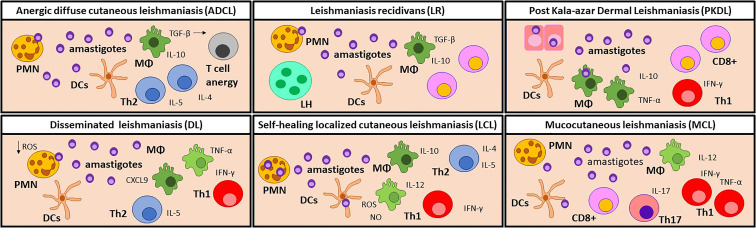
Figure 2.
Immune cell profiles in the skin lesion of CL and PKDL patients. Anergic diffuse cutaneous leishmaniasis (ADCL) lesions are developed due to a lack of a Th1 response. Parasites can interact directly with macrophages which, even when abundant, are polarized towards an M2 profile and produce high levels of TGF-β. Consequently, T cells are activated towards IL-4, IL-5, and IL-10-producer Th2 cells. In this environment, T cells become anergic, leading to chronic disease. It is noteworthy that this manifestation is particularly common in immunosuppressed patients. Disseminated leishmaniasis (DL) patients show a temporary impairment of the early T cell response, which allows for dissemination of the parasite. Later, CXCL9 attracts T-cells to the lesion site, causing a lack of systemic Th1 response. In the lesion, IL-10, iNOS, TNF-α, and IFN-γ are found in similar levels as LCL lesions. In self-healing localized cutaneous leishmaniasis (LCL), phagocytes are the first responders against infection by producing ROS and NO to destroy the parasites, but can also become permissive hosts for amastigotes. A Th1 response, characterized by IL-12 and IFN-γ, is necessary for the control of the disease while the Th2 immune response promotes tissue repair, leading to the self-healing of the lesion. In rare occasions, LCL can relapse as Leishmaniasis recidivans (LR), but the trigger stimulus is still unknown. LR is characterized by TGF-β and IL-10 production, as well as an increased ratio of CD8+ vs. CD4+ T cells. LR lesions also show a granulomatous infiltrate containing lymphohistiocytic and multinucleated giant cells. Post Kala-azar Dermal Leishmaniasis (PKDL) develops when the cellular response is reactivated after drug treatment. The remaining parasites in the skin elicit an increased inflammatory response and the development of dermal lesions. An increased proportion of CD8+ T cells over CD4+T cells is often observed, but the role of CD8 T cells is still unclear. Mucocutaneous Leishmaniasis (MCL) lesions are characterized by a chronic and hyperactive inflammatory immune response. IFN-γ and TNF-α producing Th1 cells and cytotoxic CD8+ cells are predominant leading to tissue destruction. The high numbers of Th17 and polymorphonuclear neutrophils (PMN) contribute to exacerbated inflammation, while the low levels of IL-10 detected are related to the poor control of inflammation. Manifestations with a mixed immune profile lead to a moderate pathology, while a hyperpolarized response results in a severe disease. MΦ, Macrophages; DCs, dendritic cells; PMN, Neutrophils; Th, T helper cells; LH, lymphohistiocytic and multinucleated giant cells; PKDL, Post Kala-azar Dermal Leishmaniasis.