quality of life | Provider | Patient |
| Satisfaction with mental health servicesc | Qualitative assessment | Researcher | Other |
| Service outcomes | |||
| Safety of patient and providersd | Qualitative assessment; provider and supervisor structured chart notes | Researcher | Provider, other |
| Equitable distribution of servicesc | Associations between household demographic inventory and rates of reach and retention | Provider | Patient |
| Patient-centerednessd | Qualitative assessment | Researcher | Patient, other |
| Efficiency and timelinessb | Efficiency of reach is time between screening(s) and initial treatment; efficiency of retention is time between initial treatment, follow-up treatment, and subsequent follow-ups, if treatment is indicated by guidelines in Mozambique | Provider | Patient |
| Implementation outcomes | |||
| Training | Percentage of attendance and completion, process of trainer and supervisor selection, knowledge, and fidelity to the intervention via technology-assisted methods and supervision | Researcher | Provider |
| Reach/retentionc | Reach is percentage of individuals screened positive by the e-mwTool that enter treatment; retention is percentage of completed courses of treatment for those who entered care | Provider | Patient |
| Pathway fidelitye | Percentage of individuals screened positive and referred to appropriate treatment and provider | Provider | Patient |
| Cost/resources needede | Stages of Implementation Completion Scale (SIC): 8 stages across preimplementation, implementation, and sustainability phases (49); Cost of Implementing New Strategies (50): maps implementation resources with SIC | Researcher | Provider |
| Sustainabilityd | The Program Sustainability Assessment Tool (51, 52) 40-item scale evaluates 8 dimensions essential for long-term program sustainability: environmental support, funding stability, communications, strategic planning, partnerships, program adaptation, program evaluation, and organizational capacity; mixed-methods process evaluation | Researcher | Provider |
| Mediators and moderatorsd | |||
| Knowledge | Mental health literacy (53) | Researcher | Provider |
| Self-efficacy | 10-item Work Self-Efficacy Scale (54, 55) | Researcher | Provider |
| Clinic characteristics | Rural, semiurban, urban; ratio of PCPs to CHWs | Researcher | Provider |
| Attitude toward adoption | 15-item Evidence-Based Practice Attitudes Scale (56) | Researcher | Provider |
| Organizational readiness for change | 9-item Ready Set Change (57) | Researcher | Provider |
Other indicates a subsample of the study population including community leaders, policy makers, providers, patients, and relatives.
Collected at every patient contact; de-identified aggregate every 6 months.
De-identified aggregate every 6 months.
Baseline and every 6 months.
Recorded as completed.
The main patient and implementation outcome measure, the e-mwTool (45, 46), is a 12-item instrument that can be administered by lay workers to comprehensively assess psychiatric disorders for provision of task-shifted mental health care and to classify patients into four treatment categories: common mental disorders, severe mental disorders, substance use disorders, and suicide risk. The e-mwTool development sample included 911 participants in Maputo. From the 99-item battery administered, 12 items were selected on the basis of clinical expertise and statistical rigor. The e-mwTool validation in Nampula performed well in identifying any mental disorder among 480 participants by using three items (0.94 sensitivity) and in classifying patients into treatment categories by using nine additional items (0.63–0.93 specificity). Quantitative patient outcome data and provider-level implementation measures (e.g., mediators and moderators) will be collected by using a tablet-based Research Electronic Data Capture (REDCap) tool (60, 61). Data will be hosted within the Ministry of Health; de-identified data will be available to all research partners for analysis.
Treatments
Based on the e-mwTool screen results, patients will be classified into one or more of the following treatment categories: severe, common, or substance use disorder and suicide risk (Figure 2). A tablet-based medication diagnostic algorithm will be used to provide patients who have severe disorders with psychopharmacological treatment according to specific psychiatric diagnoses, based on WHO Mental Health Gap Action Programme guidelines (62). Patients with common disorders will receive interpersonal counseling (31, 63), a briefer (four sessions) and more structured version of interpersonal therapy (32) designed for nonspecialist settings that focuses on the relation between interpersonal problems (i.e., disputes, life changes, grief, and social isolation) and the onset of psychiatric symptoms. For treatment of patients with substance use disorders, staff will use motivational interviewing (33–36), a brief (four sessions) therapeutic approach that uses active empathetic listening to explore patients’ goals, resolve ambivalence, and elicit motivation to change a behavior. Patients with acute suicide risk will develop a suicide safety plan (37) that includes a personalized set of coping strategies and sources of support to utilize during a suicidal crisis when hospitalization is not clinically indicated. All treatments have mobile applications that guide facilitators on treatment steps and allow remote monitoring of both pathway and treatment fidelity. The latter will be complemented through weekly clinical supervision of CHWs by PCPs and monthly supervision of both CHWs and PCPs by PsyTs. PsyTs supervise all clinical activities within each district. Patients with complex issues requiring hospitalization (e.g., severe disorders with suicide risk) will be transferred for inpatient care at the district hospital.
FIGURE 2. Population-based screening, identification, treatment, and follow-up within the PRIDE SSA–Mozambique system of carea.
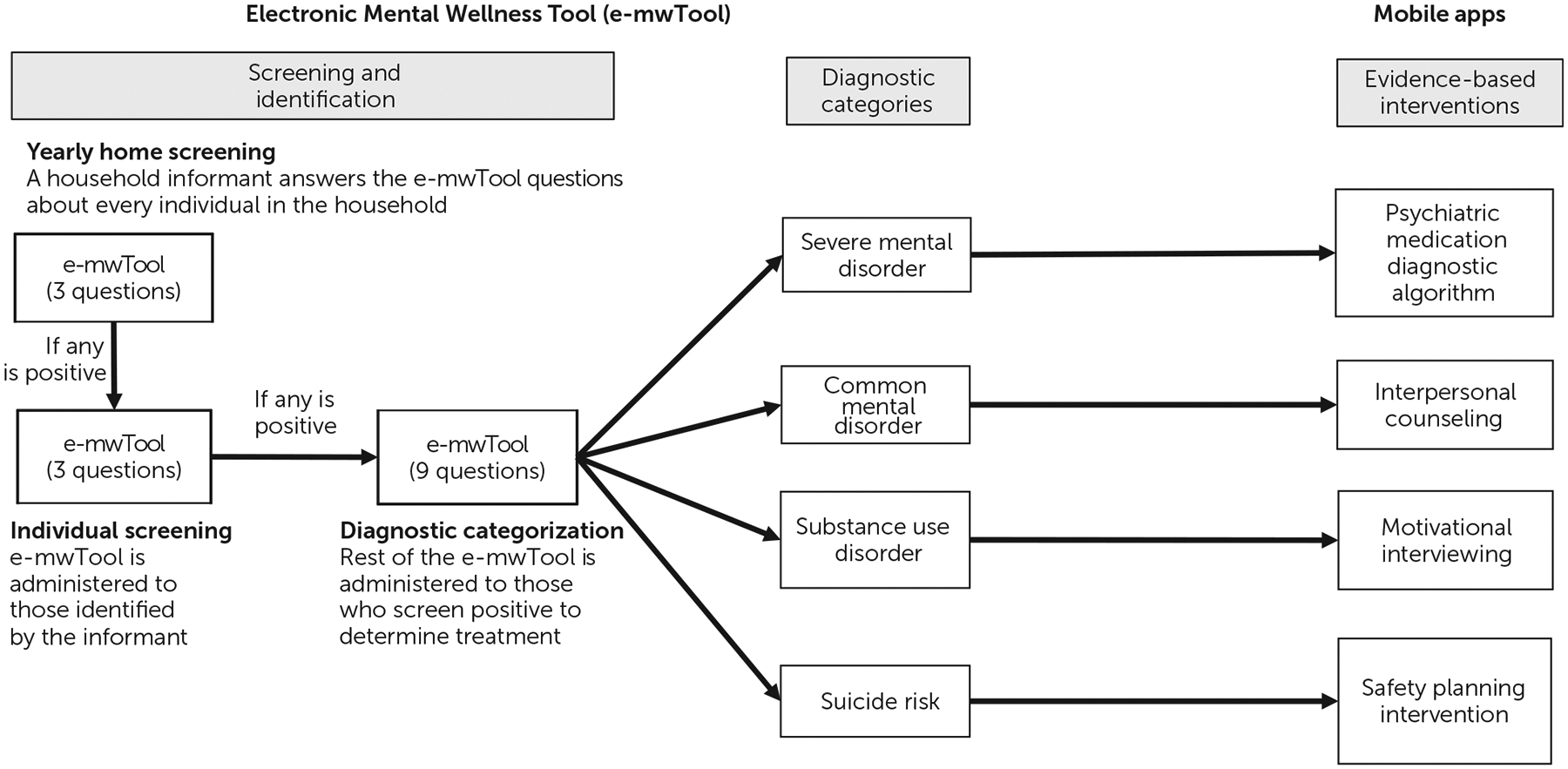
a PRIDE SSA–Mozambique, Partnerships in Research to Implement and Disseminate Sustainable and Scalable Evidence-Based Practices in Sub-Saharan Africa—Mozambique.
Interpersonal counseling, motivational interviewing, and the suicide safety planning intervention will be delivered individually for 4 weeks. At the end of these 4 weeks, patients will again be administered the e-mwTool. Those who continue to screen positive for common or substance use disorders will enter a group EBI (i.e., group interpersonal therapy [64] and motivational interviewing [65]). People with continued suicide risk will be referred to the PCP for evaluation and consultation with a mental health specialist supervisor. Those who screen positive for a new mental health condition will enter the corresponding individual treatment. Those whose assessment shows full or partial remission will be reassessed in 1 month and either discharged or referred for further care. If the findings from the initial assessment determine the presence of both common mental and substance use disorders, the EBI to be administered first will be based on symptom severity and/or patient-choice. After completion of the first EBI, patients will be assessed with the e-mwTool, and treatment will be administered according to current results.
Mixed-Methods Process Evaluation
A mixed-methods process evaluation will include quantitative patient outcome data collected during clinical activities by pathway providers as well as provider-level implementation measures (e.g., mediators and moderators) to be completed by providers at baseline and every 6 months. Qualitative data collection will be conducted in a purposive sample of six clinics (50% rural, 50% semiurban) per pathway for a total of 18 clinics. Annual data collection will include three focus groups with district-level community leaders and policy makers, 18 focus groups with health providers (one per clinic), and 36 household interviews with patients and/or their family members (two per clinic). Each focus group will include between six and eight participants; household interviews will be held with between one and four individuals from each family unit. All participants will provide written informed consent prior to participation in the qualitative portion of the study. All sessions will be audiotaped, transcribed, and uploaded into an NVivo data file for analysis. The CFIR (58) will guide our qualitative exploration of the implementation process with five domains (59): intervention characteristics (i.e., features of an intervention), outer setting (i.e., economic, political, and social context), inner setting (i.e., organizational setting), characteristics of individuals involved in implementation, and the implementation process. Interviews and focus groups will explore the underlying mechanisms of impact on and barriers and facilitators to implementation and sustainability across settings and the ways in which contextual factors influence outcomes.
Analytic Strategy
The effect of each delivery pathway on continuous outcome variables will be assessed by using longitudinal, nested random-effects linear models. The dependent variables for these models will include implementation, patient, and service outcomes (Table 2). The independent variables will be the delivery arm, time, and the interaction between them. The model will include a random effect for districts to account for nesting of providers within districts. The magnitude and statistical significance of the beta coefficient for the interaction will assess the extent to which the change in outcomes over time differs by study condition. In the event that descriptive analyses identify any baseline differences between study groups after randomization, covariates will be considered to adjust for these differences.
Incremental cost-effectiveness ratios will be constructed for the pairwise comparison of study arms (i.e., pathway 3 vs. pathway 1, pathway 2 vs. pathway 1, pathway 3 vs. pathway 2). The cost-effectiveness ratio’s numerator is the difference in mean costs for the study arms determined by the Stages of Implementation Completion (49) and Cost of Implementing New Strategies (50); the denominator is the difference between the study arms in a quantifiable measure of outcome. The primary implementation outcome is reach. The cost-effectiveness ratio for reach will quantify cost or savings of increasing the reach score by one unit in the higher performing pathway. Cost-effectiveness acceptability curves will be constructed to account for uncertainty in generalizing study results to the general population. This approach will provide the information needed to determine whether gains in reach are sufficient to justify marginal costs. In a similar manner, cost-effectiveness ratios can be constructed for other outcomes of the study (i.e., other aforementioned implementation, service, and patient outcomes) where the data demonstrate significant improvement in the outcome in one delivery pathway compared with the others.
Qualitative data analysis will be guided by grounded theory, which provides a rigorous, systematic approach to collecting and analyzing qualitative data and produces robust theoretical models of social behavior in health care settings (66). This approach uses an inductive process of iterative coding to identify recurrent themes, categories, and relationships in qualitative data. We will develop a comprehensive coding scheme based on this analysis and apply it to the data to produce a fine-grained descriptive analysis of the role of organizational and leader-level characteristics on implementation. Using the NVivo qualitative data analysis software, we will then separately code a sample of the transcripts and compare their application of the coding scheme to assess its reliability and robustness. Any disagreements in coding will be resolved through discussion.
In the process evaluation mixed-methods analyses, we will triangulate quantitative and qualitative data to better understand contextual factors that influence patient, service, and implementation outcomes across diverse districts (67–69). We will use a sequential taxonomy in which the quantitative data will be gathered prior to qualitative data, and we will weigh them equally (QUAN→QUAL) (70, 71). The function of the qualitative data is of complementarity, to understand the process of implementation as experienced by stakeholders through a connecting process wherein the qualitative data set builds upon the quantitative data set (70). To explore potential mechanisms underlying the effectiveness of different service delivery pathways, quantitative measures of the characteristics of the intervention target (e.g., provider work self-efficacy, mental health literacy, clinic urbanicity) will be included as mediators and/or moderators in models assessing implementation, service, and patient outcomes. An exploratory analysis will examine whether contextual variables, such as the size and type of organization and organizational climate, contribute to variation in implementation success related to specific delivery pathways.
RESULTS
Of the over 4.7 million people we expect to screen for mental disorders, we anticipate that 10%–15% (approximately 470,000–720,000 people) will screen positive for at least one mental disorder. The delivery pathway showing the highest overall cost-effectiveness after this 2-year trial (1 year implementation and 1 year sustainability) in the 20 districts will be scaled up in districts from the other two pathways for 1 additional year. The districts already implementing the superior delivery pathway will enter the sustainment phase of implementation, and the rest will begin the scale-up implementation phase of the chosen (superior) delivery pathway.
Because pathway 3 (community mental health care) will introduce an increased mental health workforce that provides services at both the community and primary care levels, we anticipate that this pathway will result in better patient engagement (reach), adherence to care (retention), symptom improvement, and patient and provider satisfaction than pathways 1 (usual care) or 2 (screen, refer, and treat). We also expect that pathways 2 and 3 will have higher implementation costs and treatment fidelity than pathway 1, owing to training CHWs and PCPs on disorder detection and management. We hypothesize that gains in implementation, service, and patient outcomes will justify the increased costs associated with pathway 3 and, thus, that this pathway will be the most cost effective overall.
NEXT STEPS
After identification of the most cost-effective delivery pathway and the barriers and facilitators associated with its implementation through the process evaluation, a multistep process will engage stakeholders from multiple sectors to develop an implementation toolkit for low-cost, feasible, and sustainable systemwide implementation in LMICs.
A PRIDE scale-up toolkit working group comprising PRIDE SSA leadership, the PRIDE SSA Five Country Council, and Mozambican stakeholders will be convened to draft the toolkit on the basis of outcomes from the trial and mixed-methods process evaluation. The Five Country Council comprises senior public health officials and researchers from Botswana, Malawi, Mozambique, South Africa, and Zambia, which are U19 partners in the capacity-building component of the hub. Other Mozambican stakeholders will include CHWs, PsyTs, prescribing PCPs, and community leaders.
Study leadership will assign sections of the toolkit to subgroups for development, to be reviewed at subsequent full-group meetings. As the toolkit draft nears completion, it will be discussed by community, implementation science, and global mental health advisory groups. When the first complete draft of the toolkit is prepared, study leadership will host the PRIDE SSA Policy Workshop in collaboration with the WHO and NIMH and invite feedback from a broad array of LMIC policy makers. This information will be used by the working group to finalize the toolkit.
Identification of the most appropriate workforce for delivery of comprehensive services is crucial for effective and sustained implementation of nationwide mental health care in LMICs. Leveraging a research-policy partnership, PRIDE SSA will determine how existing human resources may best be employed to provide EBIs for management of mental disorders. The finalized toolkit developed by PRIDE SSA will be used as a guide by the Mozambican Ministry of Health in nationwide mental health policy, programming, and service scale-up. The toolkit may also serve as a template for dissemination and implementation of task-shared mental health services in other LMICs, providing a blueprint for closing the treatment gap and reducing the burden of mental disorders globally.
HIGHLIGHTS.
This study examines the delivery and scale-up of comprehensive mental health services integrated into primary care and compares usual care with two task-shifting pathways.
None of the three study arms include psychiatrists and psychologists as clinical and supervising personnel, although the latter oversee all clinical activities and train other trainers on evidence-based interventions.
The study leverages novel cost-effective technology to support capacity building, screening, and evidence-based intervention delivery with fidelity.
To maximize sustainability, research funds cover all initial training activities, including training of local trainers, but do not fund the delivery of any mental health clinical services or supervision.
Acknowledgments
Research reported in this article was supported by NIMH (U19 MH 113203) under a hub that comprises a scale-up research component in Mozambique and a capacity-building component that includes Botswana, Malawi, Mozambique, South Africa, and Zambia. This article is part of a series of protocols of NIMH-funded U19 focused on global mental health implementation science. ClinicalTrials.gov identifier: NCT03610750, registered August 1, 2018.
Dr. Weissman has received research funding from NIMH, the Brain and Behavior Foundation, the Templeton Foundation, and the Sackler Foundation. She has received book royalties from Perseus Press, Oxford University Press, and APA Publishing and receives royalties on the Social Adjustment Scale from Multi-Health Systems. Dr. Oquendo has received royalties from the Research Foundation for Mental Hygiene for the commercial use of the Columbia Suicide Severity Rating Scale and owns stock in Mantra and Bristol-Myers Squibb. She serves as an advisor to Alkermes and Fundación Jimenez Diaz. The other authors report no financial relationships with commercial interests.
REFERENCES
- 1.Chisholm D, Burman-Roy S, Fekadu A, et al. : Estimating the cost of implementing district mental healthcare plans in five low- and middle-income countries: the PRIME study. Br J Psychiatry 2016; 208(suppl 56):s71–s78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoeft TJ, Fortney JC, Patel V, et al. : Task-sharing approaches to improve mental health care in rural and other low-resource settings: a systematic review. J Rural Health 2018; 34:48–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Woltmann E, Grogan-Kaylor A, Perron B, et al. : Comparative effectiveness of collaborative chronic care models for mental health conditions across primary, specialty, and behavioral health care settings: systematic review and meta-analysis. Am J Psychiatry 2012; 169:790–804 [DOI] [PubMed] [Google Scholar]
- 4.Verdeli H, Clougherty K, Onyango G, et al. : Group interpersonal psychotherapy for depressed youth in IDP camps in Northern Uganda: adaptation and training. Child Adolesc Psychiatr Clin N Am 2008; 17:605–624 [DOI] [PubMed] [Google Scholar]
- 5.Patel V, Araya R, Chatterjee S, et al. : Treatment and prevention of mental disorders in low-income and middle-income countries. Lancet 2007; 370:991–1005 [DOI] [PubMed] [Google Scholar]
- 6.Patel V, Thornicroft G: Packages of care for mental, neurological, and substance use disorders in low- and middle-income countries: PLoS Medicine series. PLoS Med 2009; 6:e1000160–e1000160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Araya R, Rojas G, Fritsch R, et al. : Treating depression in primary care in low-income women in Santiago, Chile: a randomised controlled trial. Lancet 2003; 361:995–1000 [DOI] [PubMed] [Google Scholar]
- 8.Rojas G, Fritsch R, Solis J, et al. : Treatment of postnatal depression in low-income mothers in primary-care clinics in Santiago, Chile: a randomised controlled trial. Lancet 2007; 370:1629–1637 [DOI] [PubMed] [Google Scholar]
- 9.Bass J, Neugebauer R, Clougherty KF, et al. : Group interpersonal psychotherapy for depression in rural Uganda: 6-month outcomes: randomised controlled trial. Br J Psychiatry 2006; 188:567–573 [DOI] [PubMed] [Google Scholar]
- 10.Richards DA, Bower P, Pagel C, et al. : Delivering stepped care: an analysis of implementation in routine practice. Implement Sci 2012; 7:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bower P, Gilbody S: Stepped care in psychological therapies: access, effectiveness and efficiency. Narrative literature review. Br J Psychiatry 2005; 186:11–17 [DOI] [PubMed] [Google Scholar]
- 12.Saxena S, Thornicroft G, Knapp M, et al. : Resources for mental health: scarcity, inequity, and inefficiency. Lancet 2007; 370:878–889 [DOI] [PubMed] [Google Scholar]
- 13.Chisholm D, Flisher AJJ, Lund C, et al. : Scale up services for mental disorders: a call for action. Lancet 2007; 370:1241–1252 [DOI] [PubMed] [Google Scholar]
- 14.Kohn R, Saxena S, Levav I, et al. : The treatment gap in mental health care. Bull World Health Organ 2004; 82:858–866 [PMC free article] [PubMed] [Google Scholar]
- 15.Bolton P, Bass J, Neugebauer R, et al. : Group interpersonal psychotherapy for depression in rural Uganda: a randomized controlled trial. JAMA 2003; 289:3117–3124 [DOI] [PubMed] [Google Scholar]
- 16.Murray LK, Dorsey S, Skavenski S, et al. : Identification, modification, and implementation of an evidence-based psychotherapy for children in a low-income country: the use of TF-CBT in Zambia. Int J Ment Health Syst 2013; 7:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patel V, Weiss HA, Chowdhary N, et al. : Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANAS): a cluster randomised controlled trial. Lancet 2010; 376:2086–2095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bolton P, Bass JK, Zangana GAS, et al. : A randomized controlled trial of mental health interventions for survivors of systematic violence in Kurdistan, Northern Iraq. BMC Psychiatry 2014; 14:360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Jesus Mari J, Tófoli LF, Noto C, et al. : Pharmacological and psychosocial management of mental, neurological and substance use disorders in low- and middle-income countries: issues and current strategies. Drugs 2013; 73:1549–1568 [DOI] [PubMed] [Google Scholar]
- 20.Murray LK, Dorsey S, Haroz E, et al. : A common elements treatment approach for adult mental health problems in low- and middle-income countries. Cognit Behav Pract 2014; 21:111–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Bank Open Data. Washington, DC, World Bank, 2016. https://data.worldbank.org. Accessed Feb 22, 2019
- 22.Pasquali V: The world’s richest and poorest countries 2020. Global Finance, July 2020. https://www.gfmag.com/global-data/economic-data/worlds-richest-and-poorest-countries. Accessed Feb 7, 2020 [Google Scholar]
- 23.Schwitters A, Lederer P, Zilversmit L, et al. : Barriers to health care in rural Mozambique: a rapid ethnographic assessment of planned mobile health clinics for ART. Glob Health Sci Pract 2015; 3:109–116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vos T, Flaxman AD, Naghavi M, et al. : Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380:2163–2196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.GBD Compare Data Visualization. Seattle, Institute for Health Metrics and Evaluation, 2017. http://vizhub.healthdata.org/gbd-compare
- 26.Dua T, Barbui C, Clark N, et al. : Evidence-based guidelines for mental, neurological, and substance use disorders in low- and middle-income countries: summary of WHO recommendations. PLoS Med 2011; 8:e1001122–e1001122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.WHO Mental Health Gap Action Programme (MhGAP). Geneva, World Health Organization, 2008
- 28.Dos Santos PF, Wainberg ML, Caldas-de-Almeida JM, et al. : Overview of the mental health system in Mozambique: addressing the treatment gap with a task-shifting strategy in primary care. Int J Ment Health Syst 2016; 10:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dos Santos PF, Cumbe V, Gouveia ML, et al. : Implementation of mhGAP in Mozambique: integrating epilepsy care into the primary health care system. Int J Ment Health Syst 2019; 13:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Curran GM, Bauer M, Mittman B, et al. : Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care 2012; 50:217–226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weissman MM, Hankerson SH, Scorza P, et al. : Interpersonal counseling (IPC) for depression in primary care. Am J Psychother 2014; 68:359–383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weissman MM: Interpersonal psychotherapy: history and future. Am J Psychother 2020; 73:3–7 [DOI] [PubMed] [Google Scholar]
- 33.Hettema J, Steele J, Miller WR: Motivational interviewing. Annu Rev Clin Psychol 2005; 1:91–111 [DOI] [PubMed] [Google Scholar]
- 34.Miller WR, Rollnick S: Motivational Interviewing: Helping People Change, 3rd ed. New York, Guilford Press, 2012. [Google Scholar]
- 35.Bennett G, Miller WR, Rollnick S: Motivational Interviewing: Preparing People to Change Addictive Behavior. New York, Guilford Press, 1991 [Google Scholar]
- 36.DiClemente CC, Corno CM, Graydon MM, et al. : Motivational interviewing, enhancement, and brief interventions over the last decade: a review of reviews of efficacy and effectiveness. Psychol Addict Behav 2017; 31:862–887 [DOI] [PubMed] [Google Scholar]
- 37.Stanley B, Brown GK: Safety planning intervention: a brief intervention to mitigate suicide risk. Cognit Behav Pract 2012; 19: 256–264 [Google Scholar]
- 38.Proctor EK, Landsverk J, Aarons G, et al. : Implementation research in mental health services: an emerging science with conceptual, methodological, and training challenges. Adm Policy Ment Health 2009; 36:24–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Proctor E, Silmere H, Raghavan R, et al. : Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health Ment Health Serv Res 2011; 38:65–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Curran GM, Bauer M, Mittman B, et al. : Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care 2012; 50:217–226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sweetland AC, Oquendo MA, Sidat M, et al. : Closing the mental health gap in low-income settings by building research capacity: perspectives from Mozambique. Ann Glob Health 2014; 80:126–133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moçambique Censo. Maputo, Mozambique, Instituto Nacional de Estatistica. www.ine.gov.mz. Accessed Feb 7, 2020 [Google Scholar]
- 43.Scully RP: Idai’s trail of destruction. New Sci 2019; 3223:24–25 [Google Scholar]
- 44.Kojima N: HIV care following two devastating cyclones in Mozambique. AIDS Res Hum Retroviruses 2019; 35:689–690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wainber ML, Oquendo M, Weissman MM: Electronic Mental Wellness Tool (e-mwTool) for Diagnosis and Treatment Planning. New York, Columbia University, 2020. https://columbia.resoluteinnovation.com/technologies/CU20214_electronic-mental-wellness-tool-e. Accessed Feb 7, 2020 [Google Scholar]
- 46.Lovero KL, Basaraba C, Khan S, et al. : Brief screening tool for stepped-care management of mental and substance use disorders. Psychiatr Serv (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thomas CC, Rathod SD, De Silva MJ, et al. : The 12-item WHO Disability Assessment Schedule II as an outcome measure for treatment of common mental disorders. Glob Ment Health 2016; 3:e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brazier J, Roberts J, Deverill M: The estimation of a preference-based measure of health from the SF-36. J Health Econ 2002; 21:271–292 [DOI] [PubMed] [Google Scholar]
- 49.Chamberlain P, Brown CH, Saldana L: Observational measure of implementation progress in community based settings: the stages of implementation completion (SIC). Implement Sci 2011; 6:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Saldana L, Chamberlain P, Bradford WD, et al. : The cost of implementing new strategies (COINS): a method for mapping implementation resources using the stages of implementation completion. Child Youth Serv Rev 2014; 39:177–182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Luke DA, Calhoun A, Robichaux CB, et al. : The Program Sustainability Assessment Tool: a new instrument for public health programs. Prev Chronic Dis 2014; 11:130184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Calhoun A, Mainor A, Moreland-Russell S, et al. : Using the Program Sustainability Assessment Tool to assess and plan for sustainability. Prev Chronic Dis 2014; 11:130185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jorm AF: Mental health literacy. Public knowledge and beliefs about mental disorders. Br J Psychiatry 2000; 177:396–401 [DOI] [PubMed] [Google Scholar]
- 54.Avallone F, Pepe S, Porcelli R, et al. : Perceived self-efficacy in job search: measurement scales; in Needs, Values, and Self-Efficacy in Choosing a Job [in Italian]. Rome, Institute for the Development of Vocational Training of Workers, 2007 [Google Scholar]
- 55.Pepe SJ, Maria MLF, Francesco A, et al. : Work Self-Efficacy Scale and Search for Work Self-Efficacy Scale: a validation study in Spanish and Italian cultural contexts. Rev Psicol Trab Organ 2010; 26:201 [Google Scholar]
- 56.Aarons GA: Mental health provider attitudes toward adoption of evidence-based practice: the Evidence-Based Practice Attitude Scale (EBPAS). Ment Health Serv Res 2004; 6:61–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Timmings C, Khan S, Moore JE, et al. : Ready, set, change! Development and usability testing of an online readiness for change decision support tool for healthcare organizations. BMC Med Inform Decis Mak 2016; 16:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Damschroder LJ, Aron DC, Keith RE, et al. : Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009; 4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tabak RG, Khoong EC, Chambers DA, et al. : Bridging research and practice: models for dissemination and implementation research. Am J Prev Med 2012; 43:337–350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Harris PA, Taylor R, Thielke R, et al. : Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42:377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Harris PA, Taylor R, Minor BL, et al. : The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019; 95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.MhGAP Intervention Guide For Mental, Neurological and Substance Abuse Disorders in Non-Specialized Health Settings: Mental Health Gap Action Programme (mhGAP). Geneva, World Health Organization, 2016 [PubMed] [Google Scholar]
- 63.Weissman MM, Markowitz JC, Klerman GL: The Guide to Interpersonal Psychotherapy. Oxford, UK, Oxford University Press, 2018 [Google Scholar]
- 64.Group Interpersonal Therapy (IPT) for Depression. Geneva, World Health Organization, 2016 [Google Scholar]
- 65.Velasquez MM, Stephens NS, Ingersoll K: Motivational interviewing in groups. J Groups Addict Recovery 2006; 1:27–50 [Google Scholar]
- 66.Lincoln YS, Guba EG: Naturalistic Inquiry. Washington, DC, Sage Publications, 1985 [Google Scholar]
- 67.Craig P, Dieppe P, Macintyre S, et al. : Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008; 337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.May CR, Mair FS, Dowrick CF, et al. : Process evaluation for complex interventions in primary care: understanding trials using the normalization process model. BMC Fam Pract 2007; 8:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Moore GF, Audrey S, Barker M, et al. : Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015; 350:h1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Palinkas LA, Aarons GA, Horwitz S, et al. : Mixed-method designs in implementation research. Adm Policy Ment Health 2011; 38:44–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Aarons GA, Palinkas LA: Implementation of evidence-based practice in child welfare: service provider perspectives. Adm Policy Ment Health 2007; 34:411–419 [DOI] [PubMed] [Google Scholar]


