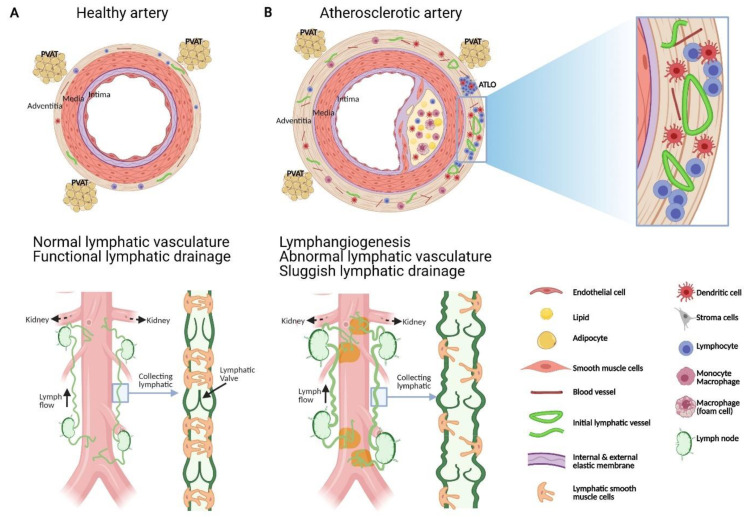
Figure 1.
Schematic representation of the structural and functional changes affecting adventitial lymphatic vessels during atherosclerosis. (A) Artery is formed by three layers, namely: the tunica intima (inner layer) lined by a monolayer of endothelial cells, the tunica media composed of SMCs, elastin and collagen, and the adventitia, the outer layer formed of fibroblast, collagen, nerve endings, immune cells, blood and lymphatic vessels. Periadventitial adipose tissue (PVAT) is also distributed around arteries. (B) Atherosclerosis is characterized by the accumulation of plaques comprising cholesterol, inflammatory soluble factors, immune cells in the intima and inflammation in adventitia that can be associated with the formation of adventitia tertiary lymphoid organ (ATLOs) when the disease is more advanced. (A) Similar to lymphatic vessels in other tissues, initial lymphatic vessels in the adventitia converge into larger collecting vessels exhibiting SMC and valves which transport lymph into draining lymph nodes. (B) Studies have shown that atherosclerosis is associated with angiogenesis and lymphangiogenesis. Notably, in the abdominal aorta, initial lymphatic vessels appeared more dilated and lymphatic drainage of macromolecule from the adventitia into the draining lymph node is severely compromised during atherosclerosis. Alterations in collecting vessels such as poor SMC coverage, abnormal valve and accumulation of extracellular matrix such as collagen, may account for the impaired lymphatic drainage. These functional defects in adventitial lymphatic vessels may participate to the retention of immune cells, inflammatory cytokines, and lipids in the arterial wall which in turn favour the progression of atherosclerotic plaque, inflammation and ATLOs. Restoring lymphatic drainage in the arterial wall may thus be a promising strategy to treat atherosclerosis.