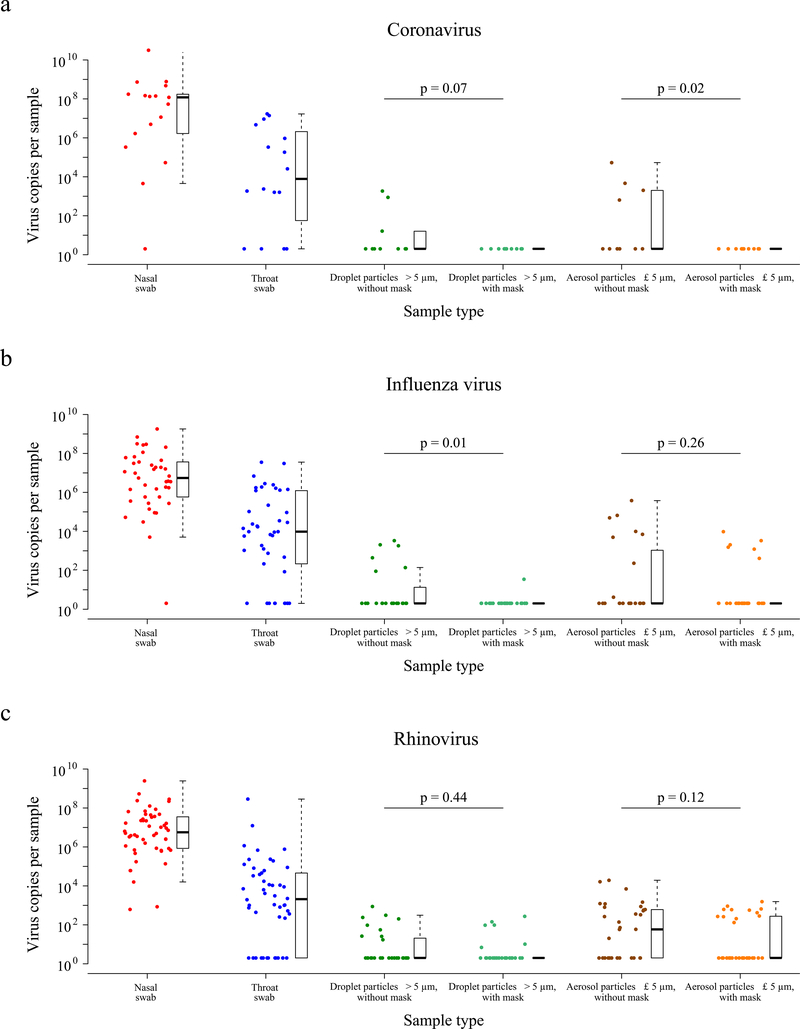
Figure 1. Efficacy of surgical face masks in reducing respiratory virus shedding in respiratory droplets and aerosols of symptomatic individuals with (a) coronavirus, (b) influenza virus or (c) rhinovirus infection.
The figure showed the virus copies per sample collected in nasal swab (red), throat swab (blue), respiratory droplets collected for 30 minutes while not wearing (dark green) or wearing (light green) a surgical face mask, and aerosols collected for 30 minutes while not wearing (brown) or wearing (orange) a face mask, collected from individuals with acute respiratory symptoms who were RT-PCR positive for coronavirus, influenza virus and rhinovirus in any samples. P-values for mask intervention as predictor of log10virus copies per sample in an unadjusted univariate Tobit regression model which allowed for censoring at the lower limit of detection of the RT-PCR assay were shown, with significant difference in bold. For nasal swabs and throat swabs, all infected individuals were included (coronavirus, n = 17; influenza virus, n = 43; rhinovirus, n = 54). For respiratory droplets and aerosols, numbers of infected individuals who provided exhaled breath samples while not wearing, or wearing, a surgical face mask respectively were: coronavirus (n = 10, 11), influenza virus (n = 23, 28), rhinovirus (n = 36, 32). A subset of participants provided exhaled breath samples for both mask intervention (coronavirus, n = 4; influenza virus, n = 8; rhinovirus, n = 14). The box plots indicated the median with the interquartile range (lower/ upper hinge) and ± 1.5*interquartile range from the first/ third quartile (lower/ upper whisker).