Fig. 3. Prevalence of human cytomegalovirus antibodies and incidence of infection in immunocompromised individuals.
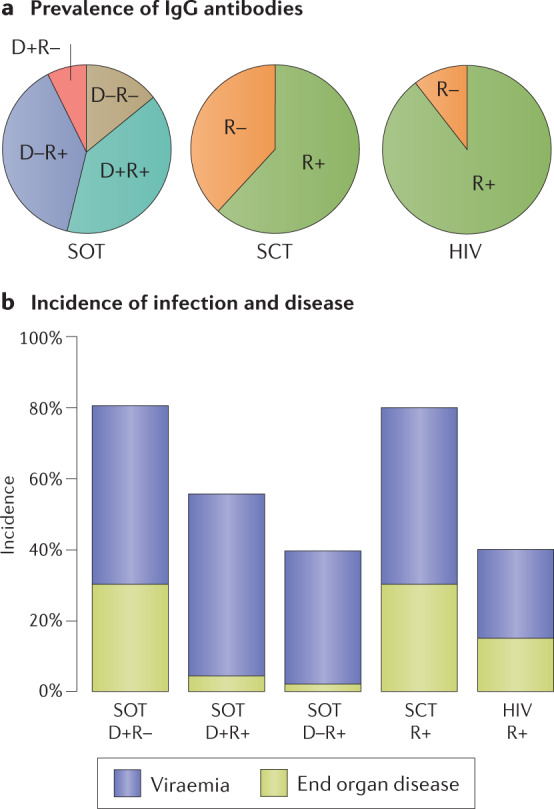
a | Prevalence of prior human cytomegalovirus (HCMV) infection is high (~90%) in individuals with HIV infection and intermediate (~60%) in those awaiting haematopoietic stem cell transplantation (SCT). The solid organ transplantation (SOT) patient group can be divided further according to prevalence of antibodies in the donor as well as the recipient. b | Once individuals become immunocompromised either through immunosuppression after transplantation or because the CD4+ T cell count in individuals who are HIV-positive falls below 100 cells per microlitre of blood, they are at risk of HCMV viraemia, which can be detected by PCR. In the SOT group, the risk is highest in those with primary infection (donor positive–recipient negative (D+R–)), intermediate in those at risk of reactivation or reinfection (D+R+) and lowest in those at risk of reactivation only (D–R+). This illustrates that pre-existing natural immunity against HCMV provides substantial protection against exogenous (reinfection) and endogenous (reactivation) sources of virus. Note that the incidence of end organ disease (EOD) declines in parallel with reduced detection of viraemia. In the SCT group, the risk of viraemia and EOD is as high as in D+R– individuals in the SOT group, despite the SCT patients being R+. Comparison of the SCT group with D–R+ individuals in the SOT group shows that reactivation dominates R+ SCT recipients and that ablation of their bone marrow greatly reduces immunity acquired in the past. The incidence of both viraemia and EOD is intermediate in individuals who are HIV-positive. Figure drawn from information provided in refs9,13,50,70,120–122.
