Abstract
Cross-sectional analyses were conducted in the baseline cohort of the Adolescent Brain and Cognitive Development (ABCD) Study to determine if lifetime low-level alcohol use was associated with an increased likelihood of lifetime suicidality (N=10,773, ages 9-10). Among the lifetime suicide ideation and attempt groups, 37.7% and 36.2% reported lifetime low-level alcohol use, respectively; versus 22.2% in the non-suicidality group. Children reporting lifetime alcohol use (i.e., ≥ a sip) showed a nearly two-fold increase in their odds of lifetime suicidality compared to those with no previous alcohol use. Future prospective research with this cohort will continue to probe alcohol-suicidality associations.
Keywords: suicide prevention, substance use, children
1. Introduction
Alcohol use is linked to suicidality during adolescence and young adulthood1-4. However, children as young as 9-years-old report drinking behavior6,7 and suicidality8,9; therefore it is possible that an association between alcohol and suicidality can be detected much earlier in life than is currently known5,10,11. We aimed to cross-sectionally examine whether self-reported low-level alcohol use (lifetime alcohol drinks and/or sip, meaning any alcohol use by ages 9-10 years old, including sipping) is associated with an increased likelihood of lifetime suicidality (lifetime SI and SA) among children enrolled in the Adolescent Brain Cognitive Development (ABCD) study baseline cohort12-14.
2. Methods
2.1. Protocol
ABCD is an NIH-funded 10-year longitudinal study being conducted across 21 sites in the U.S. (n=11,875)15. These analyses focus on the cross-sectional association between self-reported lifetime low-level alcohol use and lifetime suicidality at baseline study. A detailed account of the study protocol and recruitment strategy is previously published12,16-20.
2.2. Measures
Participants and their parent/guardian were interviewed in separate rooms to maintain confidentiality. The analyses presented here drew from a subset of self- and parent-report questionnaires described below from the ABCD baseline data (Release 2.0.1).
Youth-report of lifetime (any previous) suicidal ideation (SI) or suicide attempt (SA) were obtained from a computerized version of the Kiddie-Schedule for Affective Disorders and Schizophrenia (K-SADS-PL DSM-521)22. The sample was separated into three groups; (1) SI, (2) SA and (3) non-suicidality (i.e., denied SI/SA). Participants who endorsed both SI and SA were classified as SA. Youth completed the iSay Sip Inventory23 to characterize participants’ lifetime low-level alcohol use (any previous alcohol use, including sips).
Demographic covariates included parent-reported demographic variables of participant sex, race/ethnicity, parental education and marital status from the PhenX toolkit24-30. Additional covariates included parent-reported Achenbach Child Behavior Checklist (CBCL31) T-scores to control for internalizing and externalizing problems; the Behavioral Inhibition System and Behavioral Approach System (BIS/BAS) subscale scores32 measuring avoidance and approach sensitivities reflective of motivational traits32-34; sleep problems and average sleep duration assessed using the parent-reported Sleep Disturbance Scale for Children (SDSC)35; and parents/guardians report of the presence/absence of family history of alcohol use disorders in first- and second-degree relatives of the participant on the Developmental History Questionnaire35-38.
2.3. Data Analysis
Differences in demographic and behavioral variables between the outcome variable groups for SI, SA and non-suicidality (i.e., NON) groups were determined using ANOVAs for continuous variables and χ2-tests for categorical variables. All covariates were included in primary, post-hoc, and secondary analyses.
A multilevel (2-level, participant within study site) multinomial logistic regression40 was completed to examine whether any lifetime alcohol use increased odds of classification into SI/SA versus NON, with NON used as the reference group. Post-hoc analyses explored whether alcohol use increased likelihood of SA versus SI classification. The multilevel multinomial logistic regression was re-run with the sex at birth by alcohol use interaction term to explore whether the relationship between lifetime low-level alcohol use and classification of suicidality differed by birth sex.
3. Results
3.1. Participant Characteristics
A total of 10,773 participants (52% male) had valid data on the predictor (lifetime low-level alcohol use) and outcome (group membership to lifetime SI, lifetime SA, or non-suicidality and were included in the analyses. Approximately 54.7% of the participants were White, 13.3% Black, 19.5% Hispanic/Latino, and 12.5% “Other/Mixed”. The average age was 9.9 years.
3.2. Prevalence of Alcohol Use and Suicidality
Nearly one-quarter of participants (23.5%) self-reported lifetime low-level alcohol use. A total of 7.6% reported lifetime history of SI, and 1.3% reported lifetime history of SA. Within the SI group and SA groups, 37.7% and 36.2% reported alcohol use, respectively, as did 22.2% in the NON group. Within the group who reported any alcohol use, 14.1% reported lifetime SI/SA, versus 7.2% among those with no history of alcohol use.
Differences were found across the three groups (SI/SA/NON) for sex (male %, SI 58%/ SA 57.2%/ NON 51.6%, p=<.001), race/ethnicity (white %, SI 55.3%/ SA 40.6%/ NON 55%, p=<.001), parent education (some college %, SI 32.3%/SA39.1% /NON 28.7%, p=<.001), parent marital status (married %, SI 66.5%/SA 50.7%/NON 70.1%, p=<.001), and for the covariates avoidance (mean and SD, SI 10.7 (3.9)/SA 11.0 (4.3)/NON 9.4 (3.7), p=<.001) and approach sensitivity ([reward responsiveness mean and SD, SI 11.4 (2.9)/SA 11.6 (3.1)/NON 11.0 (2.9), p=<.001], [drive mean and SD, SI 4.5 (3.2)/SA 5.7 (3.7)/NON 4.0 (3.0), p=<.001], [fun seeking mean and SD, SI 6.3 (2.8)/SA 7.3 (3.0)/ NON 5.6 (2.6), p=<.001]), internalizing (mean and SD, SI 52.3 (11.4)/SA 55.9 (12.6) /NON 48 (10.4), p=<.001) and externalizing behaviors (mean and SD, SI 49.7 (11.0)/ SA 53.6 (12.5)/NON 45.1 (10.0), p=<.001), average sleep duration (9-11 hours %, SI 46.6%/SA 31.2%/NON 48.7%, p=<.001), sleep problems (mean and SD, SI 38.6 (9.6)/ SA 40 (9.3)/NON 36.3 (7.9), p=<.001) and family history of alcohol use disorders (positive %, SI 18.6%/SA 17.4%/NON 14.7%, p=.002).
3.3. Multilevel, Multinomial Logistic Regression Models
Reporting lifetime alcohol use significantly increased children’s odds of being classified as SI (p=<.001, 95%CI 1.822, 2.399) and SA (p=.034, 95%CI 1.349, 3.763), versus NON (Figure 1). Post-hoc analyses revealed that lifetime alcohol use did not increase the odds of being classified as SA versus being SI (p=.767, 95%CI .667, 1.742) group.
FIGURE 1:
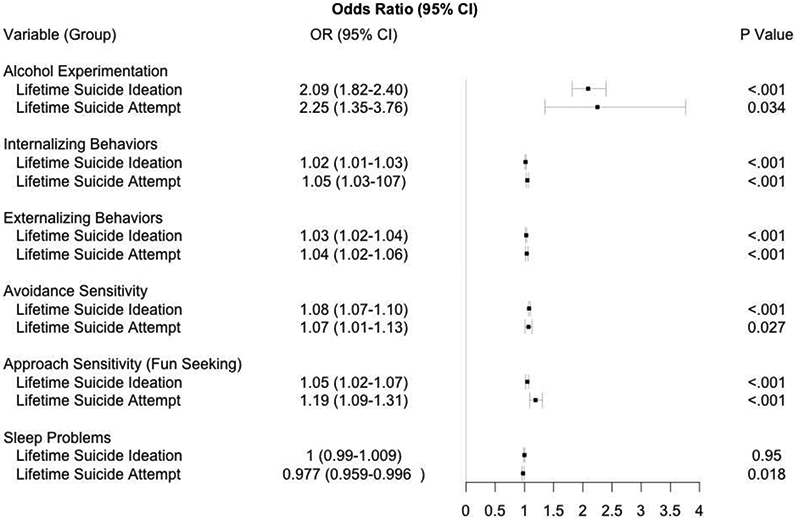
Forest Plot of Significant Predictors per Group
Several covariates were associated with increased odds of being classified as SI versus NON, including male sex (p=.002, 95%CI 1.095, 1.378), more internalizing behaviors [p=<.001, 95%CI 1.009, 1.027], and externalizing behaviors [p=<.001, 95%CI 1.019,1.035]), higher avoidance (p=<.001, 95%CI 1.066, 1.102), and approach sensitivity to fun seeking (p=<.001, 95%CI 1.021, 1.074). Similarly, covariates related to increased odds of classification as SA versus NON were more internalizing [p=<.001, 95%CI 1.032, 1.066] and externalizing [p=<.001, 95%CI 1.018, 1.057]) behaviors, more sleep problems (p=.018, 95%CI .959, .996) and higher avoidance sensitivity (p=.027, 95%CI 1.010, 1.134) and approach sensitivity to fun seeking (p=<.001, 95%CI 1.094, 1.312). The interaction of sex at birth and alcohol use did not increase odds of being classified as SI (p=.414, 95%CI .879, 1.391) or SA (p=.814, 95%CI .549, 2.163), versus NON.
4. Discussion
The relationship between alcohol use and suicidality in young adults is well established27,43-46. Here, we provide evidence that children as young as 9-10 years, a group underrepresented in the alcohol-suicide literature41,42, are experimenting with alcohol and experiencing suicidality, and that associations between alcohol use and suicidality can be detected in this age group42. Future prospective research in this diverse cohort is needed to better understand biological and behavioral mechanisms that may be underlying any alcohol-suicidality relationships observed as these youth get older and alcohol use increases. Emotional functioning47, avoidance and approach sensitivity (linked to negative affect and impulsivity48,49), and sleep problems39,50,51 were accounted for in our statistical modeling and did not eliminate the relationship between alcohol use and suicidality, yet they warrant further examination of the influence they have on suicidality and psychopathology during adolescence since they were associated with increased odds of suicidality in this large sample of children.
Rates of lifetime SI (7.6%) and SA (1.3%) have important clinical relevance in suicide prevention. First, our findings underscore a need for suicide risk screening with children as young as 9-10 years-old (e.g., school, primary care)51-54. To date, there are no validated suicide risk screening tools for youth as young as 9 years of age53-57,68. Additionally, nearly all the available interventions for suicidality are designed for adults60. Prevention and interventions need to be adapted to meet the unique needs of children58,59. Considering that children who have attempted suicide are up to 6 times more likely to attempt suicide again in adolescence61, this vulnerable population deserves greater attention from researchers, funding organizations and policymakers61,62.
4.1. Limitations
Given the cross-sectional nature of these analyses, causal inferences cannot be determined from these results. Nevertheless, establishing an association between alcohol use and suicidality in children is clinically valuable as it can aid in identifying at-risk youth. Children who present with suicidality could be screened for alcohol use and vice versa. Further, establishing this association paves the way for examining causal mechanisms in future research.
Also, self-report data have inherent limitations, particularly in research on sensitive topics such as illegal or stigmatized behaviors. The reporting of alcohol use and suicidality may be influenced by stigma, desirability bias, fear of intervention by child protection or social services63,64 and loss of autonomy65. Although this remains possible, ABCD was designed minimize these effects. Research assistants underwent extensive training to alleviate concerns about disclosure of responses to parent/guardian. Additionally, proportions of the sample reporting alcohol use and suicidality are higher than expected based on previous research7,66,67, thus, systematic underreporting is unlikely. In follow-up ABCD studies, we will implement validity checks on self-report items by examining consistency over time on responses to repeated measures of substance use and SI/SA.
4.2. Conclusions
This is the first large sample study to demonstrate that alcohol use (even low-level) is associated with increased odds of suicidality in children as young as 9-10 years. Increased efforts to prevent low-level alcohol use among children as young as 9-10 years old is warranted and may help reduce the rising rates of suicide.
Highlights.
Determine if low-level alcohol use increases the likelihood of suicidality in children.
Children who reported any lifetime alcohol use (i.e., a sip or more) showed a nearly two-fold increase in their odds of reporting lifetime suicidality compared to their counterparts who reported no previous alcohol use.
Longitudinal research will help establish the causal relationship and etiology of the alcohol-suicidality association.
Acknowledgements:
Work on this paper was supported by the National Institute on Drug Abuse grants U01 DA041089 (Jacobus and Aguinaldo), R01 DA044143 (Hasler), and R21 DA047953 (Jacobus); the National Institute on Alcohol Abuse and Alcoholism grants T32AA013525 (P.I.: Riley/Tapert to Aguinaldo) and R01 AA025626 (Hasler); the National Institute of Mental Health grant P50 MH115838 (Brent); and the California Tobacco-Related Disease Research Grants Program Office of the University of California grant 580264 (Jacobus). The content is solely the view of the authors and does not necessarily represent the official view of the NIH or NHMRC.
Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive Development (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9-10 and follow them over 10 years into early adulthood. The ABCD Study is supported by the National Institutes of Health and additional federal partners under award numbers U01DA041022, U01DA041028, U01DA041048, U01DA041089, U01DA041106, U01DA041117, U01DA041120, U01DA041134, U01DA041148, U01DA041156, U01DA041174, U24DA041123, and U24DA041147. A full list of supporters is available at https://abcdstudy.org/federal-partners.html. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/Consortium_Members.pdf. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in analysis or writing of this report. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or ABCD consortium investigators. The ABCD data repository grows and changes over time. The ABCD data used in this report came from Annual Release 2.0.1, doi: 10.15154/1504041. DOIs can be found at https://ndar.nih.gov/study.html?id=72
Footnotes
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Durant RH, Smith JA, Kreiter SR, Krowchuk DP. The Relationship Between Early Age of Onset of Initial Substance Use and Engaging in Multiple Health Risk Behaviors Among Young Adolescents. Archives of Pediatrics & Adolescent Medicine. 1999;153(3):286–291. [DOI] [PubMed] [Google Scholar]
- 2.Kim D-S, Kim H-S. Early initiation of alcohol drinking, cigarette smoking, and sexual intercourse linked to suicidal ideation and attempts: findings from the 2006 Korean Youth Risk Behavior Survey. Yonsei medical journal. 2010;51(1):18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Swahn MH, Bossarte RM. Gender, Early Alcohol Use, and Suicide Ideation and Attempts: Findings from the 2005 Youth Risk Behavior Survey. Journal of Adolescent Health. 2007;41(2):175–181. [DOI] [PubMed] [Google Scholar]
- 4.Turecki G, Brent DA, Gunnell D, et al. Suicide and suicide risk. Nature Reviews Disease Primers. 2019;5(1):74. [DOI] [PubMed] [Google Scholar]
- 5.Sawyer SM, Azzopardi PS, Wickremarathne D, Patton GC. The age of adolescence. The Lancet Child & Adolescent Health. 2018;2(3):223–228. [DOI] [PubMed] [Google Scholar]
- 6.Kerr DCR, Capaldi DM, Pears KC, Owen LD. Intergenerational influences on early alcohol use: independence from the problem behavior pathway. Dev Psychopathol. 2012;24(3):889–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donovan JE, Molina BSG. Childhood risk factors for early-onset drinking. J Stud Alcohol Drugs. 2011;72(5):741–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huber RS, Sheth C, Renshaw PF, Yurgelun-Todd DA, McGlade EC. Suicide Ideation and Neurocognition Among 9- and 10-Year Old Children in the Adolescent Brain Cognitive Development (ABCD) Study. Archives of Suicide Research. 2020:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DeVille DC, Whalen D, Breslin FJ, et al. Prevalence and Family-Related Factors Associated With Suicidal Ideation, Suicide Attempts, and Self-injury in Children Aged 9 to 10 Years. JAMA Network Open 2020;3(2):e1920956–e1920956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Testa A, Weiss DB, Rennó Santos M. A Cross-National Analysis of Alcohol Consumption and Suicide Rates: Variations by Population-Level Drinking Patterns. Journal of Drug Issues. 2019;49(4):625–642. [Google Scholar]
- 11.Esposito-Smythers C, Spirito A. Adolescent substance use and suicidal behavior: a review with implications for treatment research. Alcohol Clin Exp Res. 2004;28(5 Suppl):77s–88s. [DOI] [PubMed] [Google Scholar]
- 12.Garavan H, Bartsch H, Conway K, et al. Recruiting the ABCD sample: Design considerations and procedures. Dev Cogn Neurosci. 2018;32:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Auchter AM, Hernandez Mejia M, Heyser CJ, et al. A description of the ABCD organizational structure and communication framework. Dev Cogn Neurosci. 2018;32:8–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Volkow ND, Koob GF, Croyle RT, et al. The conception of the ABCD study: From substance use to a broad NIH collaboration. Dev Cogn Neurosci. 2018;32:4–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heeringa SG, Berglund PA. A Guide for Population-based Analysis of the Adolescent Brain Cognitive Development (ABCD) Study Baseline Data. bioRxiv. 2020:2020.2002.2010.942011. [Google Scholar]
- 16.Barch DM, Albaugh MD, Avenevoli S, et al. Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: rationale and description. Developmental cognitive neuroscience. 2018;32:55–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Volkow ND, Koob GF, Croyle RT, et al. The conception of the ABCD study: From substance use to a broad NIH collaboration. Developmental cognitive neuroscience. 2018;32:4–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luciana M, Bjork JM, Nagel BJ, et al. Adolescent neurocognitive development and impacts of substance use: Overview of the adolescent brain cognitive development (ABCD) baseline neurocognition battery. Developmental Cognitive Neuroscience. 2018;32:67–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lisdahl KM, Sher KJ, Conway KP, et al. Adolescent brain cognitive development (ABCD) study: Overview of substance use assessment methods. Dev Cogn Neurosci. 2018;32:80–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Uban KA, Horton MK, Jacobus J, et al. Biospecimens and the ABCD study: Rationale, methods of collection, measurement and early data. Dev Cogn Neurosci. 2018;32:97–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaufman J, Birmaher B, Brent D, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. 1997;36(7):980–988. [DOI] [PubMed] [Google Scholar]
- 22.Townsend L, Kobak K, Kearney C, et al. Development of Three Web-Based Computerized Versions of the Kiddie Schedule for Affective Disorders and Schizophrenia Child Psychiatric Diagnostic Interview: Preliminary Validity Data. J Am Acad Child Adolesc Psychiatry. 2020;59(2):309–325. [DOI] [PubMed] [Google Scholar]
- 23.Jackson KM, Barnett NP, Colby SM, Rogers ML. The Prospective Association Between Sipping Alcohol by the Sixth Grade and Later Substance Use. J Stud Alcohol Drugs. 2015;76(2):212–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beautrais AL, Joyce PR, Mulder RT. Risk Factors for Serious Suicide Attempts among Youths Aged 13 through 24 Years. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35(9):1174–1182. [DOI] [PubMed] [Google Scholar]
- 25.Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L. Age- and Sex-Related Risk Factors for Adolescent Suicide. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(12):1497–1505. [DOI] [PubMed] [Google Scholar]
- 26.Bridge JA, Asti L, Horowitz LM, et al. Suicide trends among elementary school–aged children in the United States from 1993 to 2012. JAMA pediatrics. 2015;169(7):673–677. [DOI] [PubMed] [Google Scholar]
- 27.Cash SJ, Bridge JA. Epidemiology of youth suicide and suicidal behavior. Curr Opin Pediatr. 2009;21(5):613–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gould MS, Fisher P, Parides M, Flory M, Shaffer D. Psychosocial risk factors of child and adolescent completed suicide. Archives of general psychiatry. 1996;53(12):1155–1162. [DOI] [PubMed] [Google Scholar]
- 29.Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: a review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(4):386–405. [DOI] [PubMed] [Google Scholar]
- 30.Stover PJ, Harlan WR, Hammond JA, Hendershot T, Hamilton CM. PhenX: a toolkit for interdisciplinary genetics research. Current opinion in lipidology. 2010;21(2):136–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Achenbach TM, Ruffle TMJPir. The Child Behavior Checklist and related forms for assessing behavioral/emotional problems and competencies. 2000;21(8):265–271. [DOI] [PubMed] [Google Scholar]
- 32.O’Connor RC, Forgan G. Suicidal Thinking and Perfectionism: The Role of Goal Adjustment and Behavioral Inhibition/Activation Systems (BIS/BAS). Journal of Rational-Emotive & Cognitive-Behavior Therapy. 2007;25(4):321–341. [Google Scholar]
- 33.Ammerman BA, Kleiman EM, Jenkins AL, Berman ME, McCloskey MS. Using propensity scores to examine the association between behavioral inhibition/activation and nonsuicidal and suicidal self-injury. Crisis. 2016. [DOI] [PubMed] [Google Scholar]
- 34.Khosravani V, Baseri A, Kamali Z, Mohammadzadeh A, Amirinezhad A. Direct and Indirect Effects of Behavioral Inhibition/Activation Systems on Depression and Current Suicidal Ideation Through Rumination and Self-Reflection. Archives of Suicide Research. 2019:1–21. [DOI] [PubMed] [Google Scholar]
- 35.Bruni O, Ottaviano S, Guidetti V, et al. The Sleep Disturbance Scale for Children (SDSC). Construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J Sleep Res. 1996;5(4):251–261. [DOI] [PubMed] [Google Scholar]
- 36.Kessler RC, Avenevoli S, Costello EJ, et al. Design and field procedures in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A). International journal of methods in psychiatric research. 2009;18(2):69–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kessler RC, Avenevoli S, Costello EJ, et al. National comorbidity survey replication adolescent supplement (NCS-A): II. Overview and design. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(4):380–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Merikangas K, Avenevoli S, Costello J, Koretz D, Kessler RC. National comorbidity survey replication adolescent supplement (NCS-A): I. Background and measures. J Am Acad Child Adolesc Psychiatry. 2009;48(4):367–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chiu HY, Lee HC, Chen PY, Lai YF, Tu YK. Associations between sleep duration and suicidality in adolescents: A systematic review and dose-response meta-analysis. Sleep Med Rev. 2018;42:119–126. [DOI] [PubMed] [Google Scholar]
- 40.Hosmer DW Jr, Lemeshow S, Sturdivant RX. Applied logistic regression. Vol 398: John Wiley & Sons; 2013. [Google Scholar]
- 41.Norström T, Rossow I. Alcohol Consumption as a Risk Factor for Suicidal Behavior: A Systematic Review of Associations at the Individual and at the Population Level. Archives of Suicide Research. 2016;20(4):489–506. [DOI] [PubMed] [Google Scholar]
- 42.Borges G, Bagge CL, Cherpitel CJ, Conner KR, Orozco R, Rossow I. A meta-analysis of acute use of alcohol and the risk of suicide attempt. Psychological Medicine. 2017;47(5):949–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aseltine RH Jr., Schilling EA, James A, Glanovsky JL, Jacobs D. Age variability in the association between heavy episodic drinking and adolescent suicide attempts: findings from a large-scale, school-based screening program. J Am Acad Child Adolesc Psychiatry. 2009;48(3):262–270. [DOI] [PubMed] [Google Scholar]
- 44.Schilling EA, Aseltine RH Jr., Glanovsky JL, James A, Jacobs D. Adolescent alcohol use, suicidal ideation, and suicide attempts. J Adolesc Health. 2009;44(4):335–341. [DOI] [PubMed] [Google Scholar]
- 45.Sellers Cm, Diaz-Valdes Iriarte A, Wyman Battalen A, O'Brien KHM. Alcohol and marijuana use as daily predictors of suicide ideation and attempts among adolescents prior to psychiatric hospitalization. Psychiatry Research. 2019;273:672–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang X, Wu L-T. Suicidal ideation and substance use among adolescents and young adults: A bidirectional relation? Drug and Alcohol Dependence. 2014;142:63–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brick LA, Marraccini ME, Micalizzi L, Benca-Bachman CE, Knopik VS, Palmer RHC. Overlapping genetic effects between suicidal ideation and neurocognitive functioning. Journal of Affective Disorders. 2019;249:104–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Taubitz LE, Pedersen WS, Larson CL. BAS Reward Responsiveness: A unique predictor of positive psychological functioning. Personality and Individual Differences. 2015;80:107–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Luby JL, Whalen D, Tillman R, Barch DM. Clinical and Psychosocial Characteristics of Young Children With Suicidal Ideation, Behaviors, and Nonsuicidal Self-Injurious Behaviors. Journal of the American Academy of Child and Adolescent Psychiatry. 2019;58(1):117–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bernert RA, Kim JS, Iwata NG, Perlis ML. Sleep disturbances as an evidence-based suicide risk factor. Curr Psychiatry Rep. 2015;17(3):554–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stanley IH, Hom MA, Luby JL, et al. Comorbid sleep disorders and suicide risk among children and adolescents with bipolar disorder. J Psychiatr Res. 2017;95:54–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bridge JA, Horowitz LM, Fontanella CA, Grupp-Phelan J, Campo JV. Prioritizing research to reduce youth suicide and suicidal behavior. Am J Prev Med. 2014;47(3 Suppl 2):S229–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Horowitz LM, Ballard ED. Suicide screening in schools, primary care and emergency departments. Curr Opin Pediatr. 2009;21(5):620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.O'Leary CC, Frank DA, Grant-Knight W, et al. Suicidal ideation among urban nine and ten year olds. J Dev Behav Pediatr. 2006;27(1):33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Horowitz LM, Bridge JA, Teach SJ, et al. Ask Suicide-Screening Questions (ASQ): a brief instrument for the pediatric emergency department. Arch Pediatr Adolesc Med. 2012;166(12):1170–1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Horowitz LM, Wang PS, Koocher GP, et al. Detecting suicide risk in a pediatric emergency department: development of a brief screening tool. Pediatrics. 2001;107(5):1133–1137. [DOI] [PubMed] [Google Scholar]
- 57.Rubin R Screening Preteens in the Emergency Department for Suicide Risk. JAMA. 2019;321(16):1557–1557. [DOI] [PubMed] [Google Scholar]
- 58.Ng MY, Weisz JR. Annual Research Review: Building a science of personalized intervention for youth mental health. Journal of Child Psychology and Psychiatry. 2016;57(3):216–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Das JK, Salam RA, Lassi ZS, et al. Interventions for Adolescent Mental Health: An Overview of Systematic Reviews. J Adolesc Health. 2016;59(4s):S49–s60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Robinson J, Bailey E, Witt K, et al. What Works in Youth Suicide Prevention? A Systematic Review and Meta-Analysis. EClinicalMedicine. 2018;4-5:52–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tishler CL, Reiss NS, Rhodes AR. Suicidal behavior in children younger than twelve: a diagnostic challenge for emergency department personnel. Acad Emerg Med. 2007;14(9):810–818. [DOI] [PubMed] [Google Scholar]
- 62.Frankenfield DL, Keyl PM, Gielen A, Wissow LS, Werthamer L, Baker SP. Adolescent patients--healthy or hurting? Missed opportunities to screen for suicide risk in the primary care setting. Arch Pediatr Adolesc Med. 2000;154(2):162–168. [DOI] [PubMed] [Google Scholar]
- 63.Stone R Pregnant women and substance use: fear, stigma, and barriers to care. Health & Justice. 2015;3(1):2. [Google Scholar]
- 64.Johnson T, Fendrich M. Modeling Sources of Self-report Bias in a Survey of Drug Use Epidemiology. Annals of Epidemiology. 2005;15(5):381–389. [DOI] [PubMed] [Google Scholar]
- 65.Richards JE, Whiteside U, Ludman EJ, et al. Understanding Why Patients May Not Report Suicidal Ideation at a Health Care Visit Prior to a Suicide Attempt: A Qualitative Study. Psychiatr Serv. 2019;70(1):40–45. [DOI] [PubMed] [Google Scholar]
- 66.Chung T, Hipwell A, Loeber R, White HR, Stouthamer-Loeber M. Ethnic Differences in Positive Alcohol Expectancies During Childhood: The Pittsburgh Girls Study. Alcoholism: Clinical and Experimental Research. 2008;32(6):966–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pitkänen T, Lyyra A-L, Pulkkinen L. Age of onset of drinking and the use of alcohol in adulthood: a follow-up study from age 8–42 for females and males. Addiction. 2005; 100(5):652–661. [DOI] [PubMed] [Google Scholar]
- 68.Aguinaldo LD, Sullivant S, Lanzillo EC, Ross A, He JP, Bradley-Ewing A, Bridge JA, Horowitz LM, Wharff EA. Validation of the ask suicide-screening questions (ASQ) with youth in outpatient specialty and primary care clinics. General Hosp Psychiatry. 2020. November 13;68:52–58. doi: 10.1016/j.genhosppsych.2020.11.006. Epub ahead of print. PMID: 33310014. [DOI] [PMC free article] [PubMed] [Google Scholar]


