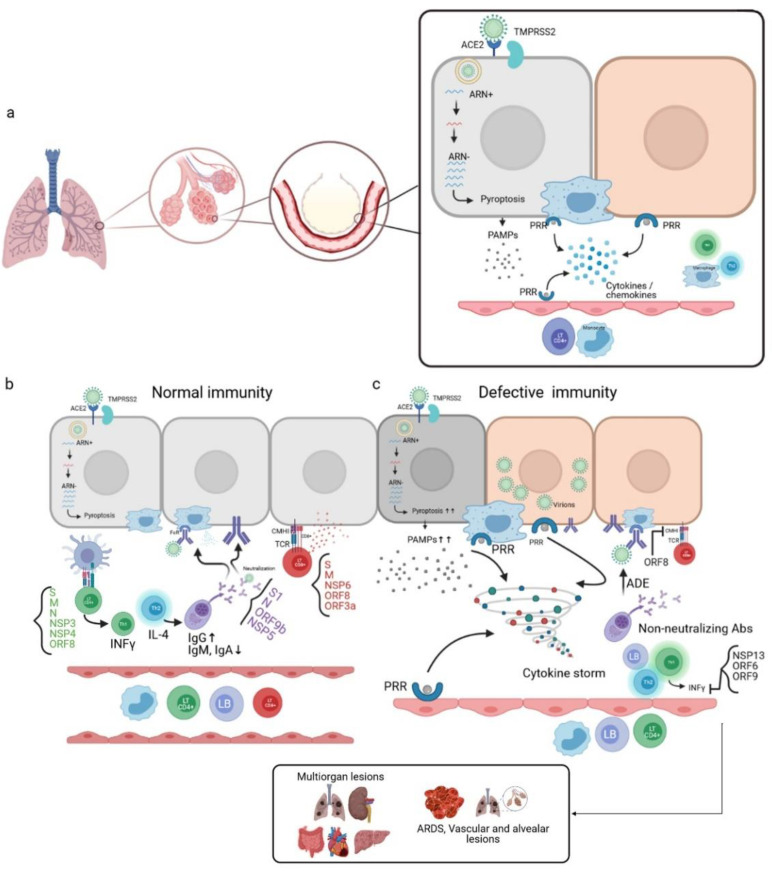
Figure 5.
Mechanism of the immune response during SARS-CoV-2 infection. (a) SARS-CoV-2 penetrates the host cell by endocytosis through the Spike binding to the ACE2R present in alveolar epithelial cells. The active replication of the virus and the release of virions lead to pyroptosis, and, therefore, the release of pathogen-associated molecular patterns (PAMPs) recognized by pattern recognition receptors (PRRs) of neighboring alveolar epithelial cells, alveolar macrophages, and endothelial cells. This leads to the production of pro-inflammatory cytokines/chemokines, which in turn attract other immune cells to the infection site. (b) In the case of a normal immune system, CD4 + LTs recognize antigen-MHCII complexes of antigen-presenting cells (APCs). This induces the differentiation of CD4 + LTs into Th1, which is the producer of INFγ. CD4 + LTs can also differentiate into Th2, the producer of IL-4, which activates the LBs into plasma cells that produce neutralizing antibodies; these antibodies target several virus antigens and promote viral phagocytosis through the opsonization phenomenon. The CD8 + LTs recognize the antigens presented by the infected cells through the interaction of their TCRs with the CMHI of the infected cells, thus leading to cell death by cytotoxicity. (c) In the case of a defective immune system, a high level of pyroptosis induces a cytokine storm; non-neutralizing antibodies are produced, which are responsible for the antibody-dependent enhancement (ADE) phenomenon. In addition, inhibition of the production of INFγ occurs due to the involvement of certain viral proteins responsible for immune escape. This unbalanced immune response leads to multiorgan lesions, acute-respiratory-distress-syndrome (ARDS), and alveolar and vascular lesions [7,57]. (Designed by biorender).