Abstract
Background
Q-methodology is an approach to studying complex issues of human ‘subjectivity’. Although this approach was developed in the early twentieth century, the value of Q-methodology in healthcare was not recognised until relatively recently. The aim of this review was to scope the empirical healthcare literature to examine the extent to which Q-methodology has been utilised in healthcare over time, including how it has been used and for what purposes.
Methods
A search of three electronic databases (Scopus, EBSCO-CINAHL Complete, Medline) was conducted. No date restriction was applied. A title and abstract review, followed by a full-text review, was conducted by a team of five reviewers. Included articles were English-language, peer-reviewed journal articles that used Q-methodology (both Q-sorting and inverted factor analysis) in healthcare settings. The following data items were extracted into a purpose-designed Excel spreadsheet: study details (e.g., setting, country, year), reasons for using Q-methodology, healthcare topic area, participants (type and number), materials (e.g., ranking anchors and Q-set), methods (e.g., development of the Q-set, analysis), study results, and study implications. Data synthesis was descriptive in nature and involved frequency counting, open coding and the organisation by data items.
Results
Of the 2,302 articles identified by the search, 289 studies were included in this review. We found evidence of increased use of Q-methodology in healthcare, particularly over the last 5 years. However, this research remains diffuse, spread across a large number of journals and topic areas. In a number of studies, we identified limitations in the reporting of methods, such as insufficient information on how authors derived their Q-set, what types of analyses they performed, and the amount of variance explained.
Conclusions
Although Q-methodology is increasingly being adopted in healthcare research, it still appears to be relatively novel. This review highlight commonalities in how the method has been used, areas of application, and the potential value of the approach. To facilitate reporting of Q-methodological studies, we present a checklist of details that should be included for publication.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12874-021-01309-7.
Keywords: Q-methodology, Mixed methods, Healthcare, Qualitative methods, Factor analysis, Subjectivity, Patient perspectives
Background
Healthcare systems and organisations are recognised for their complexity. They involve a diverse number of stakeholders, such as healthcare professionals, patients, family members/informal caregivers, policymakers, insurance agencies, governments, professional bodies, community and charitable organisations, and the general public [1]. These individuals and groups interact and influence one another in the planning, delivery and receipt of care. Formalised examples of such interactions include multidisciplinary meetings [2], care coordination [3], and consumer involvement in service organisations [4]. However, stakeholder groups often have distinct perspectives and priorities on issues related to care delivery, even those that seem well-defined, such as the nature of illness, what constitutes appropriate treatment, or quality of care [5–8].
Understanding differing perspectives within healthcare is important because the ways in which individuals and groups makes sense of these issues affects their behaviours [9]. Research methods to apprehend perspectives have traditionally been qualitative (e.g., interviews and focus groups), though quantitative surveys have also been utilized to assess stakeholders’ attitudes. These approaches have their own well-described strengths and limitations [10–12]. Another approach that has gained recognition in healthcare research for identifying and comparing individuals’ and groups’ contrasting viewpoints is Q-methodology.
Q-methodology: A mixed-method for studying perspectives
Q-methodology combines qualitative and quantitative techniques to empirically study subjectivity [13]. It involves Q-sorting, where individuals articulate their own viewpoint by ranking a set of statements (the Q-set) about a particular issue based on some defined dimension, for example, level of agreement or perceived importance [14]. Each participant’s final ranking of statements is called their ‘Q-sort’ and these are analysed using inverted factor analysis techniques; ‘inverted’ because each participant (or their whole Q-sort) is treated as a variable, unlike factor analysis of surveys, where the items are variables. The analysis aims to identify patterns of similarity as well as differences in how participants have ranked, and therefore understood, the Q-set. Factors emerge as the commonalities across participants’ viewpoints and are qualitatively interpreted. The whole process of a Q-methodological study can be summarised in seven stages (see Fig. 1).
Fig. 1.
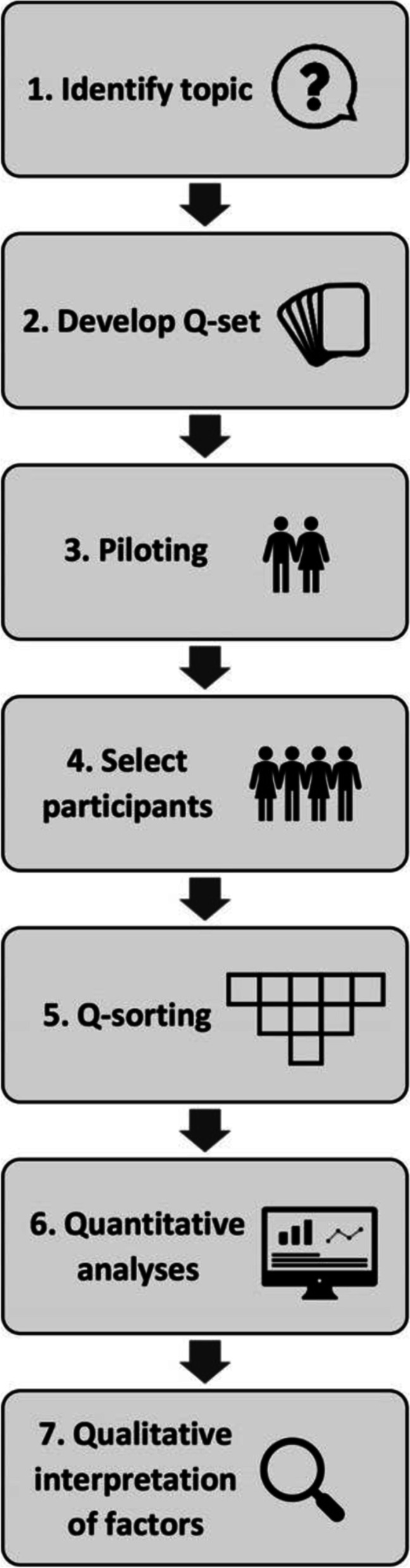
The stages of Q-methodology
Stage 1: Identify the topic
Q-methodology identifies differences in what people think, as well as common viewpoints (shared meaning). Accordingly, suitable topics are those complex and socially contested subject matter where we expect to find both variation and commonality, for which we want to “hear ‘many voices’” [15].
Stage 2: Develop the Q-set
Developing the Q-set involves collection of discrete ideas, concepts, or usually statements about the topic, ideally until saturation is reached. In Q-studies, this is called sampling the concourse which refers to all the ideas and statements that can be sensibly expressed about that topic. Sampling might involve a literature review, preliminary data collection (e.g., interviews) or searching other publicly available resources [16]. Collected statements are then reduced and refined (e.g., grouping similar ideas together) to produce a manageable Q-set [17].
Stage 3: Piloting
Piloting provides researchers with insights into the ease with which instructions and statements are understood, the time taken to complete the Q-sort, and participants’ overall impression of Q-sorting. These may lead to modifications to the study materials or procedure [17].
Stage 4: Participant selection
Q-methodology uses purposive sampling; participants are selected because they are able to articulate a viewpoint on the topic of interest and because their perspective matters [14, 15]. In quantitative surveys, larger samples are required to ensure representativeness and generalisability [18, 19]. On the other hand, because Q-methodology uses an inverted factor analysis and does not aim to generalise to a population, studies typically have samples of around 40–60 participants [14, 15].
Stage 5: Data collection—Q-sorting
Data collection involves a card-sorting task called ‘Q-sorting’, where participants rank the statements in the Q-set. To begin, participants are provided with a clear question or prompt about the topic and then asked to respond by ordering the statements according to some level of judgement (e.g., “most strongly disagree” to “most strongly agree”). Q-sorting is typically conducted on a fixed quasi-normal distribution grid, which facilitates ranking and formalises the tendency for individuals to feel relatively strongly about fewer issues [14]. Some studies have incorporated think-aloud tasks [20] during Q-sorting [21–23], in order to capture participants’ thoughts about different statements and their decision-making processes in real-time. Following completion of their Q-sort, participants are usually asked post-sorting questions about the process, as well as about their background and experience of the topic in general; this may lead into the use of other empirical methods (e.g., interviews).
Stage 6: Analysis—Quantitative analyses to obtain factors
Factor analysis is a statistical method for classifying variables (here Q-sorts) into factors through the identification of sizable portions of shared meaning [14]. Factors are found by correlating each Q-sort with every other one to determine the extent to which they have a similar configuration of the Q-set. Q-sorts with a lot in common are typically subsumed under the same factor. Technical aspects of analysis in Q-methodology are similar to traditional factor analysis, with a number of different options for factor extraction (centroid, principal component) and rotation (varimax, by-hand) available depending on the research question and nature of the study.
Stage 7: Interpretation—Qualitative interpretation of factors
Qualitative factor interpretation is assisted by the construction of factor arrays—ideal Q-sorts computed for each factor based on a weighted averaging of the participants’ Q-sorts that loaded on the factor. The overall configuration of statements in a factor array is more important than the placement of a few particular items (e.g., most negative/positive). Interpretation involves developing narratives for each factor that incorporate as many statements from the factor array as possible and may draw on other data of participants who loaded on that factor.
Q-methodology in healthcare research
Q-methodology was developed by psychologist William Stephenson in the early part of the twentieth century in the United Kingdom (UK) [24, 25]. Unlike surveys and conventional factor analysis, it had little take-up until much later, with the publication of a seminal text discussing its value to political science [26]. More recently, a number of authors have highlighted the value of Q-methodology for healthcare research. In 1997, Valenta and Wigge [27] introduced Q into health informatics, where it was used to measure physicians’ and medical students’ propensity to adapt to information technology in their workplace. Almost a decade later, Cross [28] argued for the value of studying attitudes in health-related fields using Q-methodology, noting how one’s subjectivity fundamentally impacts on one’s own behaviour. In 2008, Akhtar-Danesh, Baumann et al.[29] put forward a case for using Q in nursing research to study attitudes, feelings, values and life experiences, a theme then picked up by Simons [30] in 2013. More recently, Q-methodology has been advanced as an approach for studying priorities and priority-setting in healthcare [21, 22, 31–33]. Despite this, the extent to which Q-methodology has been utilised in healthcare, how, and for what purposes, remains unclear. Such information on current applications would not only provide insights into emerging conventions for its use in healthcare, but also demonstrate to what extent Q-methodology has value in this field.
A scoping review was selected as the most appropriate review approach because the focus was to examine how research is conducted within a defined field (Q-methodology in healthcare) and identify key characteristics of this body of research [34]. The aim of this scoping review was to explore how Q-methodology has been used in healthcare research. Specifically, this study answered the following research questions:
For what reasons is Q-methodology used in healthcare?
What healthcare topic areas are explored or studied using Q-methodology?
What types of participants are involved in these studies?
What materials are used in these studies?
How has Q-methodology been applied in healthcare studies? (i.e., details of the methods).
What are the results and potential implications of these Q-methodological studies?
Methods
A protocol was developed to cover all stages of this scoping review and was agreed upon by KC and KL prior to conducting the search, but not published. The reporting of this review was guided by the Preferred Reporting Items for Systematic Review and Meta-analyses extension for Scoping Reviews (PRISMA-ScR) checklist [35]. The checklist for the PRISMA-ScR is provided in Additional file 1.
Search and information sources
In January 2020, Scopus (Title-abstract-keywords), EBSCO-CINAHL Complete (title, abstract, subject headings) and Medline (Web of Science topic search) were searched using the terms outlined in Table 1. The full search for Medline is provided in Additional file 2. No date restrictions were applied to the search. Data records were downloaded into EndNote X8 and duplicates were removed.
Table 1.
Search strategy
| Keywords |
|---|
| 1. q methodology OR q-methodology OR q method OR q-method OR q sort OR q-sort |
| AND |
| 2. health care OR healthcare OR health-care OR medica OR nursa OR health services OR patient OR hospitala OR clinica OR acute care OR primary health OR primary care OR general practice |
a indicates truncation
Eligibility criteria and study selection
The inclusion criteria were: a) English-language, b) a peer-reviewed journal article; c) focuses on healthcare; d) constitutes a full Q-methodological study of (i) Q-sorting (e.g., card-sorting techniques) AND (ii) inverted factor analysis; f) full-text is available. ‘Healthcare’ included perspectives on health issues that impact care provision, recognised sites of healthcare delivery, or involvement of patients and healthcare professionals, including the education of healthcare professionals. Studies of health, i.e., individuals’ personal perspectives on wellbeing or their health conditions were excluded if not also related to healthcare delivery.
To establish inter-rater reliability, KC and KL completed a blinded title and abstract review of a random 5% sample of publications. A title and abstract review of remaining publications was conducted by KC. Included articles then underwent a full-text review by KC, KL, WW, KG and HMN. Regular discussions were had between team members to ensure consistency of article inclusion.
Data collection processes and data items
Data items were extracted from included articles into a purpose-designed Microsoft Excel spreadsheet and included: publication details; country(ies) where data was collected; study aim; healthcare topic; reasons for using Q-methodology; methods for devising the Q-set; number of statements; ranking anchors; delivery method; analysis method, rotation and program used; other methods used; number of participants and participant group description; number and names of factors; variance explained; and study implications.
Synthesis of results
The synthesis of results was descriptive in nature. Frequency counts were used to summarise the findings, which were then organised by data items. An iterative process of coding was used to develop a classification system for the broad healthcare topic areas and for study authors’ reasons for using Q. Throughout the results section of this review, examples are used from included studies to illustrate how Q-methodology has been used in healthcare research.
Results
Search
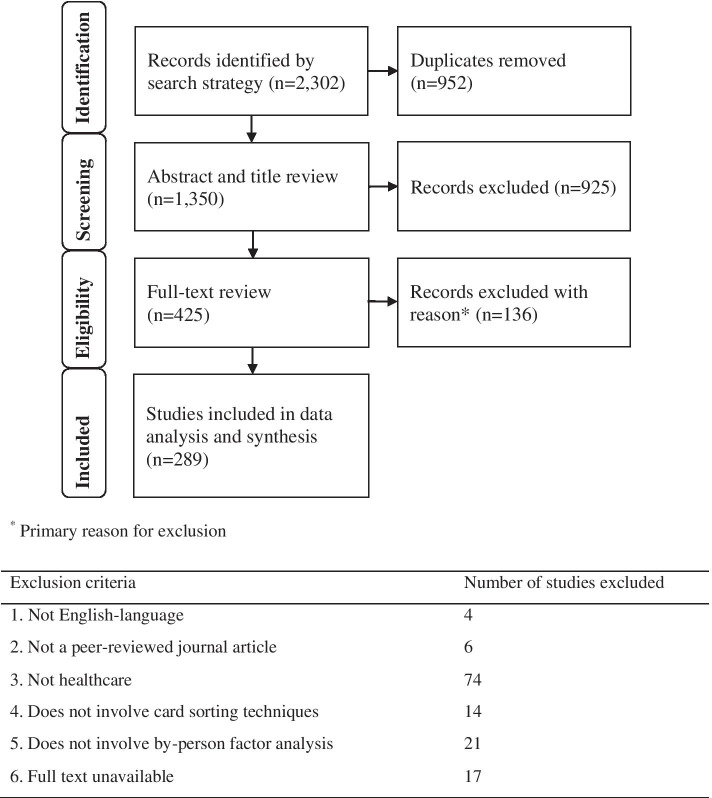
A total of 2,302 publications were identified by the search strategy, with 1,350 publications included for screening and review after removal of duplicates. Cohen’s kappa for the 5% blinded double screening of abstracts was calculated as 0.82, which is considered a ‘strong’ level of agreement [36]. Figure 2 details the retention of studies after the abstract and title review and the full-text review. A total of 289 studies were included for data analysis and synthesis. Full details of all included studies are provided in Additional file 3.
Fig. 2.
PRISMA diagram of search and review process [37]
Characteristics of included articles
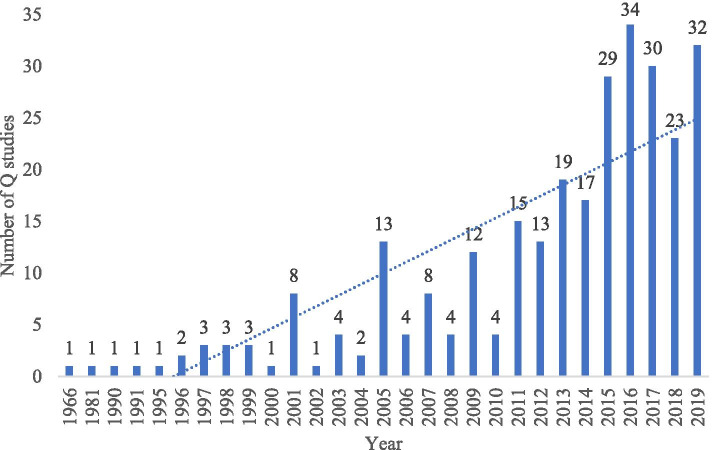
Studies were published between 1966 and 2019 (Fig. 3), across 188 different journals. The journals publishing the most healthcare-related Q-methodology studies were: the Journal of Advanced Nursing (n = 13), Nurse Education Today (n = 9), Patient Preference and Adherence (n = 6), Psychology and Psychotherapy: Theory, Research and Practice (n = 6), the Indian Journal of Science and Technology (n = 5), Patient Education and Counseling (n = 5) and Nursing & Health Sciences (n = 5).
Fig. 3.
Included studies year of publication
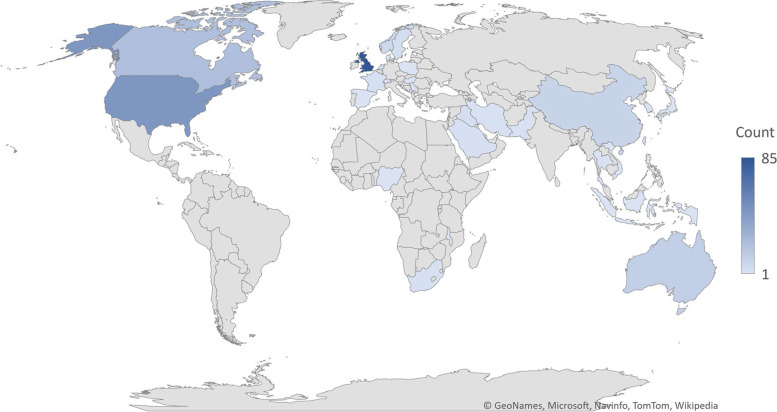
The included studies had been conducted in 34 countries (Fig. 4), with four studies [32, 38–40] reporting on multiple countries. Nine studies did not state which country the research had been conducted in [41–49]. The majority of studies were conducted in the UK (n = 85), followed by The United States (US) (n = 46), South Korea (n = 40), Canada (n = 22), the Netherlands (n = 22) and Australia (n = 12).
Fig. 4.
Geographic distribution of countries publishing Q-methodology studies. Microsoft product screen shot(s) reprinted with permission from Microsoft Corporation
Reasons for using Q-methodology
A diverse range of reasons were provided for using Q-methodology. These justifications were grouped into five categories: exploring complex issues, taking a holistic approach, useability of results, rigour, and practicalities.
Exploring complex issues
Q-methodology was described as an ideal method for exploring complex or controversial topics [50] and topics that were likely to elicit strong opinions, differing perspectives, or underacknowledged views, something which is particularly pertinent to healthcare [51–54]. For example, Askay et al. [42] reasoned that standardised and relatively objective assessments, such as questionnaires, may not be appropriate to assess the physical, emotional and social reasons for distress in burn survivors because they are unlikely to be able to quantify the complex interactions among the reasons. Q-methodology was also used due to its less-confronting nature (i.e., participants are not asked direct questions but rather they respond to pre-established statements) [55]. Some studies justified that Q-methodology had been successfully used in previous studies of similar participant groups or topics; for example, Clarke and Holt’s disability-related research [56] and Grijpma et al.’s research with kidney transplant patients [57].
Taking a holistic approach
Regarding the study approach, Q-methodology was said to be a person-centred, holistic approach that provided a ‘wholeness’ of view [50, 58, 59]. This was in part due to the forced-choice nature of the method. Some studies reported using Q-methodology as it requires participants to sort cards in relation to each other [60]. This meant that participants were not able to select the same response for each item, which was reasoned to more accurately portray real-life situations in which decision-making is constrained and must consider multiple factors [61]. The forced-choice answering style used by Q-methodology makes it likely to identify opposing opinions [62]. White et al. pointed out that other methods, such as surveys, often average opposing opinions, which can then be incorrectly interpreted as neutrality [63, 64]. Flurey and Morris [65] noted that patients with rheumatoid arthritis likely had variable daily life experiences; more traditional methods for collecting experience, however, tended to produce “overall consensus on these experiences (creating) the potential problem of providing a ‘bland generalisation’”. (page 365).
Useability of results
In terms of study outcomes, one of the most common reasons for using Q-methodology was that it enables subjectivity to be empirically studied by identifying distinct attitudes, motives, perspectives, beliefs, feelings, priorities, perceptions, views or typologies [57, 66–68]. For example, Jedeloo et al. [66] used Q-methodology to explore the preferences of adolescents with chronic conditions regarding self-management of care and hospital care. The study findings could be used to guide nurses’ interactions with adolescents with chronic condition and tailor care to their preferences.
Rigour
Another common reason given by study authors for using Q-methodology was its rigour. Q-methodology was said to allow participants to create their own meaning while reducing the impact of prior assumptions and the potential biases of the researcher [69, 70]. Many studies referred to the integration of qualitative and quantitative techniques as one of Q-methodology’s key strengths, [42, 71–73] combining the richness of qualitative data with the rigour of statistical analysis [74]. Q-methodology was also described as avoiding problems associated with missing data because Q-sorts are only analysed as completed wholes [75].
Practicalities
The practicalities of Q-methodology were a further justification for its use. For some studies this was because it only requires a small number of participants, which is useful when studying a minority participant group, such as operating room personnel [76] or mothers on a psychiatric Mother and Baby Unit [55]. Whyte and Smith reasoned that the boardgame-like nature of the method was familiar to adolescents and therefore would be fun for participants [77]. Q-methodology was said to allow participants to express their views non-verbally, [78, 79] which enabled patients with communication difficulties, for example, head and neck cancer patients, to participate [80].
Topics of Q-studies in healthcare
Topic areas covered a broad range of settings and healthcare conditions (Table 2). The most common topic areas were health professional education (n = 50, 17.3%), nursing practice (n = 39, 13.5%) and mental healthcare (n = 37, 12.8%).
Table 2.
Topic areas for studies using Q-methodology in healthcare
| Topic Area | Count | % |
|---|---|---|
| Health professional education | 50 | 17.3 |
| Nursing practice | 39 | 13.5 |
| Mental healthcare | 37 | 12.8 |
| Chronic disease | 18 | 6.2 |
| Gender, sexual and reproductive health | 16 | 5.5 |
| End of life care | 15 | 5.2 |
| Health and healthcare attitudes | 11 | 3.8 |
| Cancer | 10 | 3.5 |
| Healthcare technology | 9 | 3.1 |
| Health system planning, resource allocation and access | 8 | 2.8 |
| Organisational values, behaviours and roles | 8 | 2.8 |
| Allied health | 8 | 2.8 |
| Dentistry and orthodontics | 8 | 2.8 |
| Primary care | 7 | 2.4 |
| Dementia and aged care | 7 | 2.4 |
| Pharmacy | 7 | 2.4 |
| Caregiving | 6 | 2.1 |
| Othera | 25 | 8.7 |
| Total | 289 | 100 |
a ‘Other’ covers categories with ≤ 5 studies and includes acute and infectious conditions, disability, medicine, organ transplant, paediatric care, population health, rehabilitation, and research practice
Participants
Q-methodological studies in healthcare included a diverse range of stakeholders (e.g., patients, doctors, nurses, informal caregivers, medical students), which could be broadly classified as those receiving or consuming care (consumers) or those delivering or organising formal care (providers). Thirty studies (10.4%) [27, 53, 59, 64, 81–106] involved both consumer and provider participants. Four of these studies [87, 92, 105, 107] did not clearly report the breakdown between the types of participants. One other study involved a mix of consumers and providers, with some participants belonging to both categories [94].
Consumers
Consumers were participants in 123 studies (65.1%) and included previous and current patients from a variety of settings (e.g., hospitals, out-patient clinics, orthodontics, antenatal clinics, psychiatric settings, primary care), informal caregivers/family, people with various medical conditions, and members of the general public. Of those studies clearly specifying the number of consumers, the number of participants (P-set) ranged from 5–299 (Mdn = 33).
Providers
Care providers were participants in 196 studies (67.8%). The term ‘provider’ refers to health professionals (e.g., psychologists, nurses, GPs, allied health professionals, specialists, community health workers, medical residents), hospital volunteers, people working in a healthcare-related field (e.g., IT specialists or university faculty members), and students studying healthcare-related fields (e.g., nursing, medicine, physiotherapy). The most common occupations of participants were nurses (n = 76, 38.6%), GPs/Physicians (n = 48, 24.4%), and students (n = 42, 21.3%). Nursing was the most common study area for studies involving students (30 of 42 studies, 71.4%). Over a third of studies involving providers (n = 70, 35.7%) had participant samples comprising a mix of professions. Of the studies clearly specifying the number of care provider participants, P-sets ranged from 4–710 (Mdn = 39).
Materials
Sampling the concourse and developing the Q-set
The methods used to sample the concourse were varied, with most studies utilising multiple sources of information. These included reviewing academic literature (n = 186, 64.4%), conducting interviews (n = 138, 47.8%), seeking input from ‘experts’ in the field (n = 59, 20.4%), running focus groups or group discussions (n = 45, 15.6%), reviewing grey literature such as media sources and websites (n = 44, 15.2%), using a Q-set derived from a previous study (n = 33, 11.4%), and repurposing items from surveys or questionnaires (n = 19, 6.6.%). Other less common methods included video-taped counselling sessions, observations, and conducting document/audit reviews. Twelve studies (4.2%) did not report on how inputs for the Q-set were identified, or the reporting was unclear.
Methods to then reduce collected statements to a usable Q-set included piloting, expert review, thematic analysis and use of theoretical frameworks. The numbers of statements in a final Q-set ranged from 16–275 (Mdn = 42). Nine studies [65, 95, 103, 108–113] (3.1%) used multiple Q-sets for different participant groups. Two studies (0.7%) did not report the number of statements used.
Ranking scales and anchors
Numerical rankings used to sort the Q-set ranged from -2 to + 2 (or + 1 to + 5) to -7 to + 7. The most common numerical ranking was -4 to + 4 (n = 109, 37.7%), followed by -5 to + 5 (n = 90, 21.1%). Twelve studies (4.2%) did not include a negative value, for example, + 1 to + 9. Two studies [65, 113] (0.7%) involved the administration of two Q-sets with different ranking scales. In Flurey et al.’s study of rheumatoid arthritis, [65] participants were first asked to sort 39 statements regarding their daily experiences of living with rheumatoid arthritis from least agree (-5) to most agree (+ 5). They were then asked to sort a different Q-set comprising 23 statements regarding their help-seeking behaviours, from least agree (-4) to most agree (+ 4). Tang and colleagues [113] asked orthodontic patients to sort 30 statements about the reasons for wearing braces, ranked from -4 to + 4. They also asked patients’ parents to sort 35 cards about the reasons for their children’s orthodontic treatment, ranked from -5 to + 5. Twenty studies (6.9%) did not report the numerical ranking used.
Agreement was the most common anchoring term (n = 189, 65.4%), followed by importance (n = 26, 9.0%), priority (n = 4, 1.4%), characteristic (n = 3, 1.4%), significance (n = 3, 1.4%) and negative/positive (3%, 1.4%). Thirty-one additional anchors were used by either one or two studies. Twenty studies (6.9%) did not report on the anchor terminology used.
Administration of the Q-sorting task
The majority of studies (n = 184, 63.7%) delivered the Q-sorting task face-to-face, with one study [114] allowing participants to take the Q-sorting task away and return their Q-sorts within 3 weeks. Eighteen studies (6.2%) administered the Q-sorting task via mail. Twenty-eight studies (9.7%) administered the Q-sorting task online. An additional ten studies (3.5%) used multiple delivery methods; five studies [81, 89, 102, 115, 116] (1.7%) administered hard copies of the Q-sorting task both face-to-face and via mail, and five other studies [32, 59, 84, 106, 117] (1.7%) used both online and face-to-face administration. Forty-five studies (15.6%) did not explicitly state how Q-sorting was administered and four (1.4%) were unclear.
Of the 33 studies offering online administration, FlashQ (n = 12, 36.7%) was the most commonly used analysis program. Other programs included Q Assessor (n = 5, 15.2%), author-developed platforms (n = 4, 12.1%), Q-SortWare (n = 2, 6.1%), POETQ (n = 2, 6.1%), emailed PQS files (n = 1, 3.0%), Q-SORTOUCH (n = 1, 3.0%), QSort (n = 1, 3.0%), QSortOnline (n = 1, 3.0%), HTMLQ (n = 1, 3.0%) and WebQ (n = 1, 3.0%). Two studies did not specify which online program was used.
Additional methods of data collection
Studies commonly used methods in addition to Q-sorting; more than half (n = 165, 57.1%) used a post-sorting interview, asked additional questions, or allowed for comments to be made on how participants sorted the statements. These post-sorting methods involved enquiring about participants’ placements of cards, particularly at the extreme rankings. Twenty-three studies (8.0%) involved surveys and questionnaires, 14 studies conducted interviews on topics related to the focus of the Q-study but not explicitly about the card placement (4.8%), and 13 studies involved focus groups or group discussions (4.5%). Other methods or analyses included observations, additional statistical analysis, think-aloud tasks, and validity testing.
Two studies [31, 118] (0.7%) translated their Q-methodology findings into a survey, referring to the process as ‘Q2S’. Through a Q-methodological study, Baker et al. [31] identified three viewpoints (factors) on healthcare priorities and resource allocation. In the same article, they then adapted the Q-sorting task into a survey to identify the distribution of each of the three viewpoints in a larger population. Leggat et al. [118] identified two factors regarding the content of clinical supervision for allied health staff. The results were used to develop a survey on the content, outcomes and understanding of clinical supervision.
Analysis
Over half of the studies (n = 164, 56.7%) provided complete details of the analysis, reporting on the type of factor extraction, rotation and analysis program used. Of the included studies, 116 (40.1%) partially reported the details of their analysis and nine studies (3.1%) did not specify details about the analysis. Two of the included studies [44, 119] (0.7%) carried out second order factor analysis to identify ‘super factors’1 or higher-order factors. Wong, Eiser [119] identified three moderately correlated super factors that influenced physician end-of-life care decisions— “patient-focused beneficence”, “patient- and surrogate-focused”, and “best interest guided by ethical principles”—from 17 first order factors. Dennis et al. [44] compared real and ideal hospital environments, identifying three super factors—“Professional”, “Personal” and “Constrained”—from three real and three ideal first order factors.
Type of factor extraction
Principal Component Analysis (PCA) was used in 110 studies (38.1%) and centroid analysis was used in 91 studies (31.5%). An additional study [120] (0.3%) first used centroid factor analysis in the assessment of General Practitioners’ perceptions of irritable bowel syndrome. As this indicated the presence of one dominant factor, the authors re-analysed the data using PCA. In 87 of the studies (30.1%), the type of factor extraction used was not reported or was unclear.
Rotation
Varimax rotation was used in 206 studies (71.3%) and by hand/manual rotation was used in four (1.4%). Two additional studies [121, 122] (0.7%) used both varimax and manual rotation and two others [123, 124] (0.7%) used oblimin rotation. In their study of medical students’ attitudes toward kidney physiology and nephrology, Roberts et al. [122] explained that they initially used varimax rotation to simplify the factor solution and then manually rotated it in order to better separate students with different attitudes. Skorepen et al. [121] did not provide justification for undertaking both manual and varimax rotation in their study of suffering and dignity in psychiatric hospitals. In two studies [39, 86] (1.0%), the unrotated solution was accepted. Eaton [86] explained that in their study of good birthing experiences an unrotated factor solution was accepted as a dominant factor was revealed by the factor analysis, accounting for a high amount of the study variance. In Paige and Morin’s study [39] on nurse educators’ perspectives of simulation design, the factor solution was initially rotated, however, as this resulted in highly correlated factors, the unrotated factor solution was accepted. Seventy-three studies (25.3%) did not clearly report the type of rotation used, if any.
Analysis program
The most commonly used analysis program was PQMethod (n = 186, 64.4%), followed by PCQUANL/QUANL (n = 36, 12.5%) and PCQ (n = 21, 7.3%). Other programs included SPSS (n = 9, 3.1%), Q-Assessor (n = 5, 1.7%), QMethod (n = 4, 1.4%), Qanalyze (n = 1, 0.3%), SAS (n = 1, 0.3%) and STATA software (n = 1, 0.3%). One study [125] (0.3%) used both SPSS and Q-com to analyse data. In 24 of the studies (8.3%), the program used to analyse data was not reported.
Q-study implications
Authors’ spoke about the implications of their Q-study findings in terms of informing and influencing working and teaching practices, education curricula, clinical treatments, care delivery, policy and protocols, and staff members’ and patients’ wellbeing, while taking into consideration underlying cultural, social, religious, contextual and ethical factors. To more specifically demonstrate how Q-methodology has been used in studies of healthcare and what implications these studies have for clinical practice and/or policy, we present three examples of included studies (Table 3).
Table 3.
Examples of included studies
| Publication | Clarke & Holt46 | Killam, Mossey, Montgomery & Timmermans109 | Protiére, Baker, Genre, Goncalves & Viens110 |
|---|---|---|---|
| Study aim | To identify and explore the perspectives of nurses and other multidisciplinary stroke team members on nurses’ practice in stroke rehabilitation | To explore undergraduate baccalaureate nursing students’ understanding of clinical safety | To elicit stakeholders’ viewpoints about the dimensions at stake in determining marketing authorisation (MA) and about the processes used to grant MA (including whether the cost of the treatment should be considered in the MA procedure) |
| Topic | Perceptions of treatment/change/intervention | Education | Cancer |
| Development of the Q-set | Data from previous study | Refined from a concourse used in a previous Q study | Review of the literature; semi-structured interviews |
| Number of statements in Q-set | 32 | 43 | 34 |
| Ranking scale and anchors | Most disagree (-4) to Most agree (+ 4) | Most disagree (-5) to Most agree (+ 5) | Most disagree (-4) to Most agree (+ 4) |
| Example statement | Nurses are the most appropriate professional to liaise between stroke survivors, families and the stroke unit team | The student makes independent clinical decisions beyond his/her competency | If a treatment can prolong lifespan, even by one month, it should be given MA whatever its cost to society |
| Delivery method | Face-to-face | Face-to-face | Online (Flash Q) |
| Participants | 63 healthcare employees regularly working with/visiting patients on a stroke unit (registered nurse, healthcare assistant, therapist, physician, dietician, social worker, clinical psychologist, orthoptist) | 68 first year nursing students | 48 healthcare employees (oncologists, healthcare decision makers, individuals from the pharmaceutical industry) and 104 consumers (patients; members of the general population) |
| Analysis | PCA; Varimax; PQMethod | Centroid; Varimax; PQMethod | PCA; Manual rotation; PQMethod |
| Other methods | Post-sorting questions/additional comments; semi-structured interviews | Post-sorting group discussion | Post-sorting questions/additional comments |
| Factors/viewpoints | n = 4 | n = 4 | n = 3 |
| 1. Integrate rehabilitation principles in routine nursing practice; 2. Physical care activity takes priority over rehabilitation principles; 3. Support the wider stroke team to provide stroke rehabilitation; 4. Be cautious about nurse’ engagement in stroke rehabilitation practice | 1. Overwhelming sense of inner discomfort; 2. Practicing contrary to conventions; 3. Lacking in professional integrity; 4. Disharmonising relations | 1. Quality of life, opportunity cost and participative democracy; 2. Quality of life and patient centeredness; 3. Length of life | |
| Variance explained | 66% | Not reported | 44% |
| Study implications | Results gave insight into similarities and differences in viewpoints amongst clinical staff on nursing practices in stroke units. Study findings demonstrated the need for structured competency-based multidisciplinary training in rehabilitation skills to facilitate partnerships between registered nurses and healthcare assistants in stroke rehabilitation | The study found that compromised clinical safety is a complex concept involving personal, professional and programic variables. The authors suggested that study findings could be used to develop learning environments that are safety-oriented and student-centred | Based on the study findings, the authors indicated that there is a need for transparency and re-evaluation of treatments after they have received marketing authorisation. They also suggest that authorisation criteria should include a greater focus on quality of life in the context of advances cancer care |
Factor solutions
The numbers of factors identified by studies ranged from 0 (i.e., no identifiable factors) to 21 factors, which takes into account the total number of factors across participant groups. For example, Protière et al. [101] identified four factors for patients and four factors for healthcare professionals in their study of marketing authorisation procedures for advanced cancer drugs, and therefore, the total number of factors recorded was eight. The most common number of factors identified by included studies was four (n = 100, 34.6%).
Some studies [98, 101, 106, 109, 111, 126, 127] reported multiple study variances (e.g., for different participant groups). In this case, each reported variance was considered separately, and they ranged from 20.0% to 90.8% (M = 53.4%, SD = 11.6). Ninety studies (31.1%) did not report the total variance explained.
Discussion
This review explored how Q-methodology has been used in healthcare research. Through a comprehensive search and rigorous screening process, 289 studies were identified that used Q-methodology to study topics in healthcare. We captured data on how these studies were conducted, as well as information on the value and applications of Q-methodology to healthcare research.
Use of Q-methodology in healthcare research
In terms of the materials used to conduct Q-methodological studies in healthcare, we found several strategies for developing Q-sets, with literature reviews being most common. Although there was some variation in ranking scale ranges, the majority of studies utilised anchoring based on agreement, indicating most Q-studies in healthcare collect information on how people understand a topic (e.g., compulsory mental healthcare [85] or infant immunisation [128]), rather than prioritisation, as priority and importance anchors had much lower usage.
Face-to-face administration of the Q-sorting task was by far the most common approach to data collection. In many instances, this occurred in conjunction with another method like interviews/post-sorting questions, [129, 130] focus groups/group discussions, [131, 132] a think-aloud task, [23] or observations, [88, 133] to capture information that clarified participants’ placement of the Q-set or provide additional insights into the topic. Perhaps due to the sensitive nature of many aspects of healthcare, mail-out and online forms of collecting Q-data were less common, although several software programs were used for online data collection. In terms of analysis, both PCA and centroid techniques were well represented approaches to factor extraction, while varimax rotation was used in the overwhelming majority of studies for rotation, suggesting a preponderance of exploratory rather than theoretically driven Q-studies in healthcare.
Value of Q-methodology in healthcare research
Healthcare is a complex system, [1, 134, 135] featuring ‘wicked problems’ (e.g., sustainability, patient safety, chronic disease management, and health inequity) that have multiple interacting issues and are socially constructed from the standpoint of different observers [136, 137]. Q-methodology can be used to explore such issues because Q-sorting invites individuals to model their subjectivity by considering multiple issues in relation to each other. Our results highlight that the method is also highly suited for use with different healthcare stakeholders. Q-studies ranged from exploring the perspectives of one stakeholder group (e.g., Intensive care unit nurses [138]) to many (e.g., nurses, alternative therapists, general practitioners, surgeons, allied health professionals, mental health professionals and patients [87]), with approximately one tenth of studies examining consumer perspectives simultaneously with providers. Even where a seemingly homogenous group of participants was involved, multiple perspectives (factors) on the topic were typically uncovered.
Included studies used Q-methodology to tackle a diverse range of healthcare topics, although almost half were broadly in the areas of health professional education, mental healthcare, or nursing practice. Other common topic areas were those that have clear emotional and moral dimensions, including chronic disease, end-of-life care, resource allocation, and gender, sexual and reproductive health. As we and others have noted, [42, 55] these are the kinds of matter considered highly suited to investigation using Q-methodology. In this vein, many authors of articles we reviewed cited the value of using Q-methodology in being able to study complex and contentious topics in which there were likely to be differing opinions [51–54]. Other reasons given for using Q-methodology that are particularly pertinent to healthcare research included the way it allowed minority populations, or participants who often do not have a voice, or find it difficult to participate in other forms of research, to contribute their perspective.
Implications
Studies using Q-methodology in healthcare research have increased over the past 5 years, suggesting a growing interest and acceptance of what was once considered a niche psychological tool [14]. However, the use of Q-methodology in healthcare remains limited when compared to more traditional approaches such as questionnaire surveys. Undoubtedly some healthcare topics are better suited to surveys, but where exploration of a contested or complex issue is required, and holistic understanding of the different perspectives that converge on that topic are desired, Q-methodology should be considered. Moreover, depending on the research questions, Q-methodology may work in tandem with surveys. We reviewed two studies using the emergent design of Q2S, where different perspectives are first identified, using Q-methodology, and then the extent of their distribution in the population is investigated through surveys.
Our review found that Q-methodological research was spread across a large of number of journals. To some extent this reflects the diverse topics that Q has been used to study, however, with very few journals publishing more than one or two studies, it is likely the method remains novel and unfamiliar to many healthcare researchers. The greatest take-up appeared to be in nursing, including nursing education, which is perhaps not surprising given the longstanding and widespread acceptance of interpretive methods in nursing research [139]. A large proportion of Q-methodological research was conducted in the UK, the home of Q, followed by The US, although researchers in countries where English is not the main language have also frequently used the approach, such as South Korea.
For the most part, the studies we reviewed provided information necessary to understand how Q had been applied and the significance of the results. However, there were many occasions of authors not providing all details such as how they derived their Q-set, what types of analyses they performed, and the amount of variance explained. To facilitate increasing use of Q, and publication of Q-methodological studies, we offer a checklist of details that should be included when reporting these studies (Table 4).
Table 4.
Checklist of information to include when reporting a Q-methodological study
| How items/statements for the Q-set were collected |
|---|
| How the statements were refined and reduced to produce the draft and final Q-set |
| The number of statements in the final Q-set |
| What, if any, piloting was done and what the results were |
| The materials used for the Q-sorting task including the ranking scale and anchors |
| How the Q-sorting task was administered |
| What, if any, other methods were used in conjunction with Q-sorting, and how the data captured by these methods was used in relation to Q-data |
| The techniques used for factor extraction and rotation |
| The software programs used to administer and/or analyse the data |
| The information used to decide the number of factors to extract, rotate and interpret |
| The amount of variance explained by the factor solution |
| The processes for interpreting the factors |
| A rich narrative for each factor that explains the shared meaning it represents, supported by Q-set statements, and participant quotes where available |
Strengths and limitations
This review had a comprehensive strategy involving searches of three large academic databases, using a range of keywords associated with both Q-methodology and healthcare. A rigorous approach to reviewing was established though regular discussions between reviewers. Data verification was conducted by one reviewer (KL), who standardised data entry and clarified any inconsistencies by consulting included studies. It is possible that some studies that have used Q-methodology in healthcare were not captured, such as those that used less specific terms (e.g., narratives, viewpoints, or factor analysis) in the title and abstract. This has not limited our capacity to identify a number of trends among included studies. Following scoping review conventions, a formal quality assessment of included articles was not undertaken.
Conclusions
Q-methodology is an approach to studying complex issues that to some extent simplifies complexity by reducing participants’ viewpoints to a smaller number of common perspectives through inverted factor analysis. Nevertheless, the method’s holistic approach to data collection, analysis and interpretation retains the nuances of different perspectives. Arguably, this makes Q-methodology an ideal method for studying the kinds of complex, divisive and ethically fraught issues that are commonplace in healthcare. Our review demonstrated increasing use of the approach in healthcare, however, this research is diffuse, spread across a large number of journals and topic areas, suggesting Q-methodology is still fairly novel. We have highlighted commonalities in how the method has been used, areas of application, and the potential value of the approach, which may lead to increased use of Q-methodology in the future.
Supplementary Information
Additional file 1. PRISMA-ScR checklist.
Additional file 2. Keyword search in Web of Science Medline.
Additional file 3. Full list of studies included in the review and details of data items charted.
Acknowledgements
Not applicable.
Abbreviations
- PRISMA
Preferred Reporting Items for Systematic Review and Meta-analyses
- Q2S
Q-methodology to survey
- UK
United Kingdom
- US
United States
Authors’ contributions
KC had the original idea for the study, completed the search, title/abstract screen, and was involved in data extraction and drafting the manuscript. KL completed a subset of the title/abstract screen, and was involved in data extraction and drafting the manuscript. WW, KG and HMN were involved in data extraction. LAE and JB provided intellectual input into the manuscript. All authors critically revised and approved the final manuscript.
Funding
JB’s work is funded by multiple National Health and Medical Research Council grants: NHMRC Partnership Grant for Health Systems Sustainability (9100002); NHMRC Centre of Research Excellence Grant (APP1135048); NHMRC Investigator Grant (APP1176620) and NHMRC Partnership Project (APP1134459).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Super factors are the resulting factors from a second order factor analysis, in which the first order factor arrays (ideal Q-sorts computed for each factor) are considered Q sorts.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Kate Churruca and Kristiana Ludlow are joint lead co-authors
References
- 1.Braithwaite J, Churruca K, Ellis LA, Long J, Clay-Williams R, Damen N, et al. Complexity Science in Healthcare – Aspirations, Approaches, Applications and Accomplishments: A White Paper. Sydney: Australian Institute of Health Innovation, Macquarie University; 2017. ISBN: 978-1-74138-456-7.
- 2.Atwal A, Caldwell K. Do all health and social care professionals interact equally: A study of interactions in multidisciplinary teams in the United Kingdom. Scand J Caring Sci. 2005;19(3):268–273. doi: 10.1111/j.1471-6712.2005.00338.x. [DOI] [PubMed] [Google Scholar]
- 3.McDonald KM, Sundaram V, Bravata DM, Lewis R, Lin N, Kraft SA, et al. Closing the quality gap: A critical analysis of quality improvement strategies (Vol. 7: Care Coordination; Technical Review No. 9). Rockville: US Agency for Healthcare Research and Quality; 2007. [PubMed]
- 4.Crawford MJ, Rutter D, Manley C, Weaver T, Bhui K, Fulop N, et al. Systematic review of involving patients in the planning and development of health care. BMJ. 2002;325(7375):1263. doi: 10.1136/bmj.325.7375.1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sturmberg JP, O’Halloran DM, Martin CM. Understanding health system reform – A complex adaptive systems perspective. J Eval Clin Pract. 2012;18(1):202–8. 10.1111/j.1365-2753.2011.01792.x. [DOI] [PubMed]
- 6.Saha S, Beach MC, Cooper LA. Patient centeredness, cultural competence and healthcare quality. J Natl Med Assoc. 2008;100(11):1275–1285. doi: 10.1016/s0027-9684(15)31505-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Braithwaite J, Hibbert PD, Jaffe A, et al. Quality of health care for children in Australia, 2012–2013. JAMA. 2018;319(11):1113–1124. doi: 10.1001/jama.2018.0162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cleary PD, Edgman-Levitan S. Health care quality: Incorporating consumer perspectives. JAMA. 1997;278(19):1608–1612. doi: 10.1001/jama.1997.03550190072047. [DOI] [PubMed] [Google Scholar]
- 9.Petrie KJ, Weinman J. Patients’ perceptions of their illness: The dynamo of volition in health care. Curr Dir Psychol Sci. 2012;21(1):60–65. doi: 10.1177/0963721411429456. [DOI] [Google Scholar]
- 10.Bryman A. Social Research Methods. 4th ed. Oxford: Oxford University Press; 2016.
- 11.Kitzinger J. Qualitative research: Introducing focus groups. BMJ. 1995;311(7000):299–302. doi: 10.1136/bmj.311.7000.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marks DF, Yardley L. Research Methods for Clinical and Health Psychology. London: SAGE Ltd; 2004.
- 13.Brown SR. The history and principles of Q methodology in psychology and the social sciences. In: British Psychological Society symposium on “A Quest for a Science of Subjectivity: The Lifework of William Stephenson”. London: University of London; 1997.
- 14.Watts S, Stenner P. Doing Q Methodological Research: Theory, Method & Interpretation. London: SAGE Publications; 2012.
- 15.Stainton RR. Q methodology. In: Smith JA, Harré R, Langenhove LV, editors. Rethinking Methods in Psychology. London, UK: SAGE Publications; 1995. pp. 178–192. [Google Scholar]
- 16.McKeown B, Thomas DB. Q Methodology. Thousand Oaks, CA: SAGE Publications; 2013. [Google Scholar]
- 17.Paige JB, Morin KH. Q-sample construction: A critical step for a Q-methodological study. West J Nurs Res. 2014;38(1):96–110. doi: 10.1177/0193945914545177. [DOI] [PubMed] [Google Scholar]
- 18.Tinsley HEA, Kass RA. The latent structure of the need satisfying properties of leisure activities. J Leis Res. 1979;11(4):278–291. doi: 10.1080/00222216.1979.11969406. [DOI] [Google Scholar]
- 19.Comrey A, Lee H. Interpretation and application of factor analytic results. In: Comrey A, Lee H, editors. A First Course in Factor Analysis. New York, NY: Psychology Press; 1992. pp. 240–262. [Google Scholar]
- 20.Eccles DW, Arsal G. The think aloud method: What is it and how do I use it? Qual Res Sport Exerc Health. 2017;9(4):514–531. doi: 10.1080/2159676X.2017.1331501. [DOI] [Google Scholar]
- 21.Ludlow K, Churruca K, Mumford V, Ellis LA, Braithwaite J. Staff members’ prioritisation of care in residential aged care facilities: A Q methodology study. BMC Health Serv Res. 2020;20(1):423. doi: 10.1186/s12913-020-05127-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ludlow K, Churruca K, Ellis LA, Mumford V, Braithwaite J. Family members’ prioritisation of care in residential aged care facilities: A case for individualised care. J Clin Nur. 2020;29:3272–85. 10.1111/jocn.15352. [DOI] [PubMed]
- 23.Innes K, Gillies K, Cotton S, Campbell M. Q methodology with cognitive interviewing to rank the importance of informational items in a patient information leaflet. Trials. 2015;16(Suppl 2):P76. doi: 10.1186/1745-6215-16-S2-P76. [DOI] [Google Scholar]
- 24.Stephenson W. Technique of factor analysis. Nature. 1935;136(3434):297. 10.1038/136297b0.
- 25.Stephenson W. The Study of Behavior: Q-Technique and its Methodology. Chicago, IL: University of Chicago Press; 1953. [Google Scholar]
- 26.Brown SR. Political Subjectivity: Applications of Q methodology in Political Science. New Haven, CT: Yale University Press; 1980. [Google Scholar]
- 27.Valenta AL, Wigger U. Q-methodology: Definition and application in health care informatics. J Am Med Inform Assoc. 1997;4(6):501–510. doi: 10.1136/jamia.1997.0040501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cross RM. Exploring attitudes: The case for Q methodology. Health Educ Res. 2005;20(2):206–213. doi: 10.1093/her/cyg121. [DOI] [PubMed] [Google Scholar]
- 29.Akhtar-Danesh N, Baumann A, Cordingley L. Q-methodology in nursing research: A promising method for the study of subjectivity. West J Nurs Res. 2008;30(6):759–773. doi: 10.1177/0193945907312979. [DOI] [PubMed] [Google Scholar]
- 30.Simons J. An introduction to Q methodology. Nurse Res. 2013;20(3):28–32. doi: 10.7748/nr2013.01.20.3.28.c9494. [DOI] [PubMed] [Google Scholar]
- 31.Baker R, Wildman J, Mason H, Donaldson C. Q-ing for health—a new approach to eliciting the public’s views on health care resource allocation. Health Econ. 2014;23(3):283–297. doi: 10.1002/hec.2914. [DOI] [PubMed] [Google Scholar]
- 32.van Exel J, Baker R, Mason H, Donaldson C, Brouwer W. Public views on principles for health care priority setting: Findings of a European cross-country study using Q methodology. Soc Sci Med. 2015;126:128–137. doi: 10.1016/j.socscimed.2014.12.023. [DOI] [PubMed] [Google Scholar]
- 33.Alderson S, Foy R, Bryant L, Ahmed S, House A. Using Q-methodology to guide the implementation of new healthcare policies. BMJ Qual Saf. 2018;27:737–742. doi: 10.1136/bmjqs-2017-007380. [DOI] [PubMed] [Google Scholar]
- 34.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169(7):467–73. 10.7326/M18-0850. [DOI] [PubMed]
- 36.McHugh ML. Interrater reliability: The kappa statistic. Biochem Med (Zagreb). 2012;22(3):276–82. [PMC free article] [PubMed]
- 37.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ahmed S, Yi H, Dong D, Zhu J, Jafri H, Rashid Y, et al. Interpretations of autonomous decision-making in antenatal genetic screening among women in China, Hong Kong and Pakistan. Eur J Hum Genet. 2018;26(4):495–504. doi: 10.1038/s41431-017-0091-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Paige JB, Morin KH. Using Q-methodology to reveal nurse educators’ perspectives about simulation design. Clin Simul Nurs. 2015;11(1):11–19. doi: 10.1016/j.ecns.2014.09.010. [DOI] [Google Scholar]
- 40.Roshanai AH, Lampic C, Ingvoldstad C, Askmalm MS, Bjorvatn C, Rosenquist R, et al. What information do cancer genetic counselees prioritize? J Genet Couns. 2012;21(4):510–526. doi: 10.1007/s10897-011-9409-2. [DOI] [PubMed] [Google Scholar]
- 41.Andrews CS. Defining and exploring modesty in Jewish American women. J Relig Health. 2011;50(4):818–834. doi: 10.1007/s10943-010-9435-7. [DOI] [PubMed] [Google Scholar]
- 42.Askay SW, Stricklin M, Carrougher GJ, Patterson DR, Klein MB, Esselman PC, et al. Using QMethodology to identify reasons for distress in burn survivors postdischarge. J Burn Care Res. 2009;30(1):83–91. doi: 10.1097/BCR.0b013e3181921f42. [DOI] [PubMed] [Google Scholar]
- 43.Chun KH, Park E. Diversity of emotional intelligence among nursing and medical students. Osong Public Health Res. 2016;7(4):261–265. doi: 10.1016/j.phrp.2016.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dennis KE. Real and ideal hospital work environments in juxtaposition. West J Nurs Res. 1991;13(6):761–775. doi: 10.1177/019394599101300607. [DOI] [PubMed] [Google Scholar]
- 45.Dick K, Gleeson K, Johnstone L, Weston C. Staff beliefs about why people with learning disabilities self-harm: A Q-methodology study. Br J Learn Disabil. 2011;39(3):233–242. doi: 10.1111/j.1468-3156.2010.00660.x. [DOI] [Google Scholar]
- 46.Jung SK, Chon MY. Subjectivity toward transition experience of the patient who moves from intensive care unit to a general ward. Int J Appl Eng Res. 2014;9(24):29637–29642. [Google Scholar]
- 47.Kindsvatter A, Osborn C, Bubenzer D, Duba J. Client perceptions of pretreatment change. J Couns Dev. 2010;88(4):449–456. doi: 10.1002/j.1556-6678.2010.tb00045.x. [DOI] [Google Scholar]
- 48.Liu CC. Using Q methodology to classify users’ value types on hospital websites. Int J Technol Policy Mana. 2013;13(2):190–205. doi: 10.1504/IJTPM.2013.053097. [DOI] [Google Scholar]
- 49.Wiechman S, Stricklin M, Carrougher GJ, Patterson DR, Klein MB, Esselman PC, et al. Using QMethodology to identify reasons for distress in burn survivors postdischarge. J Burn Care Res. 2009;30(1):83–91. doi: 10.1097/BCR.0b013e3181921f42. [DOI] [PubMed] [Google Scholar]
- 50.Farrimond H. A typology of vaping: Identifying differing beliefs, motivations for use, identity and political interest amongst e-cigarette users. Int J Drug Policy. 2017;48:81–90. doi: 10.1016/j.drugpo.2017.07.011. [DOI] [PubMed] [Google Scholar]
- 51.Gidman W, Day J, Hassell K, Payne K. Delivering health care through community pharmacies: Are working conditions deterring female pharmacists’ participation? J Health Serv Res Policy. 2009;14(3):141–149. doi: 10.1258/jhsrp.2009.008077. [DOI] [PubMed] [Google Scholar]
- 52.Dean R, Siddiqui S, Beesley F, Fox J, Berry K. Staff perceptions of borderline personality disorder and recovery: A Q-sort method approach. Br J Clin Psychol. 2018;57(4):473–490. doi: 10.1111/bjc.12180. [DOI] [PubMed] [Google Scholar]
- 53.Grimshaw P, McGowan L, McNichol E. An extra care community’s perceived priorities for ‘whole system’ relationships: A Q-methodological study. Health Soc Care Community. 2017;25(3):1169–1180. doi: 10.1111/hsc.12417. [DOI] [PubMed] [Google Scholar]
- 54.Cross-Sudworth F, Williams A, Herron-Marx S. Maternity services in multi-cultural Britain: Using Q methodology to explore the views of first- and second-generation women of Pakistani origin. Midwifery. 2011;27(4):458–468. doi: 10.1016/j.midw.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 55.Butler H, Hare D, Walker S, Wieck A, Wittkowski A. The acceptability and feasibility of the Baby Triple P Positive Parenting Programme on a mother and baby unit: Q-methodology with mothers with severe mental illness. Arch Womens Ment Health. 2014;17(5):455–463. doi: 10.1007/s00737-014-0429-4. [DOI] [PubMed] [Google Scholar]
- 56.Clarke DJ, Holt J. Understanding nursing practice in stroke units: A Q-methodological study. Disabil Rehabil. 2015;37(20):1870–1880. doi: 10.3109/09638288.2014.986588. [DOI] [PubMed] [Google Scholar]
- 57.Grijpma JW, Tielen M, van Staa AL, Maasdam L, van Gelder T, Berger SP, et al. Kidney transplant patients’ attitudes towards self-management support: A Q-methodological study. Patient Educ Couns. 2016;99(5):836–843. doi: 10.1016/j.pec.2015.11.018. [DOI] [PubMed] [Google Scholar]
- 58.Honey S, Bryant LD, Murray J, Hill K, House A. Differences in the perceived role of the healthcare provider in delivering vascular health checks: A Q methodology study. BMC Fam Pract. 2013;14:172. doi: 10.1186/1471-2296-14-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ho GW, Gross DA. Differentiating physical discipline from abuse: Q findings from Chinese American mothers and pediatric nurses. Child Abuse Negl. 2015;43:83–94. doi: 10.1016/j.chiabu.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 60.Daniels VJ, Kassam N. Impact of personal goals on the internal medicine R4 subspecialty match: A Q methodology study. BMC Med Educ. 2013;13:171. doi: 10.1186/1472-6920-13-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Day JC, Bentall RP, Warner S. Schizophrenic patients’ experiences of neuroleptic medication: A Q-methodological investigation. Acta Psychiatr Scand. 1996;93(5):397–402. doi: 10.1111/j.1600-0447.1996.tb10666.x. [DOI] [PubMed] [Google Scholar]
- 62.Jueng R-N, Huang S-H, Li T-P, Liang H-Y, Huang C-M. Application of a Q method study to understanding nurses’ perspective of adopting evidence-based nursing. Asian Nurs Res. 2017;11(4):253–260. doi: 10.1016/j.anr.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 63.Hammami MM, Al Gaai E, Hammami S, Attala S. Exploring end of life priorities in Saudi males: Usefulness of Q-methodology. BMC Palliat Care. 2015;14:66. doi: 10.1186/s12904-015-0064-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.White HK, Corazzini K, Twersky J, Buhr G, McConnell E, Weiner M, et al. Prioritizing culture change in nursing homes: Perspectives of residents, staff, and family members. J Am Geriatr Soc. 2012;60(3):525–531. doi: 10.1111/j.1532-5415.2011.03840.x. [DOI] [PubMed] [Google Scholar]
- 65.Flurey CA, Morris M, Pollock J, Richards P, Hughes R, Hewlett S. A Q-methodology study of flare help-seeking behaviours and different experiences of daily life in rheumatoid arthritis. BMC Musculoskelet Disord. 2014;15(1). 10.1186/1471-2474-15-364. [DOI] [PMC free article] [PubMed]
- 66.Jedeloo S, van Staa A, Latour JM, van Exel N. Preferences for health care and self-management among Dutch adolescents with chronic conditions: A Q-methodological investigation. Int J Nurs Stud. 2010;47(5):593–603. doi: 10.1016/j.ijnurstu.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 67.Cross R. Accident and Emergency nurses’ attitudes towards health promotion. J Adv Nurs. 2005;51(5):474–483. doi: 10.1111/j.1365-2648.2005.03517.x. [DOI] [PubMed] [Google Scholar]
- 68.Ha EH. How clinical nurses in South Korea perceive the status of the nursing profession: A Q-methodological approach. Int J Nurs Pract. 2017;23(2). 10.1111/ijn.12516. [DOI] [PubMed]
- 69.Bang HY, Yeun EJ, Ham E, Jeon M, An JH. Perceptions about cancer-related fatigue among cancer patients using Q methodology. Eur J Oncol Nurs. 2016;20:64–70. doi: 10.1016/j.ejon.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 70.Ho GWK, Gross DA. Pediatric nurses’ differentiations between acceptable and unacceptable parent discipline behaviors: A Q-study. J Pediatr Health Care. 2015;29(3):255–264. doi: 10.1016/j.pedhc.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 71.Jeong E, Chang SO. Exploring nurses’ recognition of delirium in the elderly by using Q-methodology. Jpn J Nurs Sci. 2017 doi: 10.1111/jjns.12199. [DOI] [PubMed] [Google Scholar]
- 72.Killam LA, Montgomery P, Raymond JM, Mossey S, Timmermans KE, Binette J. Unsafe clinical practices as perceived by final year baccalaureate nursing students: Q methodology. BMC Nurs. 2012;11. 10.1186/1472-6955-11-26. [DOI] [PMC free article] [PubMed]
- 73.Kim IJ, Kim SH, Sohn SK. Societal perceptions of male nurses in South Korea: A Q-methodological study. Jpn J Nurs Sci. 2017;14(3):219–230. doi: 10.1111/jjns.12152. [DOI] [PubMed] [Google Scholar]
- 74.Dziopa F, Ahern K. Three different ways mental health nurses develop quality therapeutic relationships. Issues Ment Health Nurs. 2009;30(1):14–22. doi: 10.1080/01612840802500691. [DOI] [PubMed] [Google Scholar]
- 75.Barker JH. Q-methodology: An alternative approach to research in nurse education. Nurse Educ Today. 2008;28(8):917–925. doi: 10.1016/j.nedt.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 76.Hensel D, Cooper R, Craney N. Operating room personnel viewpoints about certified registered nurse anesthetists. West J Nurs Res. 2018;40(2):242–256. doi: 10.1177/0193945916682730. [DOI] [PubMed] [Google Scholar]
- 77.Whyte F, Smith LN. An exploratory study of the health-care needs of the adolescent with cancer. J Res Nurs. 1997;2(1):59–69. doi: 10.1177/136140969700200112. [DOI] [Google Scholar]
- 78.Codjoe L, Byrne M, Lister M, McGuire P, Valmaggia L. Exploring perceptions of “wellness” in black ethnic minority individuals at risk of developing psychosis. Behav Cogn Psychother. 2013;41(2):144–161. doi: 10.1017/s1352465812000707. [DOI] [PubMed] [Google Scholar]
- 79.Dudley R, Siitarinen J, James I, Dodgson G. What do people with psychosis think caused their psychosis? A Q methodology study. Behav Cogn Psychother. 2009;37(1):11–24. doi: 10.1017/S1352465808004955. [DOI] [PubMed] [Google Scholar]
- 80.Merrick S, Farrell D. Head and neck cancer patients’ experiences of percutaneous endoscopic gastrostomy feeding: A Q-methodology study. Eur J Cancer Care. 2012;21(4):493–504. doi: 10.1111/j.1365-2354.2012.01326.x. [DOI] [PubMed] [Google Scholar]
- 81.Absalom-Hornby V, Hare DJ, Gooding P, Tarrier N. Attitudes of relatives and staff towards family intervention in forensic services using Q methodology. J Psychiatr Ment Health Nurs. 2012;19(2):162–173. doi: 10.1111/j.1365-2850.2011.01770.x. [DOI] [PubMed] [Google Scholar]
- 82.Ahmed S, Jafri H, Rashid Y, Yi H, Dong D, Zhu J, et al. Autonomous decision-making for antenatal screening in Pakistan: Views held by women, men and health professionals in a low–middle income country. Eur J Hum Genet. 2019;27(6):848–856. doi: 10.1038/s41431-019-0353-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cramm JM, Leensvaart L, Berghout M, Van Exel J. Exploring views on what is important for patient-centred care in end-stage renal disease using Q methodology. BMC Nephrol. 2015;16(1). 10.1186/s12882-015-0071-z. [DOI] [PMC free article] [PubMed]
- 84.Hazen ACM, Wal AW, Sloeserwij VM, Zwart DLM, Gier JJ, Wit NJ, et al. Controversy and consensus on a clinical pharmacist in primary care in the Netherlands. Int J Clin Pharm. 2016;38(5):1250–1260. doi: 10.1007/s11096-016-0360-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Diseth RR, Bogwald K-P, Hoglend PA. Attitudes among stakeholders towards compulsory mental health care in Norway. Int J Law Psychiatry. 2011;34(1):1–6. doi: 10.1016/j.ijlp.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 86.Eaton E. What is a good birth? Using Q method to explore the diversity of attitudes about good birth. J Prenat Perinat Psychol Health. 2014;28(3):147–173. [Google Scholar]
- 87.Eccleston C, Williams AC, Stainton RW. Patients’ and professionals’ understandings of the causes of chronic pain: Blame, responsibility and identity protection. Soc Sci Med. 1997;45(5):699–709. doi: 10.1016/S0277-9536(96)00404-2. [DOI] [PubMed] [Google Scholar]
- 88.Fleming A, Kydd A. What makes a nursing home homely? A Scottish based study, using Q methodology of the perceptions of staff, residents and significant others. J Res Nurs. 2018;23(2–3):141–158. doi: 10.1177/1744987118757837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Fokkema JPI, Scheele F, Westerman M, Van Exel J, Scherpbier AJJA, Van Der Vleuten CPM, et al. Perceived effects of innovations in postgraduate medical education: A Q study focusing on workplace-based assessment. Acad Med. 2014;89(9):1259–1266. doi: 10.1097/ACM.0000000000000394. [DOI] [PubMed] [Google Scholar]
- 90.Hackert MQN, Brouwer WBF, Hoefman RJ, van Exel J. Views of older people in the Netherlands on wellbeing: A Q-methodology study. Soc Sci Med. 2019;240:112535. doi: 10.1016/j.socscimed.2019.112535. [DOI] [PubMed] [Google Scholar]
- 91.Hestdal T, Skorpen F. Experiences of suffering among elderly hip-fracture patients during the preoperative period: patients’ and nurse’s perspective. Scand J Caring Sci. 2020;34(2):409–19. 10.1111/scs.12742. [DOI] [PubMed]
- 92.James M, Warner S. Coping with their lives - women, learning disabilities, self-harm and the secure unit: A Q-methodological study. Br J Learn Disabil. 2005;33(3):120–127. doi: 10.1111/j.1468-3156.2005.00338.x. [DOI] [Google Scholar]
- 93.LaFleur RC, Truscott S, Graybill E, Crenshaw M, Crimmins D. Improving culturally congruent health care for children with disabilities: Stakeholder perspectives of cultural competence training in an interdisciplinary leadership training program. J Transcult Nurs. 2018;29(1):101–111. doi: 10.1177/1043659617699065. [DOI] [PubMed] [Google Scholar]
- 94.McHugh N, Baker RM, Mason H, Williamson L, Van Exel J, Deogaonkar R, et al. Extending life for people with a terminal illness: A moral right and an expensive death? Exploring societal perspectives. BMC Med Ethics. 2015;16(1). 10.1186/s12910-015-0008-x. [DOI] [PMC free article] [PubMed]
- 95.McIntosh CJ, Westbrook J, Sheldrick R, Surr C, Hare DJ. The feasibility of Dementia Care Mapping (DCM) on a neurorehabilitation ward. Neuropsychol Rehabil. 2012;22(6):920–941. doi: 10.1080/09602011.2012.711642. [DOI] [PubMed] [Google Scholar]
- 96.McParland J, Hezseltine L, Serpell M, Eccleston C, Stenner P. An investigation of constructions of justice and injustice in chronic pain: A Q-methodology approach. J Health Psychol. 2011;16(6):873–883. doi: 10.1177/1359105310392417. [DOI] [PubMed] [Google Scholar]
- 97.Morecroft C, Cantrill J, Tully M. Patients’ and general practitioners’ views of what constitutes appropriate hypertension management. J Health Serv Res Policy. 2005;10(2):91–96. doi: 10.1258/1355819053559119. [DOI] [PubMed] [Google Scholar]
- 98.Morera T, Bucci S, Randal C, Barrett M, Pratt D. Exploring views about mindfulness groups for voice-hearing from the perspective of service users and staff: A Q-methodology study. Psychother Res. 2017;27(2):179–188. doi: 10.1080/10503307.2015.1085657. [DOI] [PubMed] [Google Scholar]
- 99.Perz J, Ussher JM, Gilbert E. Constructions of sex and intimacy after cancer: Q methodology study of people with cancer, their partners, and health professionals. BMC Cancer. 2013;13. 10.1186/1471-2407-13-270. [DOI] [PMC free article] [PubMed]
- 100.Protiére C, Baker R, Genre D, Goncalves A, Viens P. Marketing authorization procedures for advanced cancer drugs: exploring the views of patients, oncologists, healthcare decision makers, and citizens in france. Med Decis Making. 2017;37(5):555–566. doi: 10.1177/0272989X17691953. [DOI] [PubMed] [Google Scholar]
- 101.Protière C, Spire B, Mora M, Poizot-Martin I, Préau M, Doumergue M, et al. Patterns of patient and healthcare provider viewpoints regarding participation in HIV cure-related clinical trials. Findings from a multicentre French survey using Q methodology (ANRS-APSEC). PLoS ONE. 2017;12(11):e0187489. 10.1371/journal.pone.0187489 [DOI] [PMC free article] [PubMed]
- 102.Stenner P, Cross V, McCrum C, McGowan J, Defever E, Lloyd P, et al. Self-management of chronic low back pain: Four viewpoints from patients and healthcare providers. Health Psychol Open. 2015;2(2). 10.1177/2055102915615337. [DOI] [PMC free article] [PubMed]
- 103.Westbrook JL, McIntosh CJ, Sheldrick R, Surr C, Hare DJ. Validity of Dementia Care Mapping on a neuro-rehabilitation ward: Q-methodology with staff and patients. Disabil Rehabil. 2013;35(19):1652–1659. doi: 10.3109/09638288.2012.748839. [DOI] [PubMed] [Google Scholar]
- 104.Zhu N, Xu P, Ma J, Liang Y, Xu X, Li J. Patients, caregivers and nurses’ attitudes toward patients’ participation in knee and hip joint replacement pain management: A Q-methodology study. Contemp Nurse. 2019;55(6):507–21. 10.1080/10376178.2019.1666019. [DOI] [PubMed]
- 105.Banna S, Hasan H, Dawson P. Understanding the diversity of user requirements for interactive online health services. Int J Healthc Technol Manag. 2016;15(3):253–271. doi: 10.1504/IJHTM.2016.078371. [DOI] [Google Scholar]
- 106.Evans KL, Girdler SJ, Falkmer T, Richmond JE, Wagman P, Millsteed J, et al. Viewpoints of working sandwich generation women and occupational therapists on role balance strategies. Scand J Occup Ther. 2017;24(5):366–382. doi: 10.1080/11038128.2016.1250814. [DOI] [PubMed] [Google Scholar]
- 107.Hasan H, Moleche J, Banna S. Australian online public information systems: A user-centred study of an evolving public health website. Australas J Inf Syst. 2012;17(2):5–19. [Google Scholar]
- 108.Choi B, Lee NB. The types and characteristics of clients’ perceptions of the bonny method of guided imagery and music. J Music Ther. 2014;51(1):64–102. 10.1093/jmt/thu001. [DOI] [PubMed]
- 109.Elstein AS, Van Pelt JD. Dimensions in the perception of psychiatric patients by hospital staff. J Consult Psychol. 1966;30(3):213–218. doi: 10.1037/h0023384. [DOI] [PubMed] [Google Scholar]
- 110.Landeen J, Pierazzo J, Akhtar-Danesh N, Baxter P, van Eijk S, Evers C. Exploring student and faculty perceptions of clinical simulation: A Q-sort study. J Nurs Educ. 2015;54(9):485–491. doi: 10.3928/01484834-20150814-02. [DOI] [PubMed] [Google Scholar]
- 111.Leary J, Gallagher T, Carson J, Fagin L, Bartlett H, Brown D. Stress and coping strategies in community psychiatric nurses: A Q-methodological study. J Adv Nurs. 1995;21(2):230–237. doi: 10.1111/j.1365-2648.1995.tb02519.x. [DOI] [PubMed] [Google Scholar]
- 112.Prabakaran R, Seymour S, Moles DR, Cunningham SJ. Motivation for orthodontic treatment investigated with Q-methodology: Patients’ and parents’ perspectives. Am J Orthod Dentofacial Orthop. 2012;142(2):213–220. doi: 10.1016/j.ajodo.2012.03.026. [DOI] [PubMed] [Google Scholar]
- 113.Tang X, Tong Q, Li Z, Chen Z, Weng M, Zhang X, et al. Difference and commonness among CLP, NON-CLP patients and their parents seeking for orthodontic treatment: A questionnaire applying Q methodology to investigate motives. Patient Prefer Adherence. 2019;13:2047–2060. doi: 10.2147/PPA.S224254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lister M, Gardner D. Engaging hard to engage clients: A Q methodological study involving clinical psychologists. Psychol Psychother. 2006;79(3):419–443. doi: 10.1348/147608305X59949. [DOI] [PubMed] [Google Scholar]
- 115.Gamiet S, Rowe M. The role of rehabilitation care workers in South African healthcare: A Q-methodological study. Afr J Disabil. 2019;8:537. doi: 10.4102/ajod.v8i0.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Herron-Marx S, Williams A, Hicks C. A Q methodology study of women’s experience of enduring postnatal perineal and pelvic floor morbidity. Midwifery. 2007;23(3):322–334. doi: 10.1016/j.midw.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 117.Adderley H, Wittkowski A, Calam R, Gregg L. Adult mental health practitioner beliefs about psychosis, parenting, and the role of the practitioner: A Q methodological investigation. Psychol Psychother. 2020;93(4):657–73. 10.1111/papt.12249. [DOI] [PMC free article] [PubMed]
- 118.Leggat SG, Phillips B, Pearce P, Dawson M, Schulz D, Smith J. Clinical supervision for allied health staff: Necessary but not sufficient. Aust Health Rev. 2016;40(4):431–437. doi: 10.1071/AH15080. [DOI] [PubMed] [Google Scholar]
- 119.Wong W, Eiser AR, Mrtek RG, Heckerling PS. By-person factor analysis in clinical ethical decision making: Q methodology in end-of-life care decisions. Am J Bioeth. 2004;4(3):W8–W22. doi: 10.1080/15265160490505506. [DOI] [PubMed] [Google Scholar]
- 120.Bradley S, Alderson S, Ford AC, Foy R. General practitioners’ perceptions of irritable bowel syndrome: A Q-methodological study. Fam Pract. 2018;35(1):74–79. doi: 10.1093/fampra/cmx053. [DOI] [PubMed] [Google Scholar]
- 121.Skorpen F, Thorsen AA, Forsberg C, Rehnsfeldt AW. Suffering related to dignity among patients at a psychiatric hospital. Nurs Ethics. 2014;21(2):148–162. doi: 10.1177/0969733013493216. [DOI] [PubMed] [Google Scholar]
- 122.Roberts JK, Sparks MA, Lehrich RW. Medical student attitudes toward kidney physiology and nephrology: A qualitative study. Ren Fail. 2016;38(10):1683–1693. doi: 10.1080/0886022X.2016.1230459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Purvis LJ, Cropley M. The psychological contracts of National Health Service nurses. J Nurs Manag. 2003;11(2):107–120. doi: 10.1046/j.1365-2834.2003.00357.x. [DOI] [PubMed] [Google Scholar]
- 124.Reckers-Droog V, Jansen M, Bijlmakers L, Baltussen R, Brouwer W, van Exel J. How does participating in a deliberative citizens panel on healthcare priority setting influence the views of participants? Health Policy. 2020;124(2),143–51. 10.1016/j.healthpol.2019.11.011. [DOI] [PubMed]
- 125.Corr S, Neill G, Turner A. Comparing an occupational therapy definition and consumer’s experiences: A Q methodology study. Br J Occup Ther. 2005;68(8):338–46. 10.1177/030802260506800802.
- 126.Osborne R, Janson C, Black L, Jensen GM. Motivations to pursue physical therapy residency training: A Q-methodology study of stakeholder Perspectives. Phys Ther. 2020;100(1):57–72. 10.1093/ptj/pzz142. [DOI] [PubMed]
- 127.Ghanbari A, Hasandoost F, Lyili EK, Khomeiran RT, Momeni M. Assessing emergency nurses’ clinical competency: An exploratory factor analysis study. Iran J Nurs Midwifery Res. 2017;22(4):280–6. 10.4103/1735-9066.212990. [DOI] [PMC free article] [PubMed]
- 128.Harvey H, Good J, Mason J, Reissland N. A Q-methodology study of parental understandings of infant immunisation: Implications for health-care advice. J Health Psychol. 2015;20(11):1451–1462. doi: 10.1177/1359105313513622. [DOI] [PubMed] [Google Scholar]
- 129.Hill SR, Mason H, Poole M, Vale L, Robinson L. What is important at the end of life for people with dementia? The views of people with dementia and their carers. Int J Geriatr Psychiatry. 2017;32(9):1037–1045. doi: 10.1002/gps.4564. [DOI] [PubMed] [Google Scholar]
- 130.Reid KJ, Swift A, Mehanna H. A Q methodology study to investigate the experiences of head and neck cancer patients from diagnosis to 1 year. Eur J Cancer Care. 2017;26(6):e12694. doi: 10.1111/ecc.12694. [DOI] [PubMed] [Google Scholar]
- 131.Luymes CH, Boelhouwer NJ, Poortvliet RK, de Ruijter W, Reis R, Numans ME. Understanding deprescribing of preventive cardiovascular medication: A Q-methodology study in patients. Patient Prefer Adherence. 2017;11:975–984. doi: 10.2147/PPA.S131625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Vendetti-Hastie S, Dowdall-Smith S, Montgomery P. Northern healthcare students’ perceptions of hand hygiene in community practice. Can J Infect Control. 2015;30(4):218–24.
- 133.van Staa A. Unraveling triadic communication in hospital consultations with adolescents with chronic conditions: The added value of mixed methods research. Patient Educ Couns. 2011;82(3):455–464. doi: 10.1016/j.pec.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 134.Braithwaite J, Churruca K, Long JC, Ellis LA, Herkes J. When complexity science meets implementation science: A theoretical and empirical analysis of systems change. BMC Med. 2018;16(1):63. doi: 10.1186/s12916-018-1057-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Thompson DS, Fazio X, Kustra E, Patrick L, Stanley D. Scoping review of complexity theory in health services research. BMC Health Serv Res. 2016;16(1):1–16. doi: 10.1186/s12913-016-1343-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Blackman T, Greene A, Hunter DJ, McKee L, Elliott E, Harrington B, et al. Performance assessment and wicked problems: The case of health inequalities. Public Policy Adm. 2006;21(2):66–80. doi: 10.1177/095207670602100206. [DOI] [Google Scholar]
- 137.Westbrook JI, Braithwaite J, Georgiou A, Ampt A, Creswick N, Coiera E, et al. Multimethod evaluation of information and communication technologies in health in the context of wicked problems and sociotechnical theory. JAMIA. 2007;14(6):746–755. doi: 10.1197/jamia.M2462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Lobo VM, Fisher A, Baumann A, Akhtar-Danesh N. Effective retention strategies for midcareer critical care nurses: A Q-method study. Nurs Res. 2012;61(4):300–308. doi: 10.1097/NNR.0b013e31825b69b1. [DOI] [PubMed] [Google Scholar]
- 139.Munhall PL. Philosophical ponderings on qualitative research methods in nursing. Nurs Sci Q. 1989;2(1):20–28. doi: 10.1177/089431848900200109. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. PRISMA-ScR checklist.
Additional file 2. Keyword search in Web of Science Medline.
Additional file 3. Full list of studies included in the review and details of data items charted.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.