Abstract
Aims
To evaluate the impact of chronic obstructive pulmonary disease (COPD) on 10-year all-cause death and the treatment effect of CABG versus PCI on 10-year all-cause death in patients with three-vessel disease (3VD) and/or left main coronary artery disease (LMCAD) and COPD.
Methods
Patients were stratified according to COPD status and compared with regard to clinical outcomes. Ten-year all-cause death was examined according to the presence of COPD and the revascularization strategy.
Results
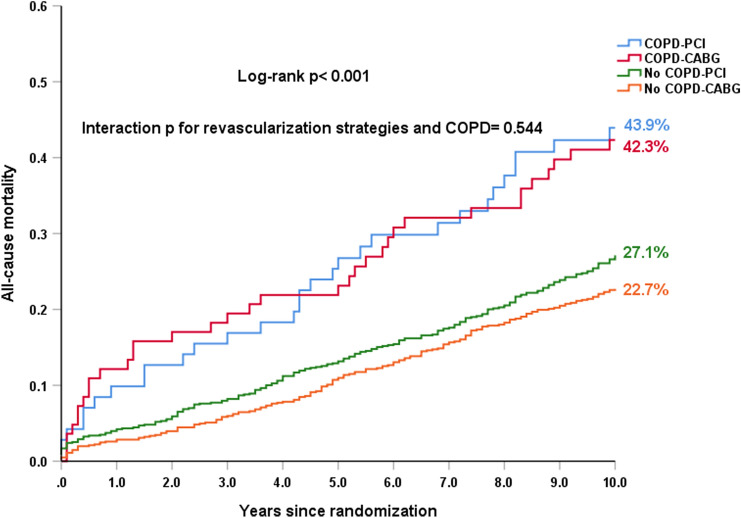
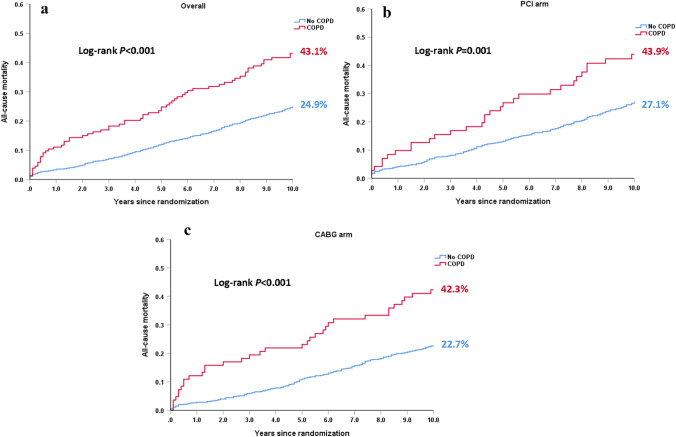
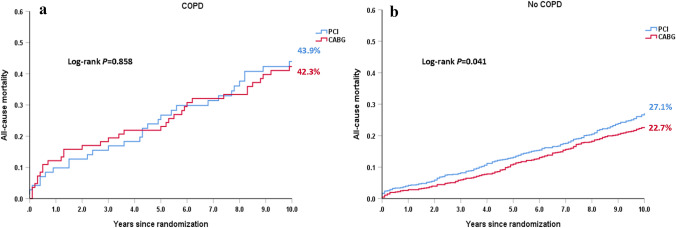
COPD status was available for all randomized 1800 patients, of whom, 154 had COPD (8.6%) at the time of randomization. Regardless of the revascularization strategy, patients with COPD had a higher risk of 10-year all-cause death, compared with those without COPD (43.1% vs. 24.9%; hazard ratio [HR]: 2.03; 95% confidence interval [CI]: 1.56–2.64; p < 0.001). Among patients with COPD, CABG appeared to have a slightly lower risk of 10-year all-cause death compared with PCI (42.3% vs. 43.9%; HR: 0.96; 95% CI: 0.59–1.56, p = 0.858), whereas among those without COPD, CABG had a significantly lower risk of 10-year all-cause death (22.7% vs. 27.1%; HR: 0.81; 95% CI: 0.67–0.99, p = 0.041). There was no significant differential treatment effect of CABG versus PCI on 10-year all-cause death between patients with and without COPD (p interaction = 0.544).
Conclusions
COPD was associated with a higher risk of 10-year all-cause death after revascularization for complex coronary artery disease. The presence of COPD did not significantly modify the beneficial effect of CABG versus PCI on 10-year all-cause death.
Trial registration: SYNTAX: ClinicalTrials.gov reference: NCT00114972. SYNTAX Extended Survival: ClinicalTrials.gov reference: NCT03417050
Graphic abstract
Keywords: All-cause death, Chronic obstructive pulmonary disease, Coronary artery bypass grafting, Percutaneous coronary intervention, SYNTAX
Introduction
Chronic obstructive pulmonary disease (COPD) is associated with accelerated atherosclerosis and cardiovascular disease; therefore, they frequently coexist [1, 2]. Known as a risk factor for cardiovascular mortality [3], the status of COPD is a variable in the formula to calculate SYNTAX score II [4–6], Southern Thoracic Society (STS) score [7], EuroSCORE II [8], and more recently—the SYNTAX score II 2020 [9]. Patients with COPD are perceived to be at increased surgical risk, and are often referred to percutaneous coronary intervention (PCI) instead of coronary bypass artery grafting (CABG). However, limited data support this preference. Most studies have indeed demonstrated that COPD patients undergoing CABG had increased in-hospital and long-term mortality [10, 11], whilst some studies reported discrepant results [12, 13]. On the other hand, patients with COPD who underwent PCI have worse prognosis compared with those without COPD [14–17]. Furthermore, in the EXCEL (Evaluation of XIENCE Versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization) trial, COPD was associated with worse clinical outcomes after left main coronary artery disease (LMCAD) revascularization. Yet the relative risks of PCI versus CABG at 30 days and 3 years were similar irrespective of the presence of COPD in this specific subset of patients [18]. Currently, therefore, the optimal revascularization strategy for patients with COPD and complex CAD remains debatable.
The SYNTAX Extended Survival (SYNTAXES) study reported the 10-year all-cause mortality in 94% of all the patients with de novo three-vessel disease (3VD) and/or LMCAD who were originally randomized to CABG or PCI in the SYNTAX trial [19]. In the present study, we aimed 1) to evaluate the impact of COPD on 10-year all-cause mortality and 2) to estimate the treatment effect of CABG versus PCI for 10-year all-cause mortality according to COPD in patients with 3VD and/or LMCAD.
Methods
Study design and population
The design and the primary results of the SYNTAX trial have been published elsewhere [20–22]. In brief, the SYNTAX trial (NCT00114972) was an international, multicenter, randomized controlled trial conducted between March 2005 and April 2007. Based on clinical judgment and the consensus of a Heart Team, all-comers patients with de novo 3VD and/or LMCAD deemed eligible for both PCI and CABG were enrolled and randomized in a 1:1 fashion to either CABG (n = 897) or PCI (n = 903) with the TAXUS Express paclitaxel-drug eluting stents (Boston Scientific Corporation, Marlborough, MA, USA). The trial completed the patient follow-up to 5 years [22]. The SYNTAXES study (NCT03417050) was an investigator-driven initiative that extended follow-up and aimed to evaluate vital status up to 10 years [19]. The longest follow-up was 14.1 years. The extended follow-up study was funded by the German Heart Research Foundation (GHF; Frankfurt am Main, Germany). Follow-up was conducted in accordance with local regulations of each participating center and complied with the declaration of Helsinki.
Definitions and endpoints
COPD at baseline was defined as long-term use of bronchodilators or steroids for lung disease according to the definition in EuroSCORE [23]. The primary endpoint of the SYNTAXES study was all-cause death at 10 years. The 30-day and 5-year major adverse cardiovascular and cerebrovascular events (MACCE, defined as a composite endpoint of all-cause death, cerebrovascular accident, myocardial infarction [MI] or repeat revascularization, the primary endpoint of the SYNTAX trial) according to the status of COPD were also explored in the current analysis. Vital status was confirmed by contact with medical care personnel and/or by electronic healthcare record review and national death registry.
Statistical analysis
All the analyses were performed according to the intention to treat principle. Continuous variables are reported as mean ± standard deviations, and were compared using Student’s t test or Mann–Whitney U test. Categorical variables are shown as percentages and numbers and were compared using Fisher’s exact test. Time-to-event Kaplan–Meier estimates with log-rank test were used to compare COPD versus non-COPD in the PCI and CABG arm, respectively, and to compare PCI with CABG according to COPD. Cox proportional hazards regression was used to calculate hazard ratios (HRs) with 95% confidence interval (CI). Multivariate analysis was performed to investigate whether COPD was an independent predictor of all-cause death at 10 years. The Cox proportional hazards regression model included the following covariates: age, gender, body mass index, current smoking, peripheral vascular disease, left ventricular ejection fraction (LVEF), creatinine clearance (ml/min), prior MI, prior stroke, and the anatomical SYNTAX score, which have been selected based on previous knowledge of the association of those variables with the clinical outcomes [24]. All analyses were performed using SPSS Statistics, version 25 (IBM Corp., Armonk, 281 N.Y., USA) and a p value of < 0.05 was considered to be statistically significant.
Results
Baseline characteristics
COPD status was available in all patients randomized in the SYNTAX trial. Of the 1800 participants, 154 (8.6%) had COPD. Baseline characteristics according to COPD status are shown in Table 1. Patients with COPD were more likely to be older, had more cardiovascular risk factors (previous carotid artery disease, peripheral vascular disease, congestive heart failure, and current smoking), and had a higher EuroSCORE and Parsonnet SCORE, as compared to those without COPD. They were less likely to receive arterial conduits and to take aspirin and beta blockers at discharge. Baseline clinical and procedural characteristics according to COPD as well as randomized revascularization strategies are reported in Table 2. By randomization, baseline clinical and procedural characteristics were largely well balanced between PCI and CABG in patients with and without COPD.
Table 1.
Baseline characteristics according to COPD
| COPD (n = 154) | No COPD (n = 1646) | p value | |
|---|---|---|---|
| PCI | 46.1 (71/154) | 50.5 (832/1646) | 0.292 |
| CABG | 53.9 (83/154) | 49.5 (814/1646) | |
| Age (year) | 66.9 ± 8.7 | 64.9 ± 9.8 | 0.017 |
| Sex | |||
| Male | 73.4 (113/154) | 78.1 (1285/1646) | 0.181 |
| Body mass index (kg/m2) | 28.6 ± 5.6 | 28.0 ± 4.6 | 0.164 |
| Medically treated diabetes | 29.2 (45/154) | 24.7 (407/1646) | 0.219 |
| On insulin | 13 (20/154) | 9.8 (162/1646) | 0.216 |
| Metabolic syndrome | 40.3 (62/154) | 36.1 (594/1646) | 0.352 |
| Hypertension | 71.4 (110/154) | 66 (1086/1646) | 0.171 |
| Dyslipidemia | 77.8 (119/153) | 77.9 (1272/1632) | 0.963 |
| Current smoker | 27.9 (43/154) | 19.5 (320/1639) | 0.013 |
| Previous MI | 36 (54/150) | 32.6 (531/1630) | 0.393 |
| Previous stroke | 5.3 (8/150) | 4.3 (70/1639) | 0.542 |
| Previous TIA | 7.3 (11/151) | 4.5 (73/1638) | 0.116 |
| Previous carotid artery disease | 16.2 (25/154) | 7.5 (123/1646) | < 0.001 |
| PVD | 19.5 (30/154) | 8.9 (147/1646) | < 0.001 |
| Impaired renal function | 22.1 (34/154) | 17.1 (282/1646) | 0.155 |
| Creatinine clearance (ml/min) | 84.8 ± 32.9 | 86.2 ± 32.7 | 0.630 |
| LVEF (%) | 56.9 ± 14.2 | 58.8 ± 12.9 | 0.171 |
| Congestive heart failure | 8.5 (13/153) | 4.3 (70/1625) | 0.019 |
| Clinical presentation | 0.432 | ||
| Silent ischemia | 14.9 (23/154) | 14.4 (237/1646) | |
| Stable angina | 61 (94/154) | 56.7 (933/1646) | |
| Unstable angina | 24 (37/154) | 28.9 (476/1646) | |
| Euro SCORE | 5.2 ± 2.9 | 3.6 ± 2.6 | < 0.001 |
| Parsonnet SCORE | 9.9 ± 6.9 | 8.4 ± 6.9 | 0.008 |
| Disease extent | 0.956 | ||
| 3VD | 60.8 (1001/1646) | 61 (94/154) | |
| LMCAD | 39 (60/154) | 39.2 (645/1646) | |
| Disease extent | 0.806 | ||
| LMCAD only | 6.5 (10/153) | 4.9 (81/1646) | |
| LMCAD + 1VD | 7.8 (12/153) | 7.7 (126/1646) | |
| LMCAD + 2VD | 13.7 (21/153) | 12 (1646/241) | |
| LMCAD + 3VD | 11.1 (17/153) | 14.6 (241/1646) | |
| 2VD | 2 (3/153) | 2 (33/1646) | |
| 3VD | 58.8 (90/153) | 58.8 (968/1646) | |
| Anatomical SYNTAX score | 29.6 ± 11.8 | 28.7 ± 11.4 | 0.344 |
| Number of lesions | 4.5 ± 1.9 | 4.3 ± 1.8 | 0.461 |
| Any total occlusion | 18.3 (28/153) | 23.7 (387/1634) | 0.132 |
| Any bifurcation | 76.5 (117/153) | 72.4 (1183/1634) | 0.279 |
| Number of stents | 4.6 ± 2.6 | 4.6 ± 2.2 | 0.924 |
| TSL per patient | 85.5 ± 52.9 | 85.7 ± 47.5 | 0.980 |
| Off pump CABG | 4.5 (7/154) | 7.5 (123/1646) | 0.215 |
| LIMA use | 44.2 (68/154) | 41.1 (676/1646) | 0.757 |
| Number of total conduits | 2.7 ± 0.8 | 2.8 ± 0.7 | 0.754 |
| Number of arterial conduits | 1.2 ± 0.5 | 1.4 ± 0.7 | 0.001 |
| Number of venous conduits | 1.5 ± 0.9 | 1.3 ± 0.9 | 0.103 |
| Complete revascularization | 61.6 (93/151) | 59.8 (965/1615) | 0.660 |
| Medication at discharge | |||
| Aspirin | 87.4 (132/151) | 92.9 (1501/1615) | 0.014 |
| Thienopyridine | 53.6 (81/151) | 59.2 (956/1615) | 0.185 |
| Statin | 78.8 (119/151) | 80.9 (1306/1615) | 0.540 |
| Beta blockers | 60.3 (91/151) | 81.8 (1321/1615) | < 0.001 |
| ACEI | 47.7 (72/151) | 50.2 (810/1615) | 0.561 |
| ARB | 14.6 (22/151) | 9.8 (158/1615) | 0.063 |
ACEI angiotensin-converting enzyme inhibitors, ARB angiotensin II receptor blockers, CABG coronary bypass artery grafting, LMCAD left main coronary artery disease, LVEF left ventricular ejection fraction, MI myocardial infarction, PCI percutaneous coronary intervention, PVD peripheral vascular disease, TIA transient ischemia attack, TSL total stent length, 3VD three-vessel disease
Table 2.
Baseline characteristics according to COPD and revascularization strategies
| COPD (N = 154) | p value | No COPD (N = 1646) | p value | |||
|---|---|---|---|---|---|---|
| PCI (N = 71) | CABG (N = 83) | PCI (N = 832) | CABG (N = 814) | |||
| Age (year) | 66.8 ± 8.9 | 67 ± 8.5 | 0.916 | 65.1 ± 9.7 | 64.8 ± 9.9 | 0.476 |
| Sex | ||||||
| Male | 71.8 (51/71) | 74.7 (62/83) | 0.688 | 76.8 (639/832) | 79.4 (646/814) | 0.210 |
| Body mass index (kg/m2) | 29.3 ± 5.5 | 28 ± 5.6 | 0.147 | 28 ± 4.7 | 27.9 ± 4.4 | 0.648 |
| Medically treated diabetes | 33.8 (24/71) | 25.3 (21/83) | 0.248 | 24.9 (207/832) | 24.6 (200/814) | 0.884 |
| On insulin | 14.1 (10/71) | 12 (10/83) | 0.708 | 9.5 (79/832) | 10.2 (83/814) | 0.633 |
| Metabolic syndrome | 46.5 (33/71) | 34.9 (29/83) | 0.032 | 36.8 (306/832) | 35.4 (288/814) | 0.380 |
| Hypertension | 74.6 (53/71) | 68.7 (57/83) | 0.413 | 68.4 (569/832) | 63.5 (517/814) | 0.037 |
| Dyslipidemia | 76.1 (54/71) | 79.3 (65/82) | 0.634 | 78.9 (651/825) | 77 (621/807) | 0.340 |
| Current smoker | 25.4 (18/71) | 30.1 (25/83) | 0.511 | 17.9 (149/832) | 21.2 (171/807) | 0.094 |
| Previous MI | 33.3 (23/69) | 38.3 (31/81) | 0.530 | 31.8 (262/824) | 33.4 (269/806) | 0.497 |
| Previous stroke | 7.2 (5/69) | 3.7 (3/81) | 0.336 | 3.6 (30/830) | 4.9 (40/809) | 0.183 |
| Previous TIA | 10 (7/70) | 4.9 (4/81) | 0.233 | 3.9 (32/831) | 5.1 (41/807) | 0.228 |
| Previous carotid artery disease | 19.7 (14/71) | 13.3 (11/83) | 0.278 | 7.1 (59/832) | 7.9 (64/814) | 0.552 |
| PVD | 21.1 (15/71) | 18.1 (15/83) | 0.633 | 8.1 (67/832) | 9.8 (80/814) | 0.207 |
| Impaired renal function | 23.9 (17/71) | 20.5 (17/83) | 0.139 | 18 (150/832) | 16.2 (132/814) | < 0.001 |
| Creatinine clearance (ml/min) | 86.2 ± 34.7 | 83.6 ± 31.3 | 0.650 | 86.7 ± 35.6 | 85.7 ± 29.3 | 0.565 |
| LVEF (%) | 58.2 ± 12.3 | 55.6 ± 15.9 | 0.363 | 59.1 ± 13 | 58.5 ± 12.9 | 0.453 |
| Congestive heart failure | 4.2 (3/71) | 12.2 (10/82) | 0.078 | 4 (33/827) | 4.6 (37/798) | 0.521 |
| Clinical presentation | 0.138 | 0.998 | ||||
| Silent ischemia | 9.9 (7/71) | 19.3 (16/83) | 14.4 (120/832) | 14.4 (117/814) | ||
| Stable angina | 60.6 (43/71) | 61.4 (51/83) | 56.6 (471/832) | 56.8 (462/814) | ||
| Unstable angina | 29.6 (21/71) | 19.3 (16/83) | 29 (241/832) | 28.9 (235/814) | ||
| Euro SCORE | 5.4 ± 3 | 5.1 ± 2.7 | 0.636 | 3.6 ± 2.5 | 3.6 ± 2.7 | 0.802 |
| Parsonnet SCORE | 10.5 ± 7.4 | 9.4 ± 6.5 | 0.343 | 8.4 ± 6.9 | 8.3 ± 6.9 | 0.924 |
| Disease extent | 0.657 | 0.842 | ||||
| 3VD | 59.2 (42/71) | 62.7 (52/83) | 60.6 (504/832) | 61.1 (497/814) | ||
| LMCAD | 40.8 (29/71) | 37.3 (31/83) | 39.4 (328/832) | 38.9 (317/814) | ||
| Disease extent | 0.983 | 0.915 | ||||
| LMCAD only | 7 (5/71) | 6.1 (5/82) | 4.4 (37/832) | 5.4 (44/814) | ||
| LMCAD + 1VD | 7 (5/71) | 8.5 (7/82) | 7.5 (62/832) | 7.9 (64/814) | ||
| LMCAD + 2VD | 14.1 (71/9) | 13.4 (11/82) | 12.3 (832/127) | 11.7 (95/814) | ||
| LMCAD + 3VD | 12.7 (9/71) | 9.8 (8/82) | 15.3 (127/832) | 14 (114/814) | ||
| 2VD | 1.4 (1/71) | 2.4 (2/82) | 1.9 (16/832) | 2.1 (17/814) | ||
| 3VD | 57.7 (41/71) | 59.8 (49/82) | 58.7 (488/832) | 59 (480/814) | ||
| Anatomical SYNTAX score | 30 ± 12.6 | 29.2 ± 11.1 | 0.666 | 28.3 ± 11.4 | 29.1 ± 11.4 | 0.149 |
| Number of lesions | 4.5 ± 2 | 4.4 ± 1.8 | 0.643 | 4.3 ± 1.8 | 4.4 ± 1.8 | 0.426 |
| Any total occlusion | 25.4 (18/71) | 12.2 (10/82) | 0.036 | 24.1 (199/826) | 23.3 (188/808) | 0.695 |
| Any bifurcation | 74.6 (53/71) | 78 (64/82) | 0.621 | 72.2 (596/826) | 72.6 (587/808) | 0.823 |
| Number of stents | 4.7 ± 2.6 | – | 4.6 ± 2.2 | – | ||
| TSL per patient | 86.6 ± 53.2 | – | 86.4 ± 47.5 | – | ||
| Off pump CABG | – | 8.4 (7/83) | – | 14.9 (121/814) | ||
| LIMA use | – | 81.9 (68/83) | – | 81.8 (666/814) | ||
| Number of total conduits | – | 2.7 ± 0.8 | – | – | 0.300 | |
| Number of arterial conduits | – | 1.2 ± 0.5 | – | – | 0.005 | |
| Number of venous conduits | – | 1.5 ± 0.9 | – | – | 0.700 | |
| Complete revascularization | 53.5 (38/71) | 68.8 (55/80) | 0.055 | 57 (470/825) | 62.7 (495/790) | 0.020 |
| Medication at discharge | ||||||
| Aspirin | 93 (66/71) | 82.5 (66/80) | 0.053 | 96.6 (797/825) | 89.1 (704/790) | < 0.001 |
| Thienopyridine | 94.4 (67/71) | 17.5 (14/80) | < 0.001 | 97 (800/825) | 19.7 (156/790) | < 0.001 |
| Statin | 84.5 (60/71) | 73.8 (59/80) | 0.106 | 86.9 (717/825) | 74.6 (589/790) | < 0.001 |
| Beta blockers | 56.3 (40/71) | 63.8 (51/80) | 0.353 | 83.4 (688/825) | 80.1 (633/790) | 0.089 |
| ACEI | 49.3 (35/71) | 46.3 (37/80) | 0.708 | 55.6 (459/825) | 44.4 (351/790) | < 0.001 |
| ARB | 21.1 (15/71) | 8.8 (7/80) | 0.031 | 12.6 (104/825) | 6.8 (54/790) | < 0.001 |
ACEI angiotensin-converting enzyme inhibitors, ARB angiotensin II receptor blockers, CABG coronary bypass artery grafting, LMCAD left main coronary artery disease, LVEF left ventricular ejection fraction, MI myocardial infarction, PCI percutaneous coronary intervention, PVD peripheral vascular disease, TIA transient ischemia attack, TSL total stent length, 3VD three-vessel disease
Outcomes according to COPD
When compared to those without COPD, patients with COPD had a comparable MACCE rate at 30 days (5.8% vs. 5.2%, HR: 1.12, 95% CI: 0.57–2.24, p = 0.738), but had a higher 5-year MACCE rate (41.4% vs. 32.1%, HR: 1.42, 95% CI: 1.09–1.85, p = 0.010), which was mainly driven by a higher 5-year all-cause death (23.2% vs. 12.2%, HR: 2.15, 95% CI: 1.49–3.10, p < 0.001) (Table 3). A significantly higher risk of all-cause death at 10 years was observed in the patients with COPD, compared with those without COPD (43.1% vs. 24.9%; HR: 2.03; 95% CI: 1.56–2.64; p < 0.001, Fig. 1a, Table 3). COPD was associated with a higher 10-year all-cause death in both PCI and CABG arms (Fig. 1b, c).
Table 3.
Risk of COPD on outcomes according to treatment strategies
| COPD | No COPD | Unadjusted HR (95% CI) | p value | |
|---|---|---|---|---|
| (n = 154) | (n = 1646) | |||
| At 30 days | ||||
| MACCE | 5.8 (9) | 5.2 (85) | 1.12 (0.57–2.24) | 0.738 |
| Death, stroke, MI | 5.8 (9) | 4.1 (67) | 1.43 (0.71–2.87) | 0.311 |
| All-cause death | 3.3 (5) | 1.2 (20) | 2.66 (1.00–7.09) | 0.050 |
| Cardiac death | 3.3 (5) | 1.2 (20) | 2.66 (1.00–7.09) | 0.050 |
| Any MI | 4.6 (7) | 2.9 (48) | 1.56 (0.71–3.45) | 0.272 |
| Any stroke | 0 (0) | 0.7 (12) | 0.04 (0–314.05) | 0.489 |
| Any repeat revascularization | 2.0 (3) | 2.3 (37) | 0.86 (0.27–2.8) | 0.806 |
| At 5 years | ||||
| MACCE | 41.4 (61) | 32.1 (500) | 1.42 (1.09–1.85) | 0.010 |
| Death, stroke, MI | 29.9 (44) | 18.3 (284) | 1.81 (1.32–2.49) | < 0.001 |
| All-cause death | 23.2 (34) | 12.2 (186) | 2.15 (1.49–3.10) | < 0.001 |
| Cardiac death | 13.8 (20) | 6.7 (102) | 2.27 (1.41–3.67) | 0.001 |
| Any MI | 10.0 (14) | 6.6 (102) | 1.56 (0.89–2.73) | 0.119 |
| Any stroke | 4.4 (6) | 2.9 (45) | 1.53 (0.65–3.58) | 0.329 |
| Any repeat revascularization | 22.1 (29) | 20.2 (303) | 1.11 (0.76–1.63) | 0.583 |
| At 10 years | ||||
| All-cause death | 43.1 (64) | 24.9 (396) | 2.03 (1.56–2.64) | < 0.001 |
COPD chronic obstructive pulmonary disease, MI myocardial infarction, MACCE major adverse cardiovascular and cerebrovascular event. Data are presented as percentage based on Kaplan–Meier estimates (number of deaths)
Fig. 1.
Kaplan–Meier curves for all-cause death at 10 years in patients with (red) or without (blue) COPD among the overall cohort, the PCI arm and the CABG arm. a 10-year all-cause mortality according to COPD in the overall cohort. b 10-year all-cause mortality according to COPD in the PCI arm. c 10-year all-cause mortality according to COPD in the CABG arm. Event rates represent Kaplan–Meier estimates
Clinical outcomes according to revascularization strategy
There were 71 and 83 COPD patients randomized to PCI and CABG, respectively. Among these patients, differences between CABG and PCI for 30-day MACCE (4.8% vs. 7.0%, HR: 0.66, 95% CI: 0.18–2.46, p = 0.538) and 5-year MACCE (35.9% vs. 47.3%, HR: 0.73, 95% CI: 0.44–1.2, p = 0.213) were not statistically significant (Table 4). At 10 years, CABG appeared to have a slightly lower risk of all-cause death compared with PCI (42.3% vs. 43.9%; HR: 0.96, 95% CI: 0.59–1.56, p = 0.858, Fig. 2a, Table 4) in patients with COPD. By contrast, among those without COPD, CABG had a significantly lower risk of 10-year all-cause death (22.7% vs. 27.1%; HR: 0.81, 95% CI: 0.67–0.99, p = 0.041, Fig. 2b, Table 4). There was no significant differential treatment effect of CABG versus PCI on the 10-year all-cause death for patients without COPD and patients with COPD (p interaction = 0.544, Table 4).
Table 4.
Treatment effect on outcomes in COPD and non-COPD patients
| COPD (N = 154) | p value | No COPD (N = 1646) | p value | p interaction | |||||
|---|---|---|---|---|---|---|---|---|---|
| CABG (N = 83) | PCI (N = 71) | HR (95% CI) | CABG (N = 814) | PCI (N = 832) | HR (95% CI) | ||||
| At 30 days | |||||||||
| MACCE | 4.8 (4) | 7.0 (5) | 0.66 (0.18–2.46) | 0.538 | 4.6 (37) | 5.8 (48) | 0.79 (0.51–1.21) | 0.282 | 0.798 |
| All-cause death, stroke, MI | 4.8 (4) | 7.0 (5) | 0.66 (0.18–2.46) | 0.538 | 3.7 (30) | 4.5 (37) | 0.83 (0.52–1.35) | 0.460 | 0.745 |
| All-cause death | 2.4 (2) | 4.2 (3) | 0.56 (0.09–3.34) | 0.523 | 0.5 (4) | 1.9 (16) | 0.26 (0.09–0.77) | 0.015 | 0.466 |
| Cardiac death | 2.4 (2) | 4.2 (3) | 0.56 (0.09–3.34) | 0.523 | 0.5 (4) | 1.9 (16) | 0.26 (0.09–0.77) | 0.015 | 0.466 |
| Any MI | 3.6 (3) | 5.7 (4) | 0.62 (0.14–2.78) | 0.534 | 2.2 (18) | 3.6 (30) | 0.61 (0.34–1.1) | 0.102 | 0.994 |
| Any stroke | 0 (0) | 0 (0) | 0 (0–0) | 1.4 (11) | 0.1 (1) | 11.35 (1.47–87.95) | 0.020 | 0.998 | |
| Any repeat revascularization | 1.2 (1) | 2.8 (2) | 0.42 (0.04–4.63) | 0.478 | 1.4 (11) | 3.1 (26) | 0.43 (0.21–0.87) | 0.020 | 0.977 |
| At 5 years | |||||||||
| MACCE | 35.9 (28) | 47.3 (33) | 0.73 (0.44–1.2) | 0.213 | 27.1 (201) | 36.8 (299) | 0.67 (0.56–0.8) | < 0.001 | 0.805 |
| All-cause death, stroke, MI | 28.3 (22) | 31.5 (22) | 0.9 (0.5–1.63) | 0.729 | 16.6 (121) | 19.9 (163) | 0.78 (0.62–0.99) | 0.038 | 0.677 |
| All-cause death | 23.3 (18) | 23.1 (16) | 1.01 (0.52–1.99) | 0.969 | 11.2 (79) | 13.1 (107) | 0.78 (0.58–1.04) | 0.092 | 0.475 |
| Cardiac death | 11.7 (9) | 16.1 (11) | 0.73 (0.3–1.76) | 0.483 | 5.0 (35) | 8.4 (67) | 0.55 (0.37–0.83) | 0.004 | 0.563 |
| Any MI | 4.9 (4) | 15.3 (10) | 0.35 (0.11–1.11) | 0.073 | 3.7 (29) | 9.2 (73) | 0.41 (0.27–0.63) | < 0.001 | 0.782 |
| Any stroke | 5.6 (4) | 3.1 (2) | 1.84 (0.34–10.04) | 0.482 | 3.6 (27) | 2.3 (18) | 1.6 (0.88–2.9) | 0.125 | 0.888 |
| Any repeat revascularization | 12.9 (9) | 31.9 (20) | 0.38 (0.17–0.84) | 0.016 | 13.8 (101) | 26.3 (202) | 0.49 (0.39–0.63) | < 0.001 | 0.532 |
| At 10 years | |||||||||
| All-cause death | 42.3 (34) | 43.9 (30) | 0.96 (0.59–1.56) | 0.858 | 22.7 (178) | 27.1 (218) | 0.81 (0.67–0.99) | 0.041 | 0.554 |
COPD chronic obstructive pulmonary disease, MI myocardial infarction, MACCE major adverse cardiovascular and cerebrovascular event. Data are presented as percentage based on Kaplan–Meier estimates (number of deaths)
Fig. 2.
Kaplan–Meier curves for all-cause death at 10 years in patients randomized to PCI (blue) vs. CABG (red) among patients with and without COPD. a All-cause mortality at 10 years in patients with COPD. b All-cause mortality at 10 years in patients without COPD. Event rates represent Kaplan–Meier estimates
Multivariable analysis
After adjustment for the baseline confounders, COPD remained an independent predictor of all-cause death at 10 years in the CABG arm (adjusted HR: 2.10, 95% CI: 1.19–3.69, p = 0.010), but was not an independent predictor in the PCI arm (adjusted HR: 1.19, 95% CI: 0.69–2.06, p = 0.536) (Table 5).
Table 5.
The association between COPD and 10-year all-cause mortality
| Overall population | PCI arm | CABG arm | ||||
|---|---|---|---|---|---|---|
| Adjusted HR (95% CI) |
p | Adjusted HR (95% CI) |
p | Adjusted HR (95% CI) |
p | |
| PVD | 2.33 (1.71–3.17) | < 0.001 | 2.61 (1.64–4.16) | < 0.001 | 2.28 (1.48–3.51) | < 0.001 |
| Current smoking | 2.17 (1.59–2.97) | < 0.001 | 2.44 (1.60–3.73) | < 0.001 | 2.05 (1.28–3.30) | 0.003 |
| Age (per 10 years increase) | 2.02 (1.67–2.43) | < 0.001 | 1.65 (1.29–2.11) | < 0.001 | 2.72 (2.01–3.69) | < 0.001 |
| Previous stroke | 1.72 (1.05–2.83) | 0.033 | 1.20 (0.55–2.59) | 0.645 | 2.33 (1.19–4.57) | 0.014 |
| Pharmacologically-treated diabetes | 1.63 (1.25–2.12) | < 0.001 | 1.66 (1.16–2.38) | 0.006 | 1.68 (1.14–2.49) | 0.010 |
| COPD | 1.50 (1.01–2.20) | 0.042 | 1.19 (0.69–2.06) | 0.536 | 2.10 (1.19–3.69) | 0.010 |
| LVEF (per 10% decrease) | 1.14 (1.03–1.25) | 0.011 | 1.18 (1.02–1.33) | 0.020 | 1.11 (0.96–1.28) | 0.165 |
| Previous MI | 1.12 (0.86–1.47) | 0.403 | 1.10 (0.76–1.59) | 0.619 | 1.05 (0.69–1.61) | 0.812 |
| Anatomical SYNTAX score (per 10 point increase) | 1.10 (0.99–1.21) | 0.076 | 1.18 (1.03–1.35) | 0.014 | 0.99 (0.84–1.16) | 0.887 |
| Female | 1.04 (0.78–1.38) | 0.795 | 1.07 (0.73–1.57) | 0.740 | 0.97 (0.63–1.49) | 0.882 |
| Creatinine clearance (per 10 ml/min decrease) | 1.03 (0.97–1.10) | 0.273 | 1.09 (1.00–1.18) | 0.055 | 0.97 (0.88–1.08) | 0.567 |
| Body mass index (per unit increase) | 1.02 (0.99–1.05) | 0.275 | 1.02 (0.98–1.06) | 0.365 | 1.00 (0.95–1.05) | 0.964 |
COPD chronic obstructive pulmonary disease, LVEF left ventricular ejection fraction, MI myocardial infarction, PVD peripheral vascular disease
Discussion
To our knowledge, our study is the first analysis to evaluate the treatment effect of CABG versus PCI on 10-year all-cause mortality according to COPD in patients with 3VD and/or LMCAD. The main findings of the present study are summarized as follows:
No significant difference was found between COPD and non-COPD patients for 30-day MACCE. However, COPD was associated with a significantly increased risk of 5-year and 10-year all-cause death.
The relative treatment effects of CABG versus PCI on 10-year all-cause death were not significantly different for patients with COPD and patients without COPD.
COPD was an independent predictor of 10-year all-cause death after CABG but not after PCI.
The impact of COPD on mortality after revascularization
COPD has been identified as a risk factor for worse clinical outcomes in CAD patients [3, 25]. However, the literature is inconsistent regarding the impact of COPD on mortality after revascularization. Angouras et al. found that COPD was not an independent predictor of increased early mortality, but was a continuing detrimental risk factor for long-term survival (mean follow-up, 7.6 years) in patients who underwent isolated CABG [26]. Analysis from SWEDEHEART registry demonstrated that patients with COPD had a significantly higher rate of both 30-day and 5-year mortality after CABG [15]. In patients who underwent PCI, previous reports showed discrepant results regarding the impact of COPD on short-term outcomes. Selvaraj et al. found that COPD was a significant independent predictor of in-hospital death and long-term mortality after PCI [16], while Berger et al. reported that in-hospital major adverse cardiac outcomes were not different between COPD and non-COPD groups. However, at 3-year follow-up, mortality for patients with COPD was significantly higher compared to those without COPD (21% vs. 9%, p < 0.001). The investigators found that COPD was independently associated with a twofold increase in the hazard of long-term mortality [27]. In our analysis, we observed that at 30 days patients with COPD had a comparable MACCE rate and a trend for a higher all-cause death (3.3% vs. 1.2%, HR: 2.66, 95% CI: 1.00–7.09, p = 0.050, Table 3). In terms of long-term survival, we found that COPD was associated with a significantly increased risk of 5-year and 10-year all-cause mortality both in the CABG arm and in the PCI arm. Our findings are consistent with previous studies reporting COPD is associated with a high risk of long-term mortality after revascularization [26, 27].
The explanations for these inconsistent results with respect to short-term mortality may be multifactorial. Varied definitions for COPD and different enrolled populations in these studies may partly contribute to the inconsistency. In addition, some studies have demonstrated that operative mortality after CABG is associated with the severity of COPD. A smaller study that evaluated the impact of COPD on CABG outcome found that only severe COPD influenced hospital deaths, so that hospital mortality in patients with mild-to-moderate COPD undergoing CABG was similar to those without COPD [28]. Subsequently, Fuster et al. found that in-hospital mortality was directly related to the severity of lung disease. Specifically, patients with forced expiratory volume in the first second (FEV1) < 60% predicted had higher mortality than those with FEV1 > 60%, and that this should be considered as a primary prognostic factor in COPD patients undergoing CABG procedures [29]. Moreover, restrictive lung disease may carry a greater prognostic impact than obstructive [11]. However, there are again inconsistent data. Michalopoulos et al. reported that patients with a history of mild or moderate COPD undergoing elective CABG had morbidity and mortality rates comparable to those without COPD [30]. Manganas et al. reported that the mortality rate associated with CABG is not affected by the presence and severity of airflow obstruction in patients with COPD, although the incidence of pulmonary infections and length of hospital stay were increased in patients with severe COPD [12]. Further studies are required to determine the impact of COPD on short-term outcomes.
Is there an optimal revascularization strategy for patients with COPD?
To date, limited data exist in terms of the optimal revascularization strategy for patients with COPD and complex CAD. To our knowledge, our study is the first analysis to evaluate the treatment effect of CABG versus PCI on 10-year all-cause mortality according to COPD in patients with 3VD and/or LMCAD. In the EXCEL trial, patients with COPD had a trend for a higher all-cause death at 30 days (3.0% vs. 0.9%, p = 0.06) compared to those without COPD [18], which is similar to our findings. With regard to long-term outcomes, a higher 3-year mortality was observed in patients with COPD. Furthermore, in the EXCEL trial there were no statistically significant interactions in the relative risks of PCI versus CABG for the primary composite endpoint (death, stroke, MI or ischemia-driven revascularization) in patients with and without COPD at 3 years [18]. These findings are consistent with our current analysis, in which COPD was associated with a higher 10-year all-cause death, and no significant interaction between COPD and treatment strategy (CABG versus PCI) was found for all-cause death at 10 years. Although patients with COPD represent an increased surgical risk, patients with severe COPD have an acceptable long-term survival [11] compared to PCI and should therefore not be routinely denied CABG. More importantly, LIMA utilization in patients with COPD results in a significantly increased long-term survival, without an increased intensive care unit stay, re-intubation rate or in-hospital mortality rate [11]. Moreover, Ovaliet et al. found similar morbidity and mortality rates among the patients with and without COPD who underwent off-pump CABG [31]. Based on this evidence, CABG should be considered as an alternative revascularization strategy for patients with COPD. However, further large-scale studies are needed.
COPD was an independent predictor of 10-year all-cause mortality after CABG but not after PCI
Previous studies had demonstrated that COPD was a predictor of long-term mortality after CABG [10]. A single-center analysis with a total of 10,994 patients found that COPD was a significant independent predictor of in-hospital death and long-term mortality after PCI [16], whereas another study reported that COPD was not an independent predictor of major adverse clinical outcomes in patients with STEMI following PCI [32]. In the SYNTAX trial, COPD was independently associated with 4-year mortality after CABG but not after PCI [4, 33]. Similarly, in SYNTAXES, with a follow-up out to 10 years, we found COPD was an independent predictor in the CABG arm but not in the PCI arm in the SYNTAXES. Therefore, COPD remains as one of the prognostic indexes in the SYNTAX score II 2020 [9]. COPD was a significant risk factor for non-adherence to medications, such as beta blockers, and underutilization of beta blockers in COPD was associated with clinicians concerns about bronchoconstriction [34]. In the SYNTAX study, patients with COPD were less likely to receive aspirin and beta blockers at discharge. However, after adjustment for the prescriptions of aspirin and beta blockers at discharge, COPD remains an independent predictor of 10-year all-cause death (HR: 1.52, 95% CI: 1.03–2.24, p = 0.037 in overall population, HR: 2.19, 95% CI: 1.24–3.89, p = 0.007 in CABG arm). Patients with COPD represent a high-risk cohort where adherence to treatment guidelines is crucial. Clinicians should take particular care with respect to the use of beta blockers and aspirin in patients with COPD, since prior studies demonstrated that both beta blockers and aspirin are not only safe but could also reduce all-cause death in patients with COPD [35, 36]. The majority of the studies in the field demonstrated that patients with a history of COPD have higher mortality rates than those without COPD, either after PCI or CABG. Therefore, in clinical practice, we should pay more attention to patients with COPD and use multidisciplinary care and self-management [37], a double health care approach that might improve the outcomes post revascularization no matter what modality of revascularization is used.
Limitations
Several limitations should be considered in our current study. First, due to the modest sample size, the present analyses might not have adequate statistical power. Further large-scale trials more specifically dedicated to COPD patients are warranted. Second, this is a post hoc analysis and should be interpreted as hypothesis-generating only [38]. Third, the SYNTAX trial enrolled patients with de novo 3VD and/or LMCAD, and the findings should not be extrapolated to other CAD patients. COPD at baseline was defined according to the definition in EuroSCORE which is not specific for COPD; that definition does not differentiate asthma from COPD patients. However, it has been demonstrated in prior studies that asthma, as comorbidity, is independently associated with ischemic heart disease to an extent similar as COPD [39]. Another major limitation is that in the SYNTAXES study, the severity of COPD, emphysema, GOLD groups or grades, COPD exacerbations, pulmonary function tests (such as FEV1), and the use of long-term oxygen therapy or noninvasive ventilation were not available. Moreover, the endpoint in the SYNTAXES study was solely 10-year all-cause death. However, the SYNTAXES study provided data from the first randomized trial, comparing surgery and PCI with drug eluting stent, for which 10-year vital status was available in 93.8% of the patients. It has to be acknowledged that the PCI patients were treated with a first-generation drug eluting stent, which is no longer commercially available. Nevertheless, it is inevitable that any long-term observational data will be derived from a population treated with outdated/obsolete technology, while the evidence provided by contemporary technology can be derived only from short-term follow-up studies. Finally, an inherent bias may exist that patients with severe COPD who were deemed extremely high risk for CABG may not have been included in the randomized cohort and directed to the PCI registry in the SYNTAX trial.
Conclusions
In the SYNTAXES trial, COPD was associated with a higher risk of 10-year all-cause death in patients with 3VD and/or LMCAD following either PCI or CABG. The risk of all-cause death at 10 years in patients with CABG versus PCI was similar irrespective of the prevalence of COPD.
Funding
The SYNTAX Extended Survival study was supported by the German Foundation of Heart Research (Frankfurt am Main, Germany). The SYNTAX trial, during 0–5 year follow-up, was funded by Boston Scientific Corporation (Marlborough, MA, USA). Both sponsors had no role in the study design, data collection, data analyses and interpretation of the study data, nor were involved in the decision to publish the final manuscript. The principal investigators and authors had complete scientific freedom.
Declarations
Conflict of interest
Dr. Serruys reports personal fees from Biosensors, Micel Technologies, Sinomedical Sciences Technology, Philips/Volcano, Xeltis, and HeartFlow, outside the submitted work. Dr. van Geuns reports personal fees from Abbott vascular, grants and personal fees from AstraZeneca, grants and personal fees from Amgen, grants and personal fees from Boston Scientific, personal fees from Sanofi, outside the submitted work. Dr. Morice reports to work as the CEO of CERC, a CRO which was never involved in the SYNTAX trial at any level, except that submitted the 10 years additional follow-up (for free) to French authorities to get approval. Dr. Morice also reports to work as minor shareholder of electroducer. Dr. Burzotta reports speaker’s fees from Abiomed, Abbott and Medtronic. Dr. Kappetein reports to work as an employee of Medtronic, outside the submitted work. Dr. James’s institution has received research grants from Boston Sc, Abbot, Biotronik, Medtronic, Astra Zeneca, Bayer, Jansen, The MedCo, and has received lecture fees from Biotronik, Astra Zeneca. All other authors have no disclosures.
References
- 1.Rabe KF, Hurst JR, Suissa S. Cardiovascular disease and COPD: dangerous liaisons? Eur Respir Rev. 2018 doi: 10.1183/16000617.0057-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andre S, Conde B, Fragoso E, et al. COPD and cardiovascular disease. Pulmonology. 2019;25(3):168–176. doi: 10.1016/j.pulmoe.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 3.Sin DD, Man SF. Chronic obstructive pulmonary disease as a risk factor for cardiovascular morbidity and mortality. Proc Am Thorac Soc. 2005;2(1):8–11. doi: 10.1513/pats.200404-032MS. [DOI] [PubMed] [Google Scholar]
- 4.Farooq V, van Klaveren D, Steyerberg EW, et al. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet. 2013;381(9867):639–650. doi: 10.1016/s0140-6736(13)60108-7. [DOI] [PubMed] [Google Scholar]
- 5.Serruys PWCP, Modolo R, et al. The SYNTAX score on its way out or … towards artificial intelligence: part I. EuroIntervention. 2020;16(1):44–59. doi: 10.4244/EIJ-D-17-00355. [DOI] [PubMed] [Google Scholar]
- 6.Serruys PWCP, Modolo R, et al. The SYNTAX score on its way out or … towards artificial intelligence: part II. EuroIntervention. 2020;16(5):60–75. doi: 10.4244/EIJ-D-19-00543B. [DOI] [PubMed] [Google Scholar]
- 7.Shahian DM, O'Brien SM, Filardo G, et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 1–coronary artery bypass grafting surgery. Ann Thorac Surg. 2009;88(1 Suppl):S2–22. doi: 10.1016/j.athoracsur.2009.05.053. [DOI] [PubMed] [Google Scholar]
- 8.Nashef SA, Roques F, Sharples LD, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41(4):734–44; discussion 44-5. doi: 10.1093/ejcts/ezs043. [DOI] [PubMed] [Google Scholar]
- 9.Takahashi K, Serruys PW, Fuster V, et al. Redevelopment and validation of the SYNTAX score II to individualise decision making between percutaneous and surgical revascularisation in patients with complex coronary artery disease: secondary analysis of the multicentre randomised controlled SYNTAXES trial with external cohort validation. Lancet. 2020;396(10260):1399–1412. doi: 10.1016/s0140-6736(20)32114-0. [DOI] [PubMed] [Google Scholar]
- 10.Leavitt BJ, Ross CS, Spence B, et al. Long-term survival of patients with chronic obstructive pulmonary disease undergoing coronary artery bypass surgery. Circulation. 2006;114(1 Suppl):I430–I434. doi: 10.1161/CIRCULATIONAHA.105.000943. [DOI] [PubMed] [Google Scholar]
- 11.O'Boyle F, Mediratta N, Chalmers J, et al. Long-term survival of patients with pulmonary disease undergoing coronary artery bypass surgery. Eur J Cardiothorac Surg. 2013;43(4):697–703. doi: 10.1093/ejcts/ezs454. [DOI] [PubMed] [Google Scholar]
- 12.Manganas H, Yves L, Bourgeois S, Perron J, Dagenais F, Maltais F. Postoperative outcome after coronary artery bypass grafting in chronic obstructive pulmonary disease. Can Respir J. 2007;14(1):19–24. doi: 10.1155/2007/378963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhao H, Li L, Yang G, et al. Postoperative outcomes of patients with chronic obstructive pulmonary disease undergoing coronary artery bypass grafting surgery: a meta-analysis. Medicine (Baltimore) 2019;98(6):e14388. doi: 10.1097/MD.0000000000014388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bundhun PK, Gupta C, Xu GM. Major adverse cardiac events and mortality in chronic obstructive pulmonary disease following percutaneous coronary intervention: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2017;17(1):191. doi: 10.1186/s12872-017-0622-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Andell P, Sjogren J, Batra G, Szummer K, Koul S. Outcome of patients with chronic obstructive pulmonary disease and severe coronary artery disease who had a coronary artery bypass graft or a percutaneous coronary intervention. Eur J Cardiothorac Surg. 2017;52(5):930–936. doi: 10.1093/ejcts/ezx219. [DOI] [PubMed] [Google Scholar]
- 16.Selvaraj CL, Gurm HS, Gupta R, Ellis SG, Bhatt DL. Chronic obstructive pulmonary disease as a predictor of mortality in patients undergoing percutaneous coronary intervention. Am J Cardiol. 2005;96(6):756–759. doi: 10.1016/j.amjcard.2005.05.016. [DOI] [PubMed] [Google Scholar]
- 17.Tomaniak M, Chichareon P, Takahashi K, et al. Impact of chronic obstructive pulmonary disease and dyspnoea on clinical outcomes in ticagrelor treated patients undergoing percutaneous coronary intervention in the randomized GLOBAL LEADERS trial. Eur Heart J Cardiovasc Pharmacother. 2019 doi: 10.1093/ehjcvp/pvz052. [DOI] [PubMed] [Google Scholar]
- 18.Huang X, Redfors B, Chen S, et al. Impact of chronic obstructive pulmonary disease on prognosis after percutaneous coronary intervention and bypass surgery for left main coronary artery disease: an analysis from the EXCEL trial. Eur J Cardiothorac Surg. 2019;55(6):1144–1151. doi: 10.1093/ejcts/ezy438. [DOI] [PubMed] [Google Scholar]
- 19.Thuijs DJFM, Kappetein AP, Serruys PW, et al. Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicentre randomised controlled SYNTAX trial. Lancet. 2019;394(10206):1325–1334. doi: 10.1016/s0140-6736(19)31997-x. [DOI] [PubMed] [Google Scholar]
- 20.Ong AT, Serruys PW, Mohr FW, et al. The SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) study: design, rationale, and run-in phase. Am Heart J. 2006;151(6):1194–1204. doi: 10.1016/j.ahj.2005.07.017. [DOI] [PubMed] [Google Scholar]
- 21.Serruys PWMM, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Stahle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW, Investigators S. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961–972. doi: 10.1056/NEJMoa0804626. [DOI] [PubMed] [Google Scholar]
- 22.Mohr FW, Morice M-C, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet. 2013;381(9867):629–638. doi: 10.1016/s0140-6736(13)60141-5. [DOI] [PubMed] [Google Scholar]
- 23.Nashef SARF, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE) Eur J Cardiothorac Surg. 1999;16:9–13. doi: 10.1016/S1010-7940(99)00134-7. [DOI] [PubMed] [Google Scholar]
- 24.Pocock SJ, McMurray JJV, Collier TJ. Statistical controversies in reporting of clinical trials: Part 2 of a 4-part series on statistics for clinical trials. J Am Coll Cardiol. 2015;66(23):2648–2662. doi: 10.1016/j.jacc.2015.10.023. [DOI] [PubMed] [Google Scholar]
- 25.Sin DD, Man SF. Why are patients with chronic obstructive pulmonary disease at increased risk of cardiovascular diseases? The potential role of systemic inflammation in chronic obstructive pulmonary disease. Circulation. 2003;107(11):1514–1519. doi: 10.1161/01.cir.0000056767.69054.b3. [DOI] [PubMed] [Google Scholar]
- 26.Angouras DC, Anagnostopoulos CE, Chamogeorgakis TP, et al. Postoperative and long-term outcome of patients with chronic obstructive pulmonary disease undergoing coronary artery bypass grafting. Ann Thorac Surg. 2010;89(4):1112–1118. doi: 10.1016/j.athoracsur.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 27.Berger JS, Sanborn TA, Sherman W, Brown DL. Effect of chronic obstructive pulmonary disease on survival of patients with coronary heart disease having percutaneous coronary intervention. Am J Cardiol. 2004;94(5):649–651. doi: 10.1016/j.amjcard.2004.05.034. [DOI] [PubMed] [Google Scholar]
- 28.Samuels LE, Kaufman MS, Morris RJ, Promisloff R, Brockman SK. Coronary artery bypass grafting in patients with COPD. Chest. 1998;113(4):878–882. doi: 10.1378/chest.113.4.878. [DOI] [PubMed] [Google Scholar]
- 29.Fuster RG, Argudo JA, Albarova OG, et al. Prognostic value of chronic obstructive pulmonary disease in coronary artery bypass grafting. Eur J Cardiothorac Surg. 2006;29(2):202–209. doi: 10.1016/j.ejcts.2005.11.015. [DOI] [PubMed] [Google Scholar]
- 30.Michalopoulos A, Geroulanos S, Papadimitriou L, et al. Mild or moderate chronic obstructive pulmonary disease risk in elective coronary artery bypass grafting surgery. World J Surg. 2001;25(12):1507–1511. doi: 10.1007/s00268-001-0161-x. [DOI] [PubMed] [Google Scholar]
- 31.Ovali C, Sahin A. Chronic obstructive pulmonary disease and off-pump coronary surgery. Ann Thorac Cardiovasc Surg. 2018;24(4):193–199. doi: 10.5761/atcs.oa.17-00231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sung PH, Chung SY, Sun CK, et al. Impact of chronic obstructive pulmonary disease on patient with acute myocardial infarction undergoing primary percutaneous coronary intervention. Biomed J. 2013;36(6):274–281. doi: 10.4103/2319-4170.113373. [DOI] [PubMed] [Google Scholar]
- 33.Farooq V, Serruys PW, Bourantas C, et al. Incidence and multivariable correlates of long-term mortality in patients treated with surgical or percutaneous revascularization in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial. Eur Heart J. 2012;33(24):3105–3113. doi: 10.1093/eurheartj/ehs367. [DOI] [PubMed] [Google Scholar]
- 34.Rasmussen DB, Bodtger U, Lamberts M, et al. Beta-blocker, aspirin, and statin usage after first-time myocardial infarction in patients with chronic obstructive pulmonary disease: a nationwide analysis from 1995 to 2015 in Denmark. Eur Heart J Qual Care Clin Outcomes. 2020;6(1):23–31. doi: 10.1093/ehjqcco/qcy063. [DOI] [PubMed] [Google Scholar]
- 35.Yang YL, Xiang ZJ, Yang JH, Wang WJ, Xu ZC, Xiang RL. Association of beta-blocker use with survival and pulmonary function in patients with chronic obstructive pulmonary and cardiovascular disease: a systematic review and meta-analysis. Eur Heart J. 2020;41(46):4415–4422. doi: 10.1093/eurheartj/ehaa793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goto T, Faridi MK, Camargo CA, Hasegawa K. The association of aspirin use with severity of acute exacerbation of chronic obstructive pulmonary disease: a retrospective cohort study. NPJ Prim Care Respir Med. 2018;28(1):7. doi: 10.1038/s41533-018-0074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marlies Zwerink MBK, van der Valk PDLPM, Zielhuis GA, Monninkhof EM, van der Palen J, Frith PA, Effing T. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014;3:CD002990. doi: 10.1002/14651858.CD002990.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Milojevic M, Nikolic A, Juni P, Head SJ. A statistical primer on subgroup analyses. Interact Cardiovasc Thorac Surg. 2020 doi: 10.1093/icvts/ivaa042. [DOI] [PubMed] [Google Scholar]
- 39.Carter P, Lagan J, Fortune C, et al. Association of cardiovascular disease with respiratory disease. J Am Coll Cardiol. 2019;73(17):2166–2177. doi: 10.1016/j.jacc.2018.11.063. [DOI] [PubMed] [Google Scholar]