Fig. 6.
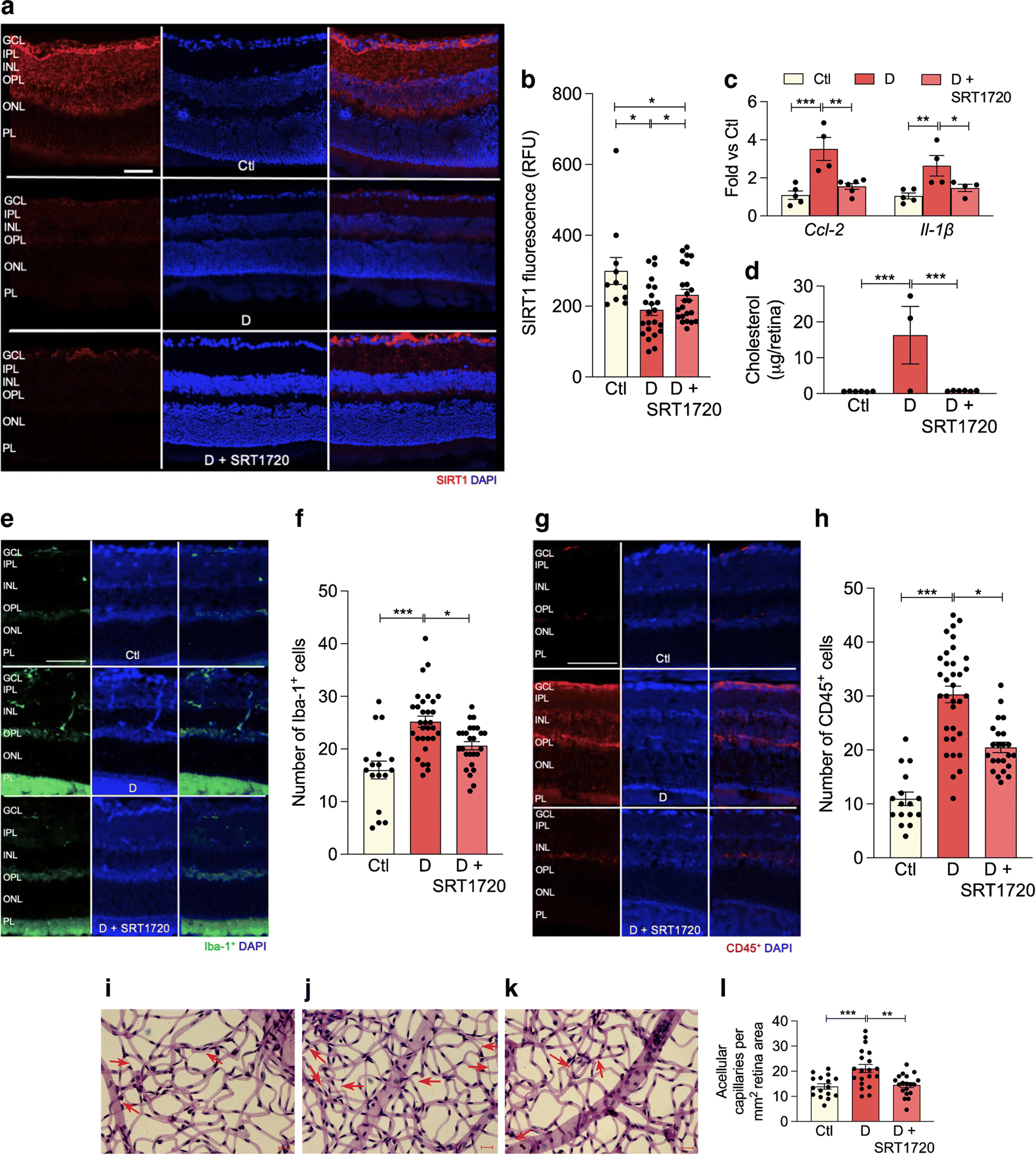
SRT1720 increases SIRT1 expression in retina of db/db mice with 6 month duration of diabetes. (a) Retinal sections from non-diabetic controls (top), diabetic mice fed normal chow (middle) or chow containing SRT1720 (bottom) were stained with anti-SIRT1 antibody (red) and DAPI was used to stain nuclei (blue). Quantification is shown in (b); several replicate samples were stained from n=4 mice. (c, d) Diabetes significantly increases proinflammatory markers Ccl-2, Il-1β mRNA expression (c) and significantly increases retinal cholesterol levels (mass spectrometry analysis) (d); the SIRT1 agonist SRT1720 restores Ccl-2 and Il-1β (c) and cholesterol (d), to non-diabetic levels; n=4–5 mice. (e–h) Diabetes increases, while SRT1720 normalises, the cell number of Iba-1+ (e, f) and CD45+ (g, h) cells in the retina, n=5 from 3 to 5 sections at 100 µm interval for each eye with a minimum of four images for section. (i–l) Acellular capillary formation (red arrows) was examined in non-diabetic animals (i), and in diabetic animals fed control chow (j) or chow containing SRT1720 (k). Diabetes significantly increases acellular capillary formation (j) while administration of the SIRT1 agonist prevents diabetes-induced acellular capillary formation (k). Quantification is shown in (l); n=5 from 4 to 5 images per mm2 retina area; *p<0.05, **p<0.01,***p<0.001. Data are represented as mean ± SEM. Scale bars, 20 µm. Ctl, control (db/m); D, diabetic (db/db); GCL, ganglion cell layer; INL, inner nuclear layer; IPL, inner plexiform layer; ONL, outer nuclear layer; OPL, outer plexiform layer; PL, photoreceptor layer. RFU, relative fluorescence units
