Abstract
Femoro-acetabular impingement (FAI), is the result of an abnormal morphology of the hip joint. On the femoral side, asphericity of the head can be highlighted by an alpha angle measurement >50° on computed tomography or MRI. However, some particular cephalic asphericities can make it difficult to measure the alpha angle, leading to a diagnostic pitfall. While in the classic cam effect, the deformity is peripheral and can be treated by arthroscopic femoroplasty, an apical head deformity remains a therapeutic challenge. We present the case of a 17-year-old male patient with a femoral head deformity, corresponding to an ISHA zone 6 overhang, significantly improved in everyday and sports life by arthroscopic trapdoor technique to resect the focal central deformity while enabling concomitant treatment of central compartment pathology, in this case, a hypertrophic ligamentum teres and femoral head chondral flap. Etiology of this femoral head deformity remains uncertain but could be a particular cam deformity, sequelae to pediatric disease or instability with repeated traction of the ligament teres on the femoral head apical insertion during cephalic growth.
INTRODUCTION
Femoro-acetabular impingement (FAI), first described by Ganz in 2003 [1] is the result of an abnormal morphology of the hip joint, femoral head–neck junction deformity creating the cam effect, acetabular retroversion or overhang creating the pincer effect and both deformities creating the mixed effect. Historically, the gold standard for FAI treatment was the open approach, but the evolution and progress of arthroscopic techniques make it possible to manage almost all FAI pathology.
On the femoral side, the head sphericity can be measured by the alpha angle, described by Notzli [2]. Normal alpha angle on X-rays does not exclude asphericity of the femoral head and should be measured on a multiplanar modality on Computed tomography or MRI [3]. Several authors have suggested that an alpha angle >50° is considered pathological on computed tomography or MRI [3, 4]. However, some particular cephalic asphericities can make it difficult to correctly position the circle and therefore to measure the alpha angle, which can lead to a diagnostic pitfall. A precise analysis of the sphericity of the femoral head on the multiplanar modality can sometimes reveal unusual deformations. While in the classic cam effect, the deformity is peripheral and can be treated by arthroscopic femoroplasty, a central or apical deformity remains a therapeutic challenge.
We report the case of a 17-year-old male patient with a femoral head deformity, corresponding to an ISHA zone 6 overhang treated under arthroscopy. Current review of the orthopedic literature on PubMed, Google Scholar and so on produced no prior publications on the topic of arthroscopic decompression of central or apical femoral head deformities.
CASE DESCRIPTION
History
A 17-year-old male patient was referred by his pediatric doctor for left hip pain. He had a normal morphology with a weight of 63 kg for 180 cm tall (BMI = 19.4), and no significant medical history. He practices running and bodybuilding regularly. The patient has complained of left inguinal pain for 6 months, initially triggered by hyperflexion. Since then he has experienced persistent inguinal pain in flexion, internal rotation and lameness after 20 min of walking, with difficulties in sports activities. The patient did not complain of mechanical symptoms or instability events, such as clicking snapping or giving way. He cannot return to sport. Physiotherapy and medical treatment (NSAID) did not resolve the symptoms.
Clinical evaluation
Clinical examination revealed a leg length discrepancy of +10 mm on the left side. Range of motion was symmetrical to contralateral range of Motion (extension 10°, flexion 110°, abduction 45°, adduction 10°, supine rotations at 90° flexion were 45° external and 20° internal). Flexion Adduction and Internal Rotation (FADIR) test and Extension Abduction and External Rotation test were positive.
Pre-operative imaging
Pelvic X-rays demonstrated left Coxa plana with the impression of a very high alpha angle at 105° in axial Dunn view. Coxometry revealed a lateral center-edge angle of Wiberg of 30°, Tonnis angle of 0° and anterior center-edge angle of 35°. MRI showed an asymmetric femoral head with a flat superior part and bony edema near the fovea. No labral tear was identified. Arthro-computed tomography (arthro-CT) confirmed the femoral head deformity (Fig. 1), and proper evaluation showed an excess of bone in the apical part of the head with an anterosuperior subchondral bone depression filled by thicker cartilage, explaining the illusion of a superior flat on the X-rays (Fig. 2). Postero-superior acetabular chondral lesions were also present on the arthro-CT.
Fig. 1.
(a and b) Arthro-computed tomography showing an aspherical femoral head, a thicker cartilage on the anterosuperior subchondral depression and chondral lesions on the posterior head (A—axial view/B—coronal view).
Fig. 2.
(a) Arthro-CT imaged of the apical deformity. A—axial view with a circle showing the normal head sphericity in red, and the apical excess of bone outside the circle and B—CT scan tangent to the apical deformity at the level of the yellow line, showing the diameter of the excess bone in green. ( b) Arthro-CT imaged of the apical deformity A—axial view with a circle showing the normal head sphericity in red, and the apical excess of bone outside the circle and B—CT scan tangent to the apical deformity at the level of the yellow line, showing the diameter of the excess bone in green.
Intra-operative findings and surgical technique
Arthroscopic treatment was finally decided and planned on the Arthro-CT. The excessive bone on the femoral apex could be circumscribed like an 8-mm circle (Fig. 2), thus only removing this bony area could restore the femoral head sphericity. Arthroscopic exploration showed mild joint effusion, an irreducible osteochondral flap in the apex of the femoral head, corresponding to the deformity of the head, and a hypertrophic ligamentum teres (Fig. 3). Chondral palpation did not detect any gap or depression in the anterosuperior cartilage. There was no labral lesion. Arthroscopic testing showed no cam effect, no abnormal congruency in extension but revealed a femoro-acetabular decoaptation starting at 45° flexion (Fig. 4). Resection of the apical bony deformity by drilling through the great trochanter and femoral neck started with the introduction of a 2-mm guide pin under fluoroscopic assistance. Arthroscopy could control the good position of the guide pin through the center of the deformity. Once perfectly centered stepwise cannulated reaming beginning with a 6-mm and ending with an 8-mm drill, was performed, carefully terminating just under the chondral flap (Fig. 5). The bone at the lesion was very sclerotic. Then, part of the ligamentum teres was debrided to decrease its volume. After decompression, we noted the reducibility of the chondral flap by direct pressure (Fig. 6) and the restoration of a better congruence in hip flexion (Fig. 7) without further decoaptation during testing. We relied on the head-acetabular congruence to fit the cartilaginous flap without needing to fixate it. Because the lesion was not placed in a weight-bearing area, we decided not to add auto or allograft under the chondral flap to avoid loss of reduction, or bony extravasation inside the joint. Post-operative X-rays are shown Fig. 8.
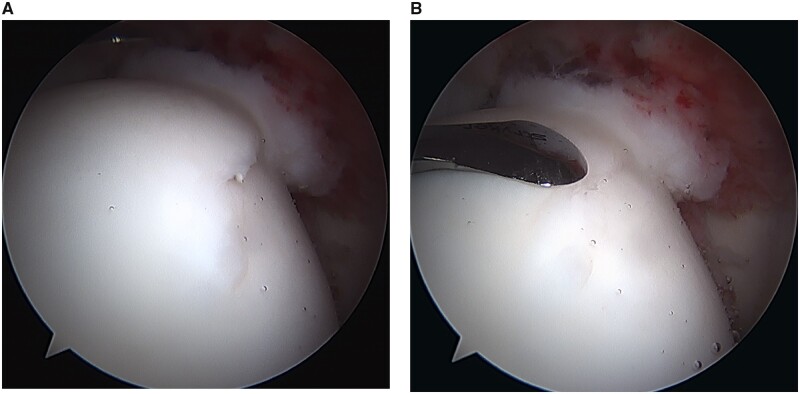
Fig. 3.
(a) Arthroscopic superior view of the central compartment under traction with 70° scope in the anterolateral portal, Shaver in the mid anterior portal. A—irreducible chondral flap in the apex of the femoral head and B—apical deformity of the femoral head with a large ligamentum teres. ( b) Arthroscopic superior view of the central compartment under traction with 70° scope in the anterolateral portal, Shaver in the mid anterior portal. A—irreducible chondral flap in the apex of the femoral head and B—apical deformity of the femoral head with a large ligamentum teres.
Fig. 4.
(a) Arthroscopic anterior view of the peripheral compartment, traction released, with 70° scope in the mid anterior portal. A—no abnormal congruency in extension and B—decoaptation in early flexion. ( b) Arthroscopic anterior view of the peripheral compartment, traction released, with 70° scope in the mid anterior portal. A—no abnormal congruency in extension and B—decoaptation in early flexion.
Fig. 5.
(a) Cannulated reaming of the lesion on a guide pin under arthroscopic and radioscopic assistance (A—arthroscopic superior view of the guide pin in the center of the lesion − 70° scope in the anterolateral portal/B—Fluoroscopic A-P view). ( b) Cannulated reaming of the lesion on a guide pin under arthroscopic and radioscopic assistance (A—arthroscopic superior view of the guide pin in the center of the lesion − 70° scope in the anterolateral portal/B—fluoroscopic A-P view).
Fig. 6.
(a) Arthroscopic superior view of the central compartment under traction with 70° scope in the anterolateral portal, palpation tool in the mid anterior portal (A—unreduced chondral flap/B—reduced chondral flap by direct pressure after drilling). ( b) Arthroscopic superior view of the central compartment under traction with 70° scope in the anterolateral portal, palpation tool in the mid anterior portal (A—unreduced chondral flap/B—reduced chondral flap by direct pressure after drilling).
Fig. 7.

Arthroscopic anterior view of the peripheral compartment, traction released, with 70° scope in the mid anterior portal showing a better congruence restoration in hip flexion.
Fig. 8.
Postoperative X-rays.
Post-operative rehabilitation
Post-operative care consisted of immediate full weight bearing, 4 weeks of hip rotation and abduction restriction and re-education protocol in physiotherapist care unit with passive flexion mobilization. Rotations, abduction and muscular reinforcement began at 1 month. At 3 months, the patient had no pain with daily activities and recovered full range of motion. FADIR position was still sensitive. He was allowed to return to sport.
CLINICAL RESULTS
At 4 years follow-up, the patient is satisfied with the procedure. He describes a few episodes of transient pain and giving way to his hip after intensive sports sessions, but no symptoms in usual activities. Modified Harris hip score (mHHS) increased from 66 pre-operatively to 77 at 4 years of follow-up. This is a significant improvement because the Minimal Clinically Important Difference (MCID) values have been reported to be approximately eight points for the mHHS in hip arthroscopy [5]. Womac score and non-arthritic hip score (NAHS) are 11 and 88.25, respectively. These two scores were not collected preoperatively and therefore cannot be compared to preoperative status. The patient in this report did not have signs of arthritis at the time of surgery and has not developed joint space narrowing in the 4-year period following surgery. Four years post-operative X-rays are shown in Fig. 9.
Fig. 9.
(a) Four years follow-up X-rays, A-P pelvis X-ray. (b and c) Dunn view (b) and Lequesne False profile view (c).
DISCUSSION
Femoral head–neck junction deformity producing flexion-induced mechanical cam impingement is a well-known subtype of femoro-acetabular impingement. This deformity results in a peripheral asphericity of the femoral neck and is commonly treated by resection osteoplasty under arthroscopy. However, in some cases, the asphericity concerns the central part of the femoral head [6]. Treatment is then challenging, based on the good evaluation and comprehension of the deformity thanks to multi-planar and 3D reconstruction imaging. From this analysis, we must define the precise extent and location of the deformity to recreate the most spherical head possible. Very few surgical techniques are described in the literature. Ganz published a femoral head reduction osteotomy for coxa magna by open resection of the central third of the head and fixation of the lateral third to the medial third [6, 7]. In this particular case, the apical deformity was creating the illusion of a coxa magna that could have been eligible for this surgical technique. Another considered option was a large peripheral osteoplastic resection under arthroscopy, but planning showed that sufficient osteoplasty to restore sphericity would violate a large part of the weight-bearing cartilaginous zone.
Once understood that the deformity was purely apical, and that taking of this 8 mm central bony outgrowth was the solution, we considered arthroscopic debridement but straight instruments like burrs and shavers are unable to access the femoral head apex via standard portals because of bony constraints even on the distracted hip. Theoretic extreme distraction might enable this access, but at high risk of iatrogenic injury to nerves, muscles and capsule. Surgical dislocation [8] to directly access the apex of the femoral head and thus, the deformity was another option. Nevertheless, in these two situations, the cartilage at the deformity would have been sacrificed unless a larger cartilage flap was created to expose the bony deformity. This could have resulted in an unstable apical flap requiring fixation. If the suture is the strongest chondral repair technique [9] knots or wire on the femoral side may abrade and damage the adjacent acetabular cartilage. Other techniques have been described for the repair of osteochondral defects in femoral head such as mosaicplasty [10, 11], allografts [10, 12] or retrograde drilling under the subchondral bone, grafting associated with microfracture under arthroscopic assistance [13].
After consideration of the aforementioned options, we decided to proceed with a described surgery called the trapdoor technique [14, 15] which has previously been described primarily as a treatment of femoral head osteonecrosis. Peripheral drilling and/or reaming enables ‘outside-in’ treatment of more central femoral head pathology similar to core decompression and without the need for excessive hip distraction. If the procedure could have been performed under fluoroscopic control alone, the addition of arthroscopy facilitates and direct control when drilling, ensuring precise deformity correction without iatrogenic damage to the overlying cartilage. Arthroscopic visualization confirmed successful chondral flap reduction after drilling and improved hip mobility after correction, so femoral head decoaptation in flexion was certainly induced by the deformity. Arthroscopy was also helpful to search and treat associated lesions: the ligamentum teres were hypertrophic and could be debrided. Reconstruction of the ligament could have been an option, the femoral tunnel having already been performed, but since the patient did not complain of instability, we preferred to keep this procedure in the event of specific symptoms [16]. We relied on the head-acetabular congruence to stabilize the chondral flap without needing to fix it. The reduction of the chondral flap was maintained by the congruence of the hip. A suture of the chondral flap would have been possible in a retrograde manner, but faced with the complexity of the procedure, the risk of damaging the cartilage of the femoral head or even the adjacent acetabular cartilage, we preferred to rely on head-acetabular congruence to maintain the flap in the reduced position, despite the risk of instability with persistent pain and/or snapping. As drilling was not likely to compromise bone integrity and fracture resistance, even as much as the standard peripheral cam decompression, early weight bearing was decided to promote compression of the chondral flap with congruent surfaces to aid in its reduction.
The disadvantage of the arthroscopic procedure on open surgical dislocation was the inability to have perfect control over the restoration of the sphericity of the femoral head. Therefore, careful preoperative planning was mandatory to achieve the best result. We had plain radiographs, MRI and arthro-CT scan to plan this surgery. 3D CT scan or even better, 3D printing, would have been of great help to evaluate the deformity and plan the perfect resection [17]. However, these techniques do not assess the articular cartilage of the femoral head, which presented different thicknesses in this patient, so the isolated correction of the bone could have been inadequate.
The etiology of the femoral head asphericity in this case is uncertain. The patient was not an athlete, but although it is known that the prevalence of cam-type deformities is more common in athletes, they can occur in the general population [18, 19]. There was no family history, genetics having also been described as a possible factor of cam-type deformity [20]. Finally, there was no history of hip diseases such as epiphysiolysis or Perthes. Moreover, this deformity did not have the appearance of typical cam deformity or a sequelae to pediatric disease. Instability could be one possible explanation with repeated traction of the ligament teres on the femoral head apical insertion which would have created this deformity during cephalic growth since, during arthroscopy, a bulky ligament requiring debridement was present. However, this hypertrophic ligament could also be the result of repeated trauma caused by the impingement between the deformity and the acetabulum.
Considering the pathomechanism, it may be different from classic cam FAI. The apical deformity could cause a sensitive incongruity during hip flexion, as we observed the head levers out of the acetabulum causing loss of labral fluid seal at mid-flexion. Symptoms could also be induced by the apical irreducible chondral flap impinging with the acetabular fossa and maybe by a participation of the hypertrophic ligamentum teres.
CONCLUSION
Apical femoral head deformities may be an atypical form of cam femoracetabular impingement with asphericity. Arthroscopic treatment is feasible using a trapdoor technique to resect the focal central deformity while enabling concomitant treatment of central compartment pathology, in this case, a hypertrophic ligamentum teres and femoral head chondral flap.
CONFLICT OF INTEREST STATEMENT
Dr N. Bonin has no conflicts of interest related to this study to declare; outside of the study, however, he is a consultant for Stryker and receives royalties as a designer for ConMed and Dedienne Santé. Dr B. Moratel declare that they have no competing interest.
FUNDING
This paper was published as part of a supplement financially supported by the European Society for Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA) www.esska.org.
REFERENCES
- 1. Ganz R, Parvizi J, Beck M. et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003; 417: 112–20. [DOI] [PubMed] [Google Scholar]
- 2. Notzli HP, Wyss TF, Stoecklin CH. et al. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 2002; 84-B: 556–60. [DOI] [PubMed] [Google Scholar]
- 3. Dudda M, Albers C, Mamisch T. et al. Do normal radiographs exclude asphericity of the femoral head-neck junction? Clin Orthop Relat Res 2009; 467: 651–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tannast M, Siebenrock KA, Anderson S.. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. Am J Roentgenol 2007; 188: 1540–52. [DOI] [PubMed] [Google Scholar]
- 5. Nwachukwu BU, Chang B, Rotter B. et al. Minimal clinically important difference and substantial clinical benefit after revision hip arthroscopy. Arthroscopy 2018; 34: 1862–8. [DOI] [PubMed] [Google Scholar]
- 6. Ganz R, Horowitz K, Leunig M.. Algorithm for combined femoral and periacetabular osteotomies in complex hip deformities. Clin Orthop Relat Res 2010; 468: 3168–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ganz R, Huff TW, Leunig M.. Extended retinacular soft tissue flap for intraarticular hip surgery: surgical technique, indications, and results of its application. Instr Course Lect 2009; 58: 241–55. [PubMed] [Google Scholar]
- 8. Ganz R, Gill T, Gautier E. et al. Surgical dislocation of the adult hip: a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br 2001; 83: 1119–24. [DOI] [PubMed] [Google Scholar]
- 9. Cassar-Gheiti AJ, Byrne DP, Kavanagh E. et al. Comparison of four chondral repair techniques in the hip joint: a biomechanical study using a physiological human cadaveric model. Osteoarthr Cartil 2015; 23: 1018–25. [DOI] [PubMed] [Google Scholar]
- 10. Du D, Hsu P, Zhu Z. et al. Current surgical options and innovation for repairing articular cartilage defects in femoral head. J Orthop Transl 2020; 21: 122–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Viamont-Guerra M-R, Bonin N, May O. et al. Promising outcomes of hip mosaicplasty by minimally invasive anterior approach using osteochondral autografts from the ipsilateral femoral head. Knee Surg Sports Traumatol Arthrosc 2020; 28: 767–76. [DOI] [PubMed] [Google Scholar]
- 12. Chen JW, Rosinsky PJ, Shapira J. et al. Osteochondral allograft implantation using the Smith-Peterson (anterior) approach for chondral lesions of the femoral head. Arthrosc Tech 2020; 9:e239–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ziino C, Safran RM.. Evolution of a posttraumatic femoral head bone cyst: a case study and surgical management. Orthop J Sports Med 2019; 7: 2325967119859287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mont MA, Einhorn TA, Sponseller PD, Hungerford DS.. The trapdoor procedure using autogenous cortical and cancellous bone grafts for osteonecrosis of the femoral head. J Bone Joint Surg Br 1998; 80: 56–62. [DOI] [PubMed] [Google Scholar]
- 15. Xu H, Niu X, Li Y. et al. What are the results using the modified trapdoor procedure to treat chondroblastoma of the femoral head? Clin Orthop Relat Res 2014; 472: 3462–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. O'Donnell J, Klaber I, Takla A.. Ligamentum teres reconstruction: indications, technique and minimum 1-year results in nine patients. J Hip Preserv Surg 2020; 7: 140–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bockhorn L, Gardner SS, Dong D. et al. Application of three-dimensional printing for pre-operative planning in hip preservation surgery. J Hip Preserv Surg 2019; 6: 164–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Agricola R, Bessems JHJM, Ginai AZ. et al. The development of Cam-type deformity in adolescent and young male soccer players. Am J Sports Med 2012; 40: 1099–106. [DOI] [PubMed] [Google Scholar]
- 19. Siebenrock KA, Ferner F, Noble PC. et al. The cam-type deformity of the proximal femur arises in childhood in response to vigorous sporting activity. Clin Orthop Relat Res 2011; 469: 3229–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pollard TC, Villar RN, Norton MR. et al. Genetic influences in the aetiology of femoroacetabular impingement: a sibling study. J Bone Joint Surg Br 2010; 92-B: 209–16. [DOI] [PubMed] [Google Scholar]