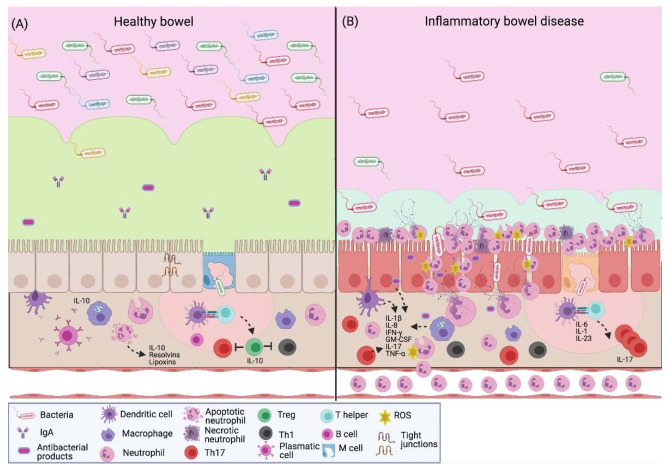
Figure 2.
NETs in inflammatory bowel disease. (A) The intestinal barrier protects the host against pathogens; it promotes homeostasis between the commensal microbiota and the immune system. In healthy intestinal mucosa, the epithelium is covered with mucus that contains antimicrobial peptides and IgA. In the lamina propria, immune cells are strategically distributed to initiate a response. There is a constant antigen presentation to establish immune tolerance towards the gut microbiota. Mucosal neutrophils prevent the antigen translocation; their apoptosis promotes mucosal injury repair through the secretion of resolvins and lipoxins; it also leads to the M2-type macrophages, which secrete IL-10 to create a microenvironment where Treg lymphocytes predominate. (B) Patients with IBD present dysbiosis and a low expression of tight junction proteins, which leads to an increase in intestinal permeability. Epithelial and immune cells produce proinflammatory cytokines (IL-1β, IL-8, IFN-γ, GM-CSF, TNF-α and IL-17) that increase the transendothelial migration and neutrophil activation to create a microenvironment where the activity of Th17 lymphocytes predominates. Neutrophils respond to luminal antigens through a respiratory burst, degranulation and the release of extracellular traps with antimicrobial factors, such as elastase and myeloperoxidase, which contribute to the characteristic colonic tissue damage in these patients. IgA, immunoglobulin A; IL-1β, interleukin-1β; IL-6, interleukin-6; IL-8, interleukin-8; IL-10, interleukin-10; IL-17, interleukin-17; IL-23, interleukin-23; IFN-γ, interferon gamma; GM-CSF, granulocyte-macrophage colony-stimulating factor; TNF-α, tumor necrosis factor- α; ROS, reactive oxygen species. Created with BioRender.com.