Abstract
Purpose
Spherical orthokeratology and soft multifocal contact lenses are commonly used for myopia control and correction, but have been shown to increase spherical aberration, coma and total higher order root mean square (HORMS) aberrations. There are limited myopia control contact lens options for patients with moderate to high astigmatism. The purpose of this study was to quantify changes in higher order aberrations (HOA) in myopic astigmatic eyes fitted with toric orthokeratology (TOK) and soft toric multifocal (STM) contact lenses.
Methods
Ocular wavefront aberrations were measured in both eyes of 30 adult subjects and are reported through the 6th radial order over a 5 mm, dilated pupil. All eyes met refractive criteria of myopia (−5.00 D to plano) and cylinder (−3.50 to −1.25 D). Three measurements were taken at baseline and after 10 ± 2 days of lens wear (TOK, STM). Sixteen subjects achieved logMAR high contrast visual acuity of 0.30 or better in both eyes and were included in this analysis. Repeated measures analysis of variance and post-hoc paired t-tests were used, as appropriate, with Benjamini-Hochberg correction.
Results
HORMS, spherical aberration (C12), and coma RMS (C7, C8) increased with TOK (0.641 [0.222], 0.409 [0.157], 0.426 [0.187] μm, respectively) and STM (0.481 [0.107], 0.223 [0.139], 0.320 [0.130] μm, respectively) from baseline (all p < 0.001). TOK was elevated compared to STM for HORMS (p = 0.03), spherical aberration (p = 0.001) and coma RMS (p = 0.04).
Conclusions
TOK induced more HORMS, spherical aberration and coma RMS than STM in myopic astigmats; however, both lens types showed an increase in HOA compared to baseline, which placed patients outside the age and pupil size matched normative ranges. While the optical changes that accompany these modalities are helpful for myopia management, the induction of HOAs may have unintended consequences on visual performance.
Keywords: astigmatism, toric orthokeratology, multifocal contact lenses, higher order aberrations, spherical aberration, coma
INTRODUCTION
The prevalence of myopia continues to rise, with the expectation of over five billion myopes by the year 2050.1 Higher levels of myopia can cause an increased risk for ocular diseases such as cataracts, glaucoma, retinal detachment and myopic maculopathy.2 While the need for myopia management is evident, the concomitant presence of astigmatism is often ignored. A large study showed the prevalence of astigmatism of at least 1.00 D in American children was 28.4%, with greater percentages observed in Asian and Hispanic children (33.6% and 36.9%, respectively).3 Astigmatism is also more prevalent in myopes compared to hyperopes.4 Few studies have examined the use of current myopia management contact lenses in the moderate to high astigmatic population.
Previous studies showed an increase in spherical aberration and coma with spherical orthokeratology lenses (Table 1). There is limited data on how higher order aberrations are affected by soft multifocal contact lenses (Table 2). These previous studies validate the ability to measure the wavefront error in eyes that have been reshaped by orthokeratology lenses or in eyes that are wearing aspheric multifocal contact lenses, whose power profiles are continuous or smooth over the entire optical surface.5,6 With spherical orthokeratology, the amount of aberration has been shown to be generally stable after one week of wear.7
Table 1.
Spherical aberration (SA), coma root mean square (RMS), and higher order root mean square (HORMS) increase during spherical orthokeratology lens wear.
| Author | Instrument | Contact Lens | Baseline Spherical Equivalent (D) | Wear Time | Pupil Diameter (mm) | SA (μm) | Coma RMS (μm) | Total HORMS (μm) |
|---|---|---|---|---|---|---|---|---|
| Sun8 | OPD-III Scan | Autek | −3.97 ± 1.53 | 1 month | 3 | ↑ to 0.06 | ↑ to 0.10 | ↑ to 0.21 |
| Yin9 | iTrace | Alpha-Ortho K | −3.40 ± 1.58† | 1 month | 4 | ↑ to 0.18 | ↑ to 0.35 | ↑ to 0.50 |
| Hiraoka10 | KR-9000 PW | Alpha-Ortho K | −1.78 ± 0.61 | 1 year | 4 | ↑ to 0.16 | ↑ to 0.25 | ↑ to 0.30 |
| Gifford11 | Discovery | BE lens | −2.36 ± 1.22 | 7 days | 5 | ↑ to 0.19 | ↑ to 0.28 | ↑ to 0.34 |
| Lian12 | WASCA | E&E Optics | −2.75 ± 0.92 | 7 days | 6 | ↑ to 0.46 | ↑ to 0.32 | ↑ to 0.67 |
| Lau13 | COAS | multiple | various | 1 year | 6, dilated | ↑ to 0.85 | ↑ to 0.41 | ↑ to 1.05 |
| Stillitano7 | LADARWave | BE lens | −2.10 ± 0.80† | 9 days | 6.5, dilated | ↑ to 0.85 | ↑ to 0.53 | ↑ to 1.04 |
represents only baseline sphere power (D),
OPD-III Scan (Nidek, nidek-intl.com), iTrace (Tracey Technologies, traceytechnologies.com), KR-9000 PW (Topcon, topconpositioning.com), Discovery (Innovative Visual Systems, ivisualsystems.com), WASCA = Wavefront Supported Custom Ablation (Carl Zeiss Meditec, zeiss.com), COAS = Complete Opthalmic Analysis System (Wavefront Sciences, wavefrontsciences.com), LADARWave (Alcon, alcon.com), Autek (Autek China., orthok.cn), Alpha-Ortho K (Alpha, alphacl.co.jp), BE lens (BE Enterprises, Australia, dissolved), E&E Optics (E&E Optics, eandeoptics.com)
Table 2.
Spherical aberration, coma root mean square (RMS), and higher order root mean square (HORMS) increase with soft multifocal lens wear.
| Author | Instrument | Lens | Baseline Spherical Equivalent (D) | Wear Time | Pupil Diameter (mm) | SA (μm) | Coma RMS (μm) | Total HORMS (μm) |
|---|---|---|---|---|---|---|---|---|
| Fedtke14 | BHVI-EyeMapper | Proclear MF center distance | Group 1: −2.90 ± 0.95, Group 2: −2.95 ± 0.78 | 8 days | 3 | ↑ to 0.03 | C8: ↑ to 0.05 | N/A |
| Martins15 | IRX3 | Precilens center-distance prototype | −2.23 ± 1.50 | 45 min | 5 | ↑ to 0.34 | ↑ to 0.63 | ↑ to 0.77 |
| Lopes-Ferreira†16 | IRX3 | Biofinity MF center distance | −0.66 ± 1.97 | 15 days | Max round pupil | ↑ by 0.07 | ↑ by 0.02 | ↑ by 0.07 |
MF = multifocal,
Higher order aberrations (HOA) for Lopes-Ferreira show an increase by the listed amount, whereas all others show an increase in HOA to that amount.
BHVI-EyeMapper (BHVI = Brien Holden Vision Institute, bhvi.org), IRX3 (ImaginEyes, imagine-eyes.com), Proclear and Biofinity (CooperVision, coopervision.com), Precilens (Presilens, precilens.com)
The predominant changes in HOA after orthokeratology wear have been observed in spherical aberration, horizontal and vertical coma.17 Changes in spherical aberration may result from reshaping of the cornea due to the mid-peripheral steepening, while changes in coma occur with lens decentration.13 Similarly, distance centre multifocal contact lenses can cause shifts in spherical aberration due to their positive peripheral power profile and again changes to coma follow from lens decentration.14,18 These specific categories of HOA, spherical-like (primary and secondary spherical aberration), coma-like (horizontal and vertical coma) and total higher order aberrations have been shown to change after orthokeratology lens wear.10,13,19 Studies that have looked at other Zernike terms, such as trefoil, quadrafoil and secondary astigmatism, showed only small and insignificant changes after orthokeratology lens wear.7 Therefore, this study will specifically evaluate changes in spherical aberration, horizontal and vertical coma.
The mechanisms by which orthokeratology and soft multifocal contact lenses slow axial elongation have not been fully elucidated. The prevailing theory is that an increase in myopic defocus on the peripheral retina serves as a stop signal for eye growth.2,20,21 These optical interventions can change the image profile by reducing relative peripheral hyperopia. This theory of relative peripheral defocus has been supported by both animal22 and human23,24 research. A related but alternative hypothesis is that these contact lenses increase higher order aberrations, specifically spherical aberration, due to the annular mid-peripheral steepening of the cornea after orthokeratology wear.10,25 As shown in Table 1 and Table 2, spherical aberration, coma and HORMS are consistently elevated after lens wear. While the research is in agreement that these contact lenses increase higher order aberrations, the relationship between increased aberrations and axial elongation is less clear;26 however, some studies have found that increased spherical aberration is associated with improved myopia control efficacy.27,28
To date, no study has directly compared higher order aberrations induced by soft multifocal and orthokeratology lenses. The purpose of this study was to quantify changes in select higher order aberrations (HOA), specifically spherical aberration, horizontal and vertical coma, recorded on a cohort of myopic astigmatic eyes after being fitted with toric orthokeratology (TOK) and soft toric multifocal (STM) contact lenses in a randomised order.
METHODS
Subjects
This randomised crossover study was conducted at the University of Houston College of Optometry. All subjects were adults, aged 18 to 39 years, with myopia of −5.00 D to plano and moderate to high refractive astigmatism of −3.50 D to −1.50 D. Subjects had to be free of ocular disease, including accommodative or binocular vision issues, with no history of previous ocular surgeries or gas permeable contact lens wear within one month of enrolling. The study was conducted in accordance with the Declaration of Helsinki and was approved by the University of Houston Institutional Review Board. The study was registered on ClinicalTrials.gov (NCT03728218) and all subjects consented to participate before beginning any assessment.
Contact Lenses
At the initial visit, subjects’ manifest refraction and corneal tomography were measured with the Oculus Pentacam HR (Oculus, pentacam.com). The difference between the average elevation value in the vertical and horizontal meridians at an 8-mm chord was calculated from the tomography images. This elevation difference and manifest refraction data were used to order Dual Axis corneal refractive therapy (CRT) lenses (Paragon Vision Sciences, paragonvision.com) following the manufacturer’s guidelines. These lenses have toric alignment curves but a spherical base curve. More details on the lens selection process have been reported previously.29
The same data were used to empirically order Proclear Multifocal Toric lenses (CooperVision, coopervision.com) with the base curve selection and powers based on the manufacturer’s fitting guideline. The centre distance design was used with a +2.50 D add power based on previous myopia control trials.30
The order of contact lens wear was randomised and separated by a 14 ± 2 day washout period, during which time the subjects wore their habitual correction.31 Corneal tomography was performed after the washout period to ensure the subject had returned to baseline levels prior to dispensing the second set of lenses.
Wavefront error
The iTrace (Tracey Technologies, traceytechnologies.com) was used to measure wavefront aberrometry. For ocular aberrations, the iTrace was shown to have good repeatability, with mean standard deviations < 0.05 μm for all of the Zernike terms analysed here.32 Subjects were dilated with two drops of 1% tropicamide separated by five minutes. Three pupil-centred measurements were taken on each eye at baseline, after TOK lens wear and after STM lens wear (Table 3). All measurements taken after lens wear were performed in the afternoon to account for diurnal variation with orthokeratology lenses. The three measurements collected on each eye were averaged term by term. At the baseline visit, the measurement was taken without correction. After TOK wear, the measurement was taken without the lens on the eye; however, after STM wear, the measurement was taken with the lens on the eye. Wavefront aberrations were fitted over a 5 mm pupil through the 8th radial order of the normalised Zernike polynomials, and reported through the 6th radial order. Zernike coefficients for left eyes were flipped about the vertical axis to align with right eyes for analysis.33
Table 3.
Complete study visit schedule showing wavefront error (WFE) measured at baseline uncorrected and at outcome visits, either without lenses (post toric orthokeratology) or with soft toric multifocal lenses.
| Visit | Day | Details |
|---|---|---|
| 1 | −30 to −7 | Baseline, WFE measured uncorrected |
| 2 | 1 | Contact lens fittings, randomization, dispense lens 1 |
| 3 | 10 ± 2 | Outcome (including WFE) lens 1 |
| Washout period, subjects wore habitual correction | ||
| 4 | 24 ± 2 | Dispense lens 2 |
| 5 | 34 ± 2 | Outcome (including WFE) lens 2 |
To maintain equality between the two lens types, only subjects who achieved acceptable high contrast distance visual acuity of 0.30 logMAR or better in each eye were included in the analysis (Figure 1). High contrast visual acuity was measured at 100% contrast with the M&S Smart System (M&S Technologies, mstech-eyes.com). Visual acuity of 0.30 logMAR was chosen as it is a common cutoff criterion for studies of refractive error, specifically after orthokeratology34 and refractive surgery.35
Figure 1.
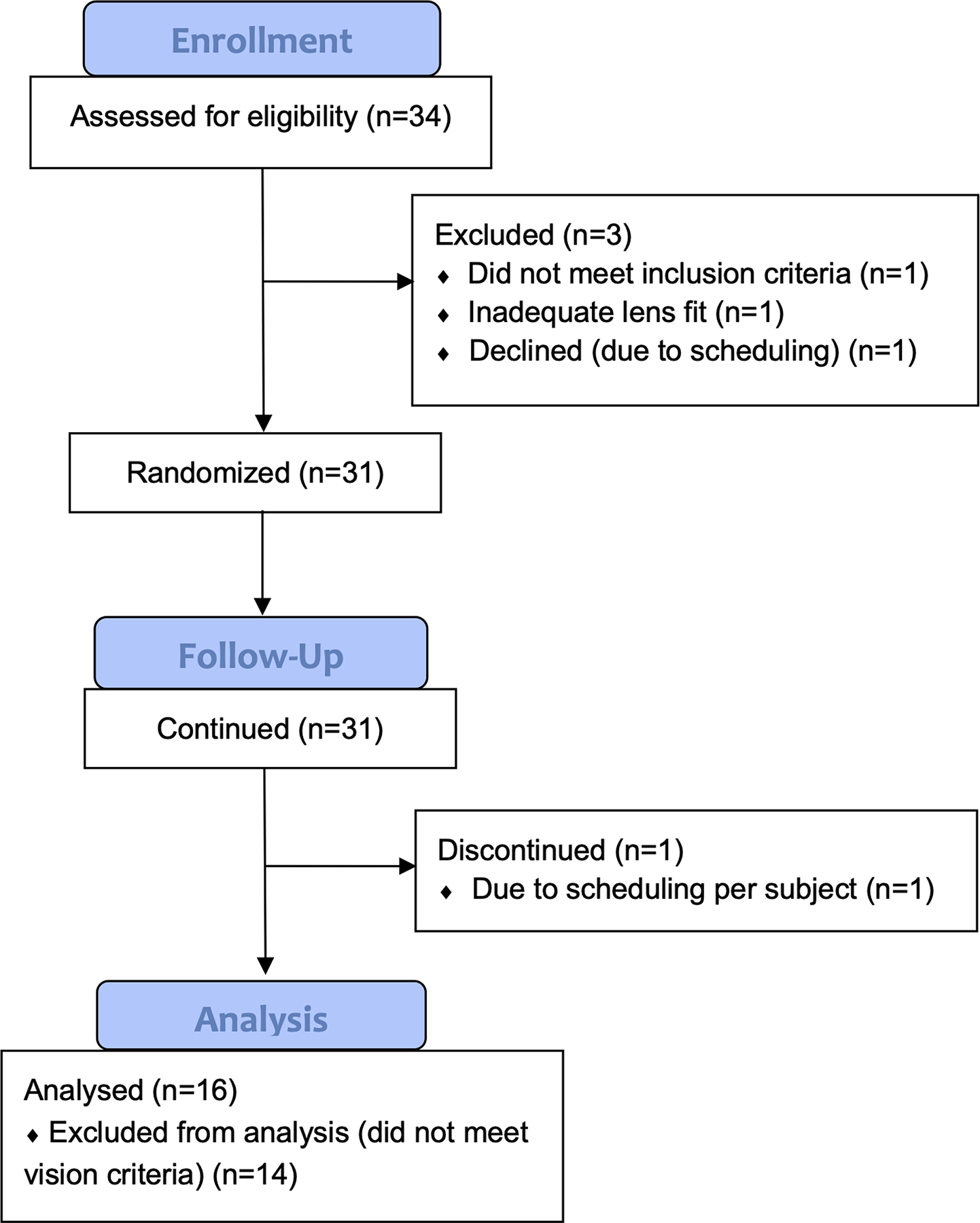
Participant flow diagram
Statistical analysis
Data were exported from the iTrace to Microsoft Office Excel (Microsoft, microsoft.com) and analysed with the commercial statistical software SPSS (version 25.0; IBM, ibm.com). Repeated measures analysis of variance (ANOVA) tests were performed. Both eye (right and left) and lens condition (baseline, TOK, and STM) were included in the model. Greenhouse-Geisser p-values were reported. Post-hoc paired t-tests were used, as appropriate, with Benjamini-Hochberg correction for multiple comparisons.
RESULTS
Both eyes of 16 subjects (32 eyes total) achieved high contrast logMAR visual acuity of 0.30 or better and were included in this analysis. The analysed group was older in age with less myopia than the group excluded from analysis; however, the amount of cylinder power and HORMS between the two groups is similar (Table 4). The analysed cohort included 12 females and 4 males, with an average age of 26.5 [5.1] years (ranging from 21 to 37 years). At baseline, the average manifest sphere power of both eyes was −2.06 [0.93] D with a refractive cylinder power of −1.99 [0.52] D.
Table 4.
Comparison (mean [SD]) of baseline characteristics between the analysed group and those excluded from analysis due to failing to meet the vision requirement. HORMS: Higher order root mean square.
| Analysed (n=16) | Excluded (n=14) | Significance | |
|---|---|---|---|
| Age (years) | 26.50 [5.06] | 22.79 [1.81] | p = 0.02* |
| Manifest sphere right eye (D) | −2.20 [0.90] | −3.34 [1.38] | p = 0.01* |
| Manifest sphere left eye (D) | −1.92 [0.96] | −3.43 [1.31] | p = 0.001* |
| Manifest cylinder right eye (D) | −1.91 [0.47] | −2.11 [0.50] | p = 0.27 |
| Manifest cylinder left eye (D) | −2.08 [0.57] | −1.98 [0.48] | p = 0.62 |
| HORMS right eye (μm) | 0.23 [0.06] | 0.27 [0.15]† | p = 0.37 |
| HORMS left eye (μm) | 0.25 [0.10] | 0.27 [0.14]† | p = 0.81 |
indicates statistical significance p < 0.05,
indicates mean and standard deviation of 13 available measures since one excluded subject’s data was not captured, all measures over 5 mm pupil size
Lower order aberrations consist primarily of defocus and astigmatism. The baseline lower order root mean square (LORMS) was higher in the excluded cohort (Table 5, both p < 0.04). After TOK wear, the residual LORMS was greater for the excluded groups than the analysed group (both p < 0.001). However, after STM wear, the LORMS for the analysed and excluded groups were not statistically different (both p > 0.20). In the analysed group, the residual LORMS with TOK and STM was not statistically different for either eye (both p > 0.09). However, in the excluded group, the residual LORMS was significantly greater after TOK than STM for both eyes (both p ≤ 0.002).
Table 5.
Comparison (mean [SD]) of lower order aberrations (LORMS) between the analysed group and those excluded from analysis due to failing to meet the vision requirement. TOK: Toric orthokeratology; STM: soft toric multifocal.
| Analysed (n=16) | Excluded (n=14)† | Significance | |
|---|---|---|---|
| Baseline LORMS OD (μm) | 3.36 [0.70] | 4.15 [1.24] | p = 0.04* |
| Baseline LORMS OS (μm) | 3.32 [0.66] | 4.29 [1.15] | p = 0.008* |
| TOK LORMS OD (μm) | 2.04 [0.57] | 3.35 [1.04] | p < 0.001* |
| TOK LORMS OS (μm) | 2.00 [0.67] | 3.53 [0.93] | p < 0.001* |
| STM LORMS OD (μm) | 1.69 [0.52] | 1.41 [0.74] | p = 0.24 |
| STM LORMS OS (μm) | 1.81 [0.61] | 1.99 [0.89] | p = 0.52 |
indicates statistical significance p < 0.05,
indicates mean and standard deviation of 13 available measures since one excluded subject’s data was not captured, all measures over 5 mm pupil size
At baseline, HORMS for the included eyes was 0.24 [0.08] μm (Figure 2). After TOK and STM wear, HORMS increased to 0.64 [0.22] μm and 0.48 [0.11] μm, respectively (both p < 0.001 compared to baseline). When compared to each other, TOK increased HORMS more than STM (p = 0.03) and resulted in a greater range of HORMS than STM, even though both are elevated from baseline conditions.
Figure 2.
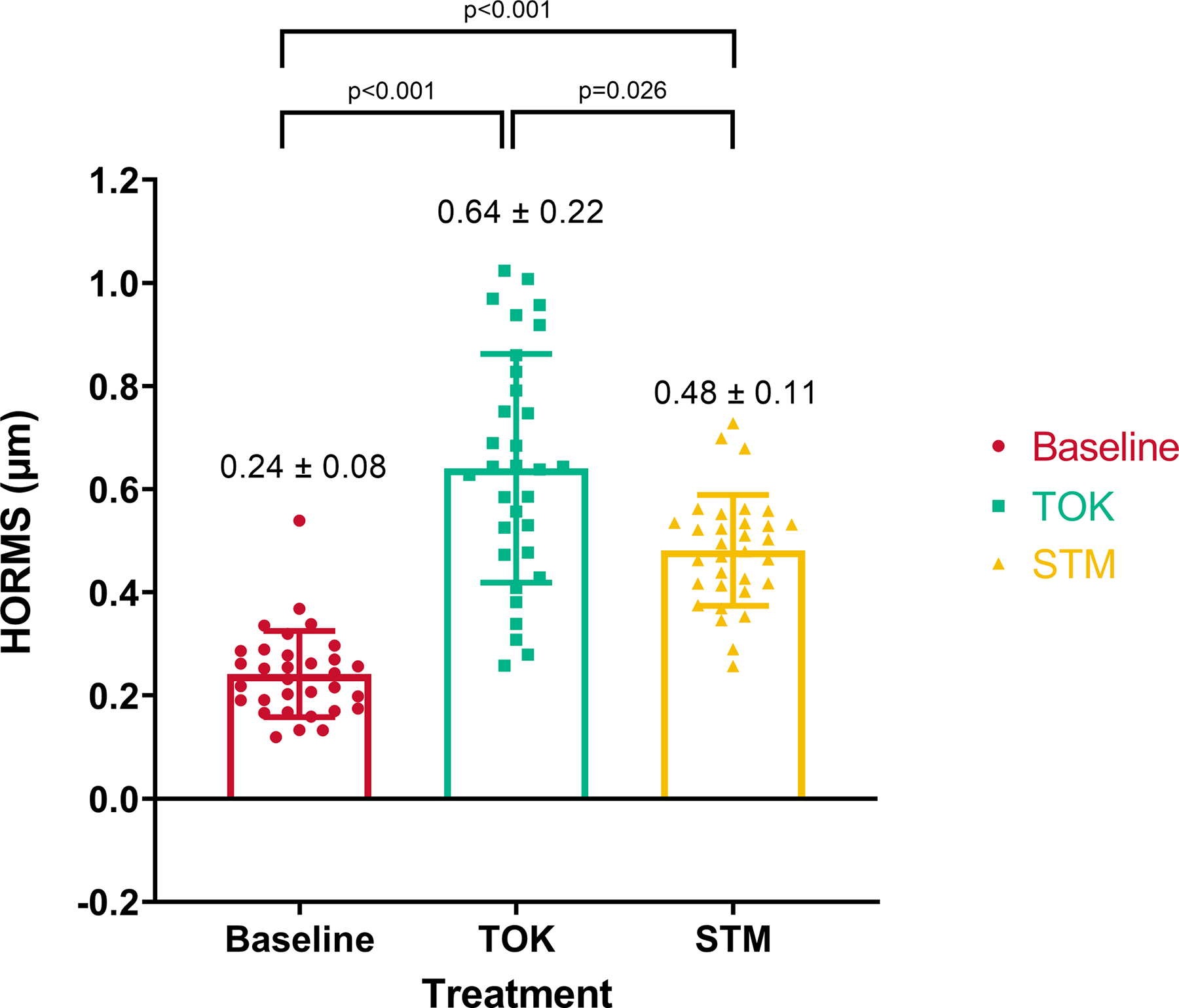
Higher order root mean square (HORMS) increased from baseline with toric orthokeratology (TOK) and soft toric multifocal (STM) lens treatments.
Primary spherical aberration has been shown to be elevated in previous studies evaluating eyes after orthokeratology and soft multifocal contact lens wear. In this study, C12 was 0.05 [0.07] μm at baseline (Figure 3). Primary spherical aberration increased after TOK (0.41 [0.16] μm) and STM (0.22 [0.14] μm) lens wear. These increases were significant when compared to baseline (both p < 0.001) and when compared to each other (p = 0.001). The intra-individual standard deviations for all three conditions were ≤ 0.03 μm.
Figure 3.
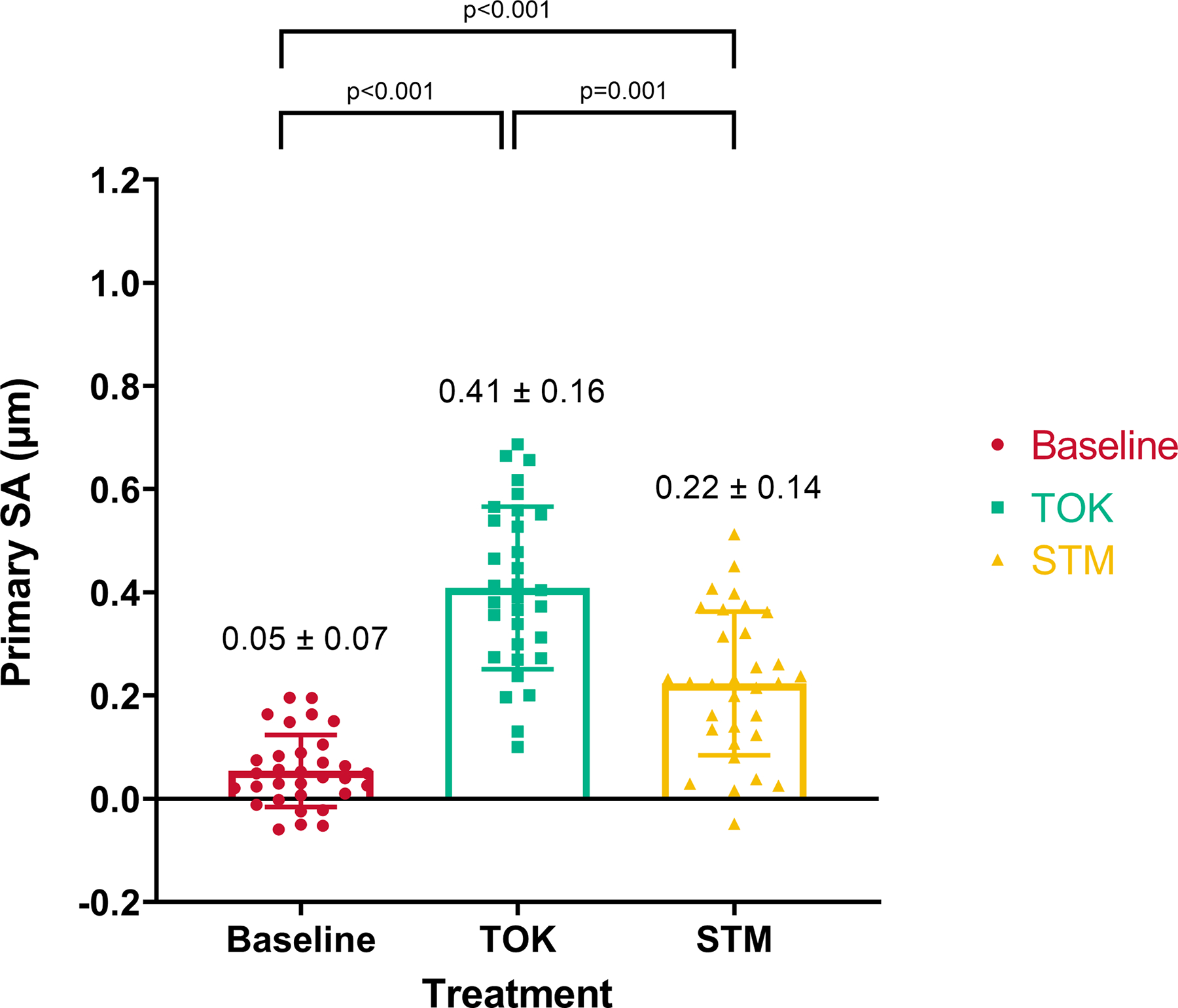
Primary spherical aberration increased from baseline with toric orthokeratology (TOK) and soft toric multifocal (STM) lens treatments.
Primary coma RMS includes both primary vertical (C7) and horizontal (C8) coma. As expected, primary coma RMS increased from baseline (0.15 [0.07] μm) to after TOK (0.43 [0.19] μm) and STM (0.32 [0.13] μm) lens wear (both p < 0.001) (Figure 4). Primary coma RMS was significantly greater after TOK wear compared to STM wear (p = 0.04). The intra-individual standard deviations for primary vertical and horizontal coma in all three conditions were ≤ 0.10 μm.
Figure 4.
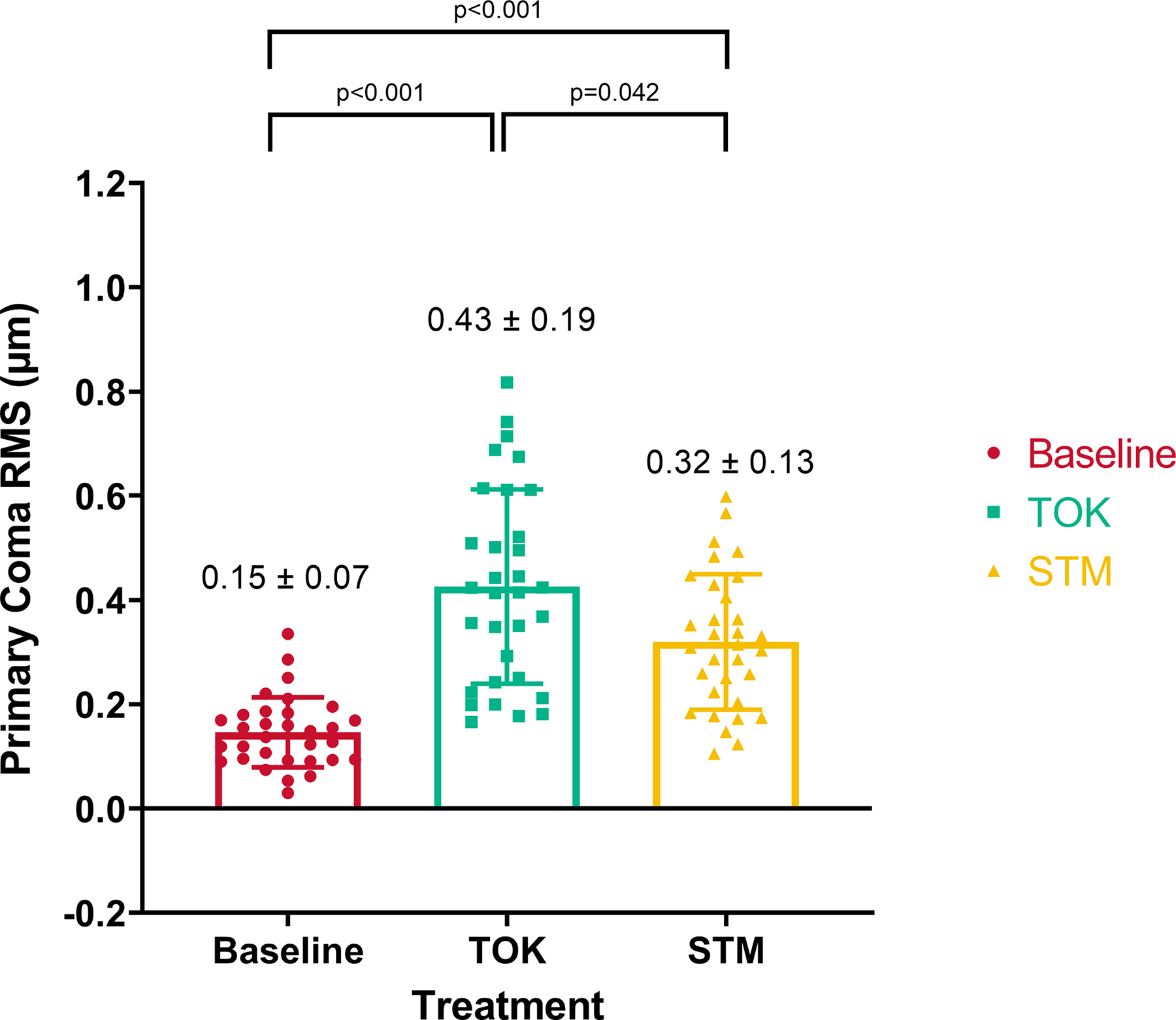
Primary coma root mean square (RMS) increased from baseline with toric orthokeratology (TOK) and soft toric multifocal (STM) lens treatments.
To put these values into context, the results of this study are summarised in Table 6, alongside previously published results from Applegate et al.36 showing the typical range of HOA for normal individuals of the same age and pupil size.
Table 6.
Comparison of study results to Applegate et al.36 showing the higher order aberrations (HOA) after the lens conditions were outside the typical range for normal individuals of the same age and pupil size (5 mm). HORMS: higher order root mean square.
| Baseline | TOK | STM | Applegate et al. | |
|---|---|---|---|---|
| HORMS (3rd – 6th order) (μm) | 0.242 ± 0.084 | 0.641 ± 0.222 | 0.481 ± 0.107 | 0.180 ± 0.059 |
| Coma RMS (C7 & C8) (μm) | 0.146 ± 0.067 | 0.426 ± 0.187 | 0.320 ± 0.130 | 0.087 ± 0.049 |
| Spherical Aberration (C12) (μm) | 0.053 ± 0.070 | 0.409 ± 0.157 | 0.223 ± 0.139 | 0.065 ± 0.057 |
DISCUSSION
The increase in HORMS, spherical aberration and coma associated with orthokeratology and soft multifocal contact lens wear align with previously published results (Tables 1 and 2). However, this study adds to the literature by directly comparing toric orthokeratology and soft toric multifocal lenses within the same sample, and found that the increase in higher order aberrations was consistently greater with the toric orthokeratology lenses for a common cohort of moderate to high myopic astigmatic eyes.
As mentioned previously, one of the theories regarding the mechanism of myopia control is increased spherical aberration, whereby more positive spherical aberration was reported to be associated with less axial elongation.27,28 Orthokeratology lenses reshape the cornea to become less prolate and thus induce greater positive spherical aberration.12 Centre distance multifocal contact lenses induce positive spherical aberration, whereas centre near multifocal contact lenses induce negative spherical aberration.37 If this theory is correct, our results show that in the same population wearing both orthokeratology and soft multifocal contact lenses, the orthokeratology lenses induced greater amounts of spherical aberration. This hypothesis, coupled with the observation that orthokeratology lenses induced higher levels of spherical aberration, could suggest that orthokeratology lenses may be better at slowing myopia progression. However, it is important to note that the predominant theory for myopia control is still the induction of peripheral myopic defocus. Further studies are needed to show whether increased spherical aberration is indeed correlated with slower axial elongation and less myopia progression.
Considering the impact on vision beyond the reduction in myopic defocus, the increase in higher order aberrations placed these subjects outside the normative range for individuals of the same age and pupil size (Table 6).36 This increase may translate to decreased visual performance or reduced subjective visual acceptance, which may be greater with orthokeratology lenses compared to soft multifocal lenses. The excluded group in this study were those who failed to meet the visual requirement of 0.30 logMAR or better with both lens modalities. Of the excluded participants, 10 did not meet the vision requirement with the orthokeratology lenses, one with the soft multifocal lens and two with both lens types. Therefore, a greater number of excluded participants had inadequate vision with orthokeratology lenses, despite reaching acceptable vision with soft multifocal lenses.
There were some limitations to this study due to the fact that the subjects were not refitted with either lens modality to achieve optimal fit for maximum potential treatment. Both the toric orthokeratology and soft toric multifocal lenses were ordered empirically and the subject only continued to randomisation if they could see 0.30 logMAR or better in each eye with each pair of lenses. For consistency in the fitting process, no lens adjustments were made.
To compare the outcomes of the two lens modalities fairly, data used in these analyses required that subjects could see 0.30 logMAR or better in each eye with each correction. Therefore, the sample size was limited. The inadequate vision of some subjects with the empirically ordered lenses demonstrated the typical clinical challenges of fitting myopic astigmatic patients.
The higher order aberration terms measured in this study had a large inter-individual deviation, especially with contact lens wear. When compared to normal individuals of the same age range and pupil size (Table 6),36 the standard deviation of the measurements was much greater with both lens conditions. This is likely related to the refractive error/power of the contact lenses and decentration which could cause more or less of the peripheral “add power” to be contained within the pupil (or analysis diameter for aberrometry).
Here, HORMS is used as a quantitative measure of the level of higher order aberration for three conditions (unaided, TOK-, and STM-corrected) on a common cohort of eyes. However, HORMS does not consider the origin of aberration from specific terms, and terms near the centre of the Zernike pyramid are known to impact vision more than those at the edge.38 Further, HORMS does not consider the manner in which aberration terms interact to form the resulting retinal image. For these reasons, HORMS has been shown to be a poor predictor of visual performance.36,39 Future research should focus on quantifying performance with a metric that considers these aspects of retinal and visual image quality, as well as taking multifocality into consideration, since current metrics have not been optimised or validated for optical or visual conditions intended to induce multifocality. At the time of writing, there is not a single accepted visual quality metric for multifocal or toric orthokeratology correction. Development of a new, or application of an existing, metric to conditions resulting in multifocality could help scientists and clinicians understand the unintended consequences of fitting these two lens modalities.
CONCLUSION
Both toric orthokeratology and soft toric multifocal lenses increased higher order aberrations, specifically HORMS, spherical aberration and coma RMS. Toric orthokeratology consistently increased these higher order aberrations by a greater amount than soft toric multifocal lenses. Both of these contact lens treatments place patients outside the age and pupil size-matched normative range. These changes in higher order aberrations may be helpful for myopia management but may have unintended consequences on visual performance.
Acknowledgement:
This work was supported by the National Institutes of Health Loan Repayment Program (Tomiyama) and NIH P30 EY007551 (Frishman). Paragon Vision Sciences provided the orthokeratology lenses but had no role in the study design or outcomes. Portions of this work were presented as a poster at the American Academy of Optometry meeting on 9 October 2020 in Nashville, Tennessee, USA.
Disclosures:
Dr. Richdale has received research funding from Alcon, Novartis, Paragon Vision Sciences, and Euclid Systems and consults for Novartis, Paragon Vision Sciences, SightGlass, and CooperVision. The remaining authors report no conflicts of interest and have no proprietary interest in any of the materials mentioned in this article.
References
- 1.: Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016; 123: 1036–1042. [DOI] [PubMed] [Google Scholar]
- 2.: Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res 2012; 31(6): 622–660. [DOI] [PubMed] [Google Scholar]
- 3.: Kleinstein RN, Jones L, Hullet S, et al. Refractive error and ethnicity in children. Arch Ophthalmol 2003; 121(8): 1141. [DOI] [PubMed] [Google Scholar]
- 4.: Young G, Sulley A & Hunt C. Prevalence of astigmatism in relation to soft contact lens fitting. Eye Contact Lens Sci Clin Pract 2011; 37(1): 20–25. [DOI] [PubMed] [Google Scholar]
- 5.: Wagner S, Conrad F, Bakaraju RC, Fedtke C, Ehrmann K & Holden BA. Power profiles of single vision and multifocal soft contact lenses. Contact Lens Anterior Eye. 2015; 38(1): 2–14. [DOI] [PubMed] [Google Scholar]
- 6.: Singh NK, Jaskulski M, Ramasubramanian V, et al. Validation of a clinical aberrometer using pyramidal wavefront sensing. Optom Vis Sci. 2019; 96(10): 733–744. [DOI] [PubMed] [Google Scholar]
- 7.: Stillitano I, Schor P, Lipener C & Hofling-Lima AL. Long-term follow-up of orthokeratology corneal reshaping using wavefront aberrometry and contrast sensitivity. Eye Contact Lens Sci Clin Pract 2008; 34(3): 140–145. [DOI] [PubMed] [Google Scholar]
- 8.: Sun Y, Wang L, Gao J, Yang M & Zhao Q. Influence of overnight orthokeratology on corneal surface shape and optical quality. J Ophthalmol 2017; 2017: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.: Yin Y, Zhao Y, Wu X, et al. One-year effect of wearing orthokeratology lenses on the visual quality of juvenile myopia: a retrospective study. PeerJ 2019; 7: e6998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.: Hiraoka T, Kakita T, Okamoto F & Oshika T. Influence of ocular wavefront aberrations on axial length elongation in myopic children treated with overnight orthokeratology. Ophthalmology 2015; 122(1): 93–100. [DOI] [PubMed] [Google Scholar]
- 11.: Gifford P, Li M, Lu H, Miu J, Panjaya M & Swarbrick HA. Corneal versus ocular aberrations after overnight orthokeratology. Optom Vis Sci 2013; 90(5): 439–447. [DOI] [PubMed] [Google Scholar]
- 12.: Lian Y, Shen M, Huang S, et al. Corneal reshaping and wavefront aberrations during overnight orthokeratology. Eye Contact Lens Sci Clin Pract 2014; 40(3): 161–168. [DOI] [PubMed] [Google Scholar]
- 13.: Lau JK, Vincent SJ, Cheung S-W & Cho P. Higher-order aberrations and axial elongation in myopic children treated with orthokeratology. Investig Opthalmology Vis Sci 2020; 61(2): 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.: Fedtke C, Ehrmann K, Thomas V & Bakaraju RC. Peripheral refraction and aberration profiles with multifocal lenses. Optom Vis Sci 2017; 94(9): 876–885. [DOI] [PubMed] [Google Scholar]
- 15.: Martins C, Amorim-De-Sousa A, Faria-Ribeiro M, Pauné J, González-Méijome JM, & Queirós A. Visual performance and high-order aberrations with different contact lens prototypes with potential for myopia control. Curr Eye Res 2020; 45(1): 24–30. [DOI] [PubMed] [Google Scholar]
- 16.: Lopes-Ferreira D, Fernandes P, Queirós A & González-Meijome JM. Combined effect of ocular and multifocal contact lens induced aberrations on visual performance. Eye Contact Lens Sci Clin Pract 2018; 44(5): S131–137. [DOI] [PubMed] [Google Scholar]
- 17.: Hughes RPJ, Vincent SJ, Read SA & Collins MJ. Higher order aberrations, refractive error development and myopia control: a review. Clin Exp Optom 2020; 103(1): 68–85. [DOI] [PubMed] [Google Scholar]
- 18.: Bakaraju RC, Ehrmann K, Ho A & Papas E. Inherent ocular spherical aberration and multifocal contact lens optical performance. Optom Vis Sci 2010; 87(12): 1009–1022. [DOI] [PubMed] [Google Scholar]
- 19.: Chang C-F & Cheng H-C. Effect of orthokeratology lens on contrast sensitivity function and high-order aberrations in children and adults. Eye Contact Lens Sci Clin Pract 2020; 46(6): 375–380. [DOI] [PubMed] [Google Scholar]
- 20.: Mutti DO, Hayes JR, Mitchell GL, et al. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Investig Opthalmology Vis Sci 2007; 48(6): 2510–2519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.: Holden B, Sankaridurg P, Smith E, Aller T, Jong M & He M. Myopia, an underrated global challenge to vision: where the current data takes us on myopia control. Eye. 2014; 28(2): 142–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.: Smith III EL & Hung L-F. The role of optical defocus in regulating refractive development in infant monkeys. Vision Res 1999; 39(8): 1415–1435. [DOI] [PubMed] [Google Scholar]
- 23.: Atchison DA, Jones CE, Schmid KL, et al. Eye shape in emmetropia and myopia. Investig Ophthalmol Vis Sci 2004; 45(10): 3380–3386. [DOI] [PubMed] [Google Scholar]
- 24.: Seidemann A, Schaeffel F, Guirao A, Lopez-Gil N & Artal P. Peripheral refractive errors in myopic, emmetropic, and hyperopic young subjects. J Opt Soc Am A 2002; 19(12): 2363–2373. [DOI] [PubMed] [Google Scholar]
- 25.: Berntsen DA, Barr JT & Mitchell GL. The effect of overnight contact lens corneal reshaping on higher-order aberrations and best-corrected visual acuity. Optom Vis Sci 2005; 82(6): 490–497. [DOI] [PubMed] [Google Scholar]
- 26.: Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutiérrez-Ortega R & Suzaki A. Short- and long-term changes in corneal aberrations and axial length induced by orthokeratology in children are not correlated. Eye Contact Lens Sci Clin Pract 2017; 43(6): 358–363. [DOI] [PubMed] [Google Scholar]
- 27.: Lau JK, Vincent SJ, Collins MJ, Cheung SW & Cho P. Ocular higher-order aberrations and axial eye growth in young Hong Kong children. Sci Rep 2018; 8(1): 2–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.: Hiraoka T, Kotsuka J, Kakita T, Okamoto F & Oshika T. Relationship between higher-order wavefront aberrations and natural progression of myopia in schoolchildren. Sci Rep. 2017; 7(1): 7876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.: Tomiyama ES, Logan A-K & Richdale K. Corneal elevation, power, and astigmatism to assess toric orthokeratology lenses in moderate-to-high astigmats. Eye Contact Lens Sci Clin Pract 2021; 47(2): 86–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.: Walline JJ, Walker MK, Mutti DO, et al. Effect of high add power, medium add power, or single-vision contact lenses on myopia progression in children. JAMA. 2020; 324(6): 571–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.: Kang P & Swarbrick H. The influence of different ok lens designs on peripheral refraction. Optom Vis Sci 2016; 93(9): 1112–1119. [DOI] [PubMed] [Google Scholar]
- 32.: Visser N, Berendschot TTJM, Verbakel F, Tan AN, de Brabander J & Nuijts RMMA. Evaluation of the comparability and repeatability of four wavefront aberrometers. Investig Ophthalmol Vis Sci 2011; 52(3): 1302–1311. [DOI] [PubMed] [Google Scholar]
- 33.: Smolek MK, Klyce SD & Sarver EJ. Inattention to nonsuperimposable midline symmetry causes wavefront analysis error. Arch Ophthalmol 2002; 120(4): 439–447. [DOI] [PubMed] [Google Scholar]
- 34.: Koffler B, Sears J, Wohl L & Forstot L. Success rate of incorporating corneal refractive therapy into 3 different ophthalmology practices. Eye Contact Lens. 2016; 42(1): 74–79. [DOI] [PubMed] [Google Scholar]
- 35.: Chalita MR, Xu M, Krueger RR. Retreatments after laser in situ keratomileusis. J Refract Surg. 2005: 624–630. [PubMed] [Google Scholar]
- 36.: Applegate RA, Donnelly III WJ, Marsack JD, Koenig DE & Pesudovs K. Three-dimensional relationship between high-order root-mean-square wavefront error, pupil diameter, and aging. J Opt Soc Am A 2007; 24(3): 578–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.: Richdale K, Cox I, Kollbaum P, et al. CLEAR – Contact lens optics. Contact Lens Anterior Eye 2021; 44(2): 220–239. [DOI] [PubMed] [Google Scholar]
- 38.: Applegate RA, Sarver EJ & Khemsara V. Are all aberrations equal? J Refract Surg 2002; 18(5): S556–562. [DOI] [PubMed] [Google Scholar]
- 39.: Applegate RA, Marsack JD, Ramos R & Sarver EJ. Interaction between aberrations to improve or reduce visual performance. J Cataract Refract Surg. 2003; 29(8): 1487–1495. [DOI] [PubMed] [Google Scholar]


