Abstract
Psichiatric illness such as depression, schizophrenia and cognitive deficiency are frequently associated with the Darier Disease. Physicians should be aware of such association to allow prompt diagnosis and early interventions of potentially life‐threatening psychiatric disorders.
Keywords: ATP2A2, Darier disease, neuropsychiatric disease
Psichiatric illness such as depression, schizophrenia and cognitive deficiency are frequently associated with the Darier Disease. Physicians should be aware of such association to allow prompt diagnosis and early interventions of potentially life‐threatening psychiatric disorders.
![]()
1. INTRODUCTION
Darier disease (DD) is a rare genodermatosis caused by heterozygous mutations in the ATP2A2 gene highly expressed both in the skin and in the brain. This finding suggests its role in the pathogenesis of cutaneous and neurocognitive manifestations with neuropsychiatric symptoms.
Darier disease is an autosomal dominant skin disorder caused by loss of adhesion between epidermal cells (acantholysis). Hyperkeratotic papules, predominantly distributed in seborrheic areas, distinctive nail abnormalities, and palmar and plantar pits are the typical clinical manifestations. Onset of the disease usually occurs around puberty, and the course of the disorder is characterized by remissions and relapses. 1 It is caused by mutations in a single gene, ATP2A2, which encodes the sarco⁄endoplasmic reticulum Ca2+. ATPase isoform 2 (SERCA2), a calcium pump located in the endoplasmic reticulum (ER) membrane. A range of neuropsychiatric features have been reported in DD patients including major depression, bipolar disorder, learning disabilities, and mental retardation. 1 , 2 We report a case of DD in a 15‐year‐old patient who presented a range of major neuropsychiatric symptoms.
2. CASE REPORT
A 15‐year‐old Caucasian girl came to our observation for a 4‐year history of itchy papular eruption mainly localized on the trunk and folds. The lesions were often accompanied by a very unpleasant smell. Such manifestations typically worsened in the summer period after sun exposure, with spontaneous remission in the cold seasons. Her father had a similar rash. There was no history of atopic dermatitis or allergic manifestations. At time of our observation, multiple reddish‐brown greasy papules mainly localized on décolleté, abdomen, and dorsum were detected (Figure 1A,B). The mucosa was not affected. Nails abnormalities and punctate depressions (pitting) on the palms and soles were observed. Biopsy of a papular lesion on the left supraclavicular region was performed. Histopathologic examination revealed intra‐epidermal acantholysis associated with dyskeratosis, confirming the clinical diagnosis of DD (Figure 1C). In course of examination, the patient showed a humble look, with apathetic behavior and no apparent interest about her medical condition. Because of the possible association between DD and psychiatric illness, the patient underwent neuropsychological evaluation that revealed impairment of psychosocial functioning with social withdrawal. Suicidal ideation, abulia, anguish, and guilty feeling were also noted. The cognitive profile was examined through the administration of a second level test, the WISC‐IV (Wechsler Intelligence Scale for Children) in order to identify the patient's strengths and weaknesses. The performance was lower than the expected standard for age and grade of school education with an Intelligence Quotient (IQ) of 62. Clinical interview evidenced an emotional experience influenced by a state of marked emotional distress. Criticism, self‐disqualification, and tendency to excessive rumination emerged from which suicidal ideation arose. The diagnosis of mixed behavior and emotional disorder in a patient with mild cognitive disability was made, according to the Diagnostic and Statistical Manual of Mental Disorders (DSM‐5). Skin lesions were started on topical methylprednisolone twice daily for 10 days, followed by daily application of pimecrolimus ointment for 1 month, with progressive reduction of scales and itching. The patient was treated with alprazolam and carbolithium. Weekly psychological support sessions and biweekly specific cognitive training were scheduled; the help of a school support was strongly recommended. At follow‐up visit, after 2 months of therapy, no improvement of skin lesions was observed. Psychiatric examination also revealed a bad therapeutic outcome with low adherence to the cognitive supports and worsening of agoraphobia and suicidal ideation. So, aripiprazole was added to therapy, with improved control of the disease at 6 months' follow‐up. No skin changes were recorded, due to spontaneous discontinuation of topical therapies.
FIGURE 1.
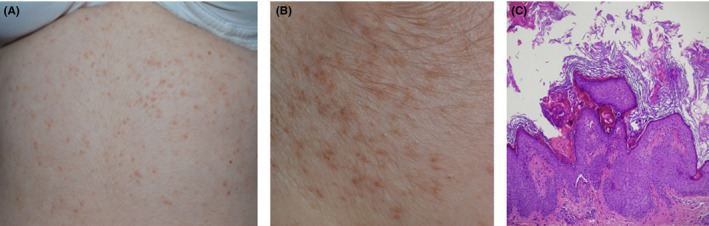
A, B, Multiple reddish‐brown greasy papules localized on abdomen and on the neck; C, A biopsy specimen revealed intra‐epidermal acantholysis associated with dyskeratosis (hematoxylin‐eosin, original magnification x20)
3. DISCUSSION
We report a paradigmatic case of DD linked to neuropsychiatric symptoms. DD is a rare autosomal dominant genetic skin disorder classified as hereditary acantholytic dermatosis. Age of onset is generally 11‐20 years, and the course of the disorder is typically relapsing. Penetrance is complete although expressivity is highly variable. 1 DD is caused by mutations in a single gene, ATP2A2, which encodes the sarco⁄endoplasmic reticulum Ca2+ ATPase isoform 2 (SERCA2), a calcium pump located in the endoplasmic reticulum (ER) membrane that plays a pivotal role in intracellular calcium signaling. Since ATP2A2 gene is highly expressed both in the skin and in the brain, its' possible pleiotropic effects could be explained by the ectodermal origin of these tissues and by the involvement of intracellular calcium signaling in neuronal excitability, neurotransmission, and synaptic plasticity. 1 , 2 The finding that the ATP2A2 gene is expressed in the human brain strongly suggests its role in the pathogenesis of neurocognitive manifestations of DD. 2 Clinically, it is characterized by yellow to brown hyperkeratotic papules, predominantly distributed in seborrheic areas. Less common cutaneous findings include distinctive nail abnormalities and palmar and plantar pits. The occurrence of neuropsychiatric features in DD has been reported, including major depression (which is the most commonly observed), bipolar disorder, learning disabilities, and mental retardation. 2 The prevalence of depression in DD patients is considerably higher than the general population lifetime prevalence as reported in the European Study of the Epidemiology of Mental Disorders (30% and 12%‐8%, respectively). 3 Our patient showed several psychiatric phenotypes, including both major depression and deficit in cognitive functions. In addition, Cederlof et al 4 showed that patients with DD had a 4.3 times higher risk of being diagnosed with bipolar disorder and a 2.3 times higher risk of being diagnosed with schizophrenia, compared to nonaffected ones. About intellectual functioning, our patient had a IQ lower than average and low school performance. A Swedish nationwide study found a sixfold increased risk of being diagnosed with intellectual disability. 5 These findings could in part negatively influence the therapeutic adherence rate in some patients affected by DD. In fact, such in our case, patients may not be able to fully understand their condition and to properly carry out the medical prescription. At present, dermatologic treatment is difficult. In the majority of cases, therapeutical approach has the aim to improve pruritus and irritation. General measures include topical emollients in association with soap substitutes and cotton clothing. Furthermore, in case of history of photo‐aggravation, sun protection is also essential. The concomitant application of topical retinoids could be useful, and in some cases, oral retinoids, either acitretin or isotretinoin, could be prescribed. The use of topical corticosteroids could reduce inflammation but do not alter the disease course. 6 The apathetic behavior and the low interest about medical condition, in association with the dysthymia, could represent a factor of poor adherence to both dermatologic and psychiatric therapy. There is no clear relationship between DD severity and incidence of psychiatric manifestations, with a relatively high prevalence of psychiatric problems even in patients with mild skin symptoms. 7
4. CONCLUSION
Our case deals with the role of skin as visual marker of potential life‐threatening neuropsychiatric alterations, underlining the need for a careful, prolonged follow‐up in order to prevent undesirable consequences‐such as suicide attempt‐and to improve the adherence to therapy. For this purpose, patients' family also needs to be adequately informed and involved in the therapeutic path. Moreover, according to the autosomal dominant inheritance of DD, a familial counseling, is strongly recommended in order to promptly diagnose a potential dermatologic and neuropsychiatric involvement of the family members.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
FLP: first author, wrote the manuscript. AM: collected the data of the patient. LB: was responsible for the clinical message. LM: involved in patient's treatment and follow‐up modalities. NCA: performed neuropsychiatric analysis. RC: reviewed pathologic report. MV: was responsible for review and revision. FB: served as a principal investigator, established the diagnosis, and was responsible for discussion and revision.
ETHICAL APPROVAL
We confirm that the manuscript has been read and approved by all named authors.
CONSENT STATEMENT
Published with written consent of the patient.
Li Pomi F, Motolese A, Bertino L, et al. Beyond the skin involvement in Darier disease: A complicated neuropsychiatric phenotype. Clin Case Rep. 2021;9:e04263. 10.1002/ccr3.4263
DATA AVAILABILITY STATEMENT
All data relevant to the study are included in the article.
REFERENCES
- 1. Foggia L, Hovnanian A. Calcium pump disorders of the skin. Am J Med Genet C Semin Med Genet. 2004;131C:20‐31. [DOI] [PubMed] [Google Scholar]
- 2. Dodiuk‐Gad R, Lerner M, Breznitz Z, et al. Learning disabilities in Darier's disease patients. J Eur Acad Dermatol Venereol. 2014;28(3):314‐319. [DOI] [PubMed] [Google Scholar]
- 3. Gordon‐Smith K, Jones LA, Burge SM, Munro CS, Tavadia S, Craddock N. The neuropsychiatric phenotype in Darier disease. Br J Dermatol. 2010;163(3):515‐522. [DOI] [PubMed] [Google Scholar]
- 4. Cederlof M, Bergen SE, Langstrom N, et al. The association between Darier disease, bipolar disorder, and schizophrenia revisited: a population‐based family study. Bipolar Disord. 2015;17(3):340‐344. [DOI] [PubMed] [Google Scholar]
- 5. Cederlof M, Karlsson R, Larsson H, et al. Intellectual disability and cognitive ability in Darier disease: Swedish nation‐wide study. Br J Dermatol. 2015;173(1):155‐158. [DOI] [PubMed] [Google Scholar]
- 6. Haber RN, Dib NG. Management of Darier disease: a review of the literature and update. Indian J Dermatol Venereol Leprol. 2021;87(1):14‐21. [DOI] [PubMed] [Google Scholar]
- 7. Dodiuk‐Gad RP, Cohen‐Barak E, Khayat M, et al. Darier disease in Israel: combined evaluation of genetic and neuropsychiatric aspects. Br J Dermatol. 2016;174(3):562‐568. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article.


