Abstract
Exposure to alcohol misuse is considered an adverse childhood experience impacting on neurodevelopmental and behavioural outcomes in adolescents including substance use, mental illness, problem behaviours, suicidality, and teenage pregnancy. Most research on this issue has focussed on higher income countries, whereas patterns of alcohol use and related factors may be different in low- and middle-income countries (LMICs). This systematic review therefore seeks to collate all published studies from 1990–2020 on the topic set in LMICs. 43 studies were included, totalling 70,609 participants from 18 LMICs. Outcomes assessed included: substance use; depression/anxiety; suicidal ideation; problem behaviour; emotional dysfunction; teenage pregnancy; and self-harm. Despite heterogeneity in the studies identified, this review documented some association between exposure to household alcohol misuse and adverse adolescent outcomes in LMICs, including mental health problems, problem behaviours, and suicidality. The mechanisms leading to these outcomes are likely varied, and further research in different socio-economic and cultural contexts, particularly in the form of longitudinal studies, is called for.
Electronic supplementary material
The online version of this article (10.1007/s10578-020-01038-w) contains supplementary material, which is available to authorized users.
Keywords: Alcohol, Adolescent, Behaviour, Low- and middle-income countries
Introduction
Experiences in childhood and adolescence have been shown to have a significant impact on health in later life, primarily based on research from high income countries (HICs) [1, 2]. This might be through exposure to social and environmental factors directly leading to the development of particular diseases, or more indirectly, with childhood experiences shaping attitudes and future health behaviours. Some of these consequences become apparent relatively quickly, others develop much later in adult life. Of particular interest are those that become prominent during adolescence, as this has been identified as a stage when many enduring health problems (including mental and physical health as well as risky behaviours) first emerge [3, 4].
Adverse childhood experiences (ACEs), including parental or caregiver substance abuse, mental illness, conflict, neglect, or abuse, have been particularly associated with harmful adolescent neurodevelopmental and behavioural outcomes [5]. Children living in families where they are exposed to alcohol misuse by a caregiver have been described as having an increased likelihood of adverse experiences including abuse or neglect [6]. The negative association between maternal alcohol exposure in utero and development is well known; exposure can cause foetal alcohol spectrum disorders which include developmental and later mental health problems [7, 8], but the impact of indirect alcohol exposure via caregivers and negative adolescent outcomes has been comparatively less well described, particularly in low and middle income countries (LMICs). Harmful or problem drinking by parents, caregivers, or others in the household can disrupt family relationships, place adolescents under chronic stress, and lead to injury, abuse and neglect [1]. Associated consequences in terms of adolescent health can include suicidality, mental illness, substance use, teenage pregnancy, and a range of problem behaviours such as absence from school and internet addiction.
Comparatively little work has been done to investigate how household alcohol misuse impacts adolescents in the household in LMICs specifically. This demands attention, as patterns of alcohol use and misuse, household structure and dynamics, and childhood experiences vary considerably by country and culture [9]. Family units tend to be more cohesive in LMICs than in high-income countries, with large households and several generations under one roof, increasing the potential for exposure to alcohol misuse in the home from a large number of family members [10], especially in the presence of household crowding which is known to exacerbate mental health outcomes including alcohol abuse [11]. The multigenerational aspect could also conceivably be protective. Therefore, we aim to review and synthesise the results of studies from LMICs, in the hope that findings can inform policy recommendations and directions for future research.
Studies on childhood indirect exposure to alcohol misuse in the home have tended to report neurodevelopmental outcomes, whereas those on adolescents focus more on behavioural outcomes. Mechanisms through which associations might arise vary significantly between these two age groups and types of outcomes; therefore to maintain focus it makes sense for adolescents to be studied as an individual group [12]. The following review therefore reports specifically on adolescent behavioural outcomes, given that the relative balance between the rapid increase in the development of executive function and simultaneously an increase in impulsivity and independence may result in the opportunities for certain risky behaviours to occur [13]. A separate review completed in parallel to this one reports on the studies relevant to child neurodevelopmental outcomes [14].
Our aims are as follows:
To identify studies of the impact of excess alcohol consumption among household adults on adolescent developmental health outcomes (neurodevelopmental, cognitive and behavioural) in low- and middle-income countries and to evaluate the quality of the research
To explore whether the nature of alcohol use and misuse differs by individual family members (father, mother or other family member) in its impact on adolescent health outcomes (including neurodevelopment, cognitive and behavioural impact) in low- and middle-income countries
Methods
A protocol for this review was published on the PROSPERO register in June 2017, registration number CRD42017070209.
Eligibility Criteria
Studies were included in this review if they met the following criteria:
Participants: individuals aged 10–18 years
Exposure: household member engaging in alcohol misuse. ‘Household' included all relatives living in the household. 'Family' included parents and siblings
Setting: low- and middle-income countries as defined by the World Bank [15]
Outcome: Outcome measure of adverse adolescent behavioural and neurodevelopmental impacts (excludes outcomes directly related to alcohol exposure such as children’s own drinking behaviour as a result of adult alcohol exposure or in utero alcohol exposure)
Language: Studies published in English, or with translation available
Year: Published from 1990 or later
In order to be inclusive and avoid missing potentially relevant studies, a wide participant-eligible age range of 10–18 was used for this study [16]. Behavioural and neurodevelopmental changes of adolescence have been shown to begin with the onset of puberty, with hormonal changes associated with changes in neuronal development and cognitive function [17, 18]. Studies which only included a small minority of participants within this range were excluded. The lower limit of age 10 was selected in line with guidance from the WHO, who define adolescence as beginning at this age [19]. Age 10 is also the age at which most girls, who commence puberty prior to boys, have commenced puberty (defined by the onset of breast development) [20]. The upper limit of age 18 was selected as this is the legal age at which a subject is considered an adult in the majority of countries [21]. Studies which focused on antenatal, rather than household, alcohol exposure, were excluded due to confounding. Studies which described outcomes of abuse unconnected to characteristics of the child or adolescent were also not eligible.
The term ‘alcohol misuse’ i.e. harmful use (ICD-11 code F10.1) was understood as harmful in accordance with WHO guidelines, whether due to excessive volumes above recommended lower limits, or problematic patterns of drinking [22]. In order to ensure that no potentially relevant studies would be missed, the search term included ‘use’ to be deliberately broad and inclusive. Adolescents’ own use of alcohol was deliberately excluded as an outcome measure. This was partly because the relationship with household alcohol misuse has already been addressed in previous reviews [23, 24], and partly because this review sought to investigate more indirect impacts of alcohol misuse in the home. Adolescent drinking due to potential genetic elements, or due to easy availability of alcohol, was not of interest [25, 26].
Information Sources
Five electronic databases were searched from 1990 to April 2020: Medline, EMBASE, OVID Global Health, Cochrane Library and PsychInfo. An original June 2017 search was updated in June 2018 and in April 2020.
Search Strategy
The search strategy was structured as follows: “alcohol use” AND “household” AND “young person” AND “neurodevelopmental outcome(s)” with associated synonyms. Each category contained a range of terms. The full search strings used for MEDLINE are available in Supplementary File 1.
The results were then filtered using the Cochrane LMIC filter, modelled on World Bank definitions, to return studies set in low and middle income countries (LMICs) [27]. This filter has been previously used in systematic reviews of similar nature [28–31]. During targeted abstract and full text review, further screening made use of the up to date World Bank list of LMICs [15].
Study Selection and Data Extraction
After the studies were downloaded, and the Cochrane LMIC filter had been applied, each title and abstract was reviewed by one reviewer and uncertainties checked by a second against the inclusion criteria. Shortlisted full-text articles were subsequently checked by two separate reviewers. This led to the population of the final list of studies to be included.
A standardised pre-piloted extraction form was developed, tested on 10 articles and revised iteratively as needed. Extracted information included:
Study characteristics: setting, study design, method of data-analysis;
Participants: study population, number of participants in each group, patient characteristics
Child or adolescent health outcome (as reflected in primary outcome)
Household adult alcohol exposure or definition (as reflected in secondary outcome)
Household location, income, food insecurity, asset index and family factors and other factors (if available)
Each study type was classified e.g. cohort, cross-sectional study, according to standard definitions [32]. Each study was also classified as relevant to adolescents, children, or both.
Results Synthesis
The evidence reviewed is presented as a narrative report due to the wide range of methodologies used, populations, and outcomes. It was an objective of this study to incorporate any reported behavioural outcomes. Consequently, there were no pre-specified outcome measures; rather, these were identified and categorised iteratively by the research team according to the outcomes reported in the eligible studies. The results for adolescents covered the following behavioural and mental health outcomes:
Substance use (other than alcohol)
Depression/anxiety and other psychiatric disorders
Emotional dysfunction
Problem behaviour
Suicidal ideation and behaviour
Teenage pregnancy
Self-harm (non-suicidal)
Quality Assurance
In our review, given the predominance of observational studies, the National Heart, Lung and Blood Institute (NHLBI) Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies was utilised, or the equivalent tool for Case–Control studies if applicable [33]. The former tool asks 14 questions with answers of ‘Yes’, ‘No’ or ‘Other’, such as ‘Was the exposure(s) assessed more than once over time?’ Two reviewers independently screened each study shortlisted for inclusion and awarded one point for each ‘yes’ answer, with additional arbitration by other team members where required, in order to reach an overall score. A maximum score of 14 (12 for Case–Control studies) was available for each paper, and a minimum score of 0, with higher scores indicating a high-quality paper relevant to our objectives. The scores were then used to produce an overall rating of ‘Good’, ‘Fair’ or ‘Poor’ relevant to the review, with studies rated as ‘Poor’ excluded from inclusion in the main results section.
Results
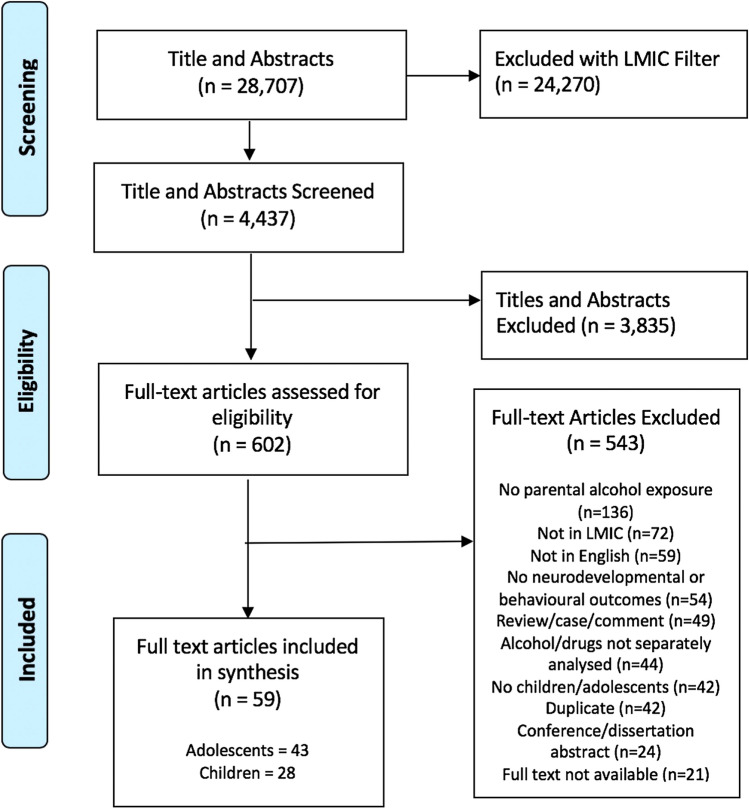
In total, 28,707 titles and abstracts were downloaded from the chosen databases. After filtering with the Cochrane LMIC filter [27], 4437 results were screened by title and abstract. 602 papers were subsequently selected for full text review. The process of study selection is illustrated in Fig. 1.
Fig. 1.
Study selection process
Study Characteristics
In total, 43 studies were included in this review of adolescents: 37 cross-sectional studies, 3 case–control studies, 2 cohort studies, and 1 mixed-methods study. Across the studies, 70,609 participants were included, from 18 different lower- and middle-income countries. The countries of origin of the included studies are reported in Table 1. Key characteristics are described in Table 2.
Table 1.
Countries of origin of included studies
| Country | Number of studies |
|---|---|
| India | 9 studies [36, 43, 48, 58–60, 64, 68, 74] |
| Turkey | 9 studies [39, 51–54, 56, 57, 67, 71] |
| Brazil | 6 studies [40, 46, 47, 49, 75, 85] |
| South Africa | 3 studies [35, 55, 66] |
| Kenya | 2 studies [65, 73] |
| Rwanda | 2 studies [37, 42] |
| Uganda | 2 studies [69, 72] |
| Thailand | 2 studies [41, 44] |
| Mexico | 1 study [34] |
| China | 1 study [70] |
| Ghana | 1 study [38] |
| Sri Lanka | 1 study [62] |
| Ukraine | 1 study [45] |
| Botswana | 1 study [50] |
| Morocco | 1 study [63] |
| Multi-country (Laos, Mongolia, Nepal, Sri Lanka) | 1 study [61] |
Table 2.
Summary of included studies
| Author | Country | Study type | Sample size | Population | Age range | Household alcohol exposure | Household location | Adolescent outcomes assessed | NHLBI Quality score | NHLBI Quality overall assessment |
|---|---|---|---|---|---|---|---|---|---|---|
| Andrade [46] | Brazil | Cross-sectional | 1231 | Public school students | 14–17 | Family | Urban | Substance use | 10 | Good |
| Betancourt [42] | Rwanda | Cross-sectional (as part of larger Case–control study) | 680 | Young people affected by and living with HIV | 11–17 | Family | Rural | Suicidal ideation/behaviour | 6 | Fair |
| Burlaka 2017 [45] | Ukraine | Cross-sectional | 251 | Mothers and children | 9–16 | Mother | Mixed | Emotional dysfunction | 9 | Good |
| Caputo and Bordin [40] | Brazil | Case–control | 408 | Sexually active teenage girls | 13–17 | Family | Urban | Teenage pregnancy | 9 | Good |
| Catani [62] | Sri Lanka | Cross-sectional | 296 | Young people attending school | 9–15 | Parents | Urban | Depression/anxiety and other psychiatric disorders | 7 | Fair |
| Chaudhury [37] | Rwanda | Mixed methods | 93 | Families affected by caregiver HIV | 7–17 | Caregiver | Rural | Depression/anxiety and other psychiatric disorders | 11 | Good |
| Ciftci Demirci [56] | Turkey | Cross-sectional | 1969 | Young people seeking treatment for substance use disorder | 11–20 | Parents | Urban | Substance use | 8 | Fair |
| da Rocha [85] | Brazil | Case–control study | 146 | Those with an IQ less than 70 referred to a special education institution | 7–19 | Relative/family | Urban | Cognitive delay/disorder | 6 | Fair |
| Evren [54] | Turkey | Cross-sectional | 4957 | 10th grade students in Istanbul | Mean 16.54 (SD 2.72) | Parents | Urban | Substance use | 7 | Fair |
| Faler [75] | Brazil | Case–control | 431 | Adolescent females | 14–16 | Parents | Urban | Teenage pregnancy | 8 | Fair |
| Francisco [34] | Mexico | Cross-sectional | 785 | Pregnant adolescents | 13–19 | Parents | Urban | Substance use; teenage pregnancy | 9 | Good |
| Gulati and Dutta [43] | India | Cross-sectional | 245 | Adolescents from families living in conditions of poverty | 12–16 | Parents | Rural | Emotional dysfunction | 8 | Fair |
| Guvendeger Doksat [71] | Turkey | Cross-sectional | 2518 | Young people admitted to psychiatric hospital | Mean 16* | Family | Urban | Suicidal ideation/behaviour; self-harm | 8 | Fair |
| Hamdulay and Mash [55] | South Africa | Cross-sectional | 438 | Students attending grade 8 and 11 classes | 14–17 | Household | Urban | Substance use | 7 | Fair |
| Jaisoorya 2018 [48] | India | Cross-sectional | 7560 | School Students | 12–19 | Family | Mixed | Emotional dysfunction | 10 | Good |
| Jogdand and Naik [68] | India | Cross-sectional | 600 | General | 6–18 | Caregiver | Urban | Problem behaviours | 7 | Fair |
| Karatay and Bas [67] | Turkey | Cross-sectional | 613 | High school students | Approx 14–18 (9th–12th grade) | Family | Urban | Emotional dysfunction | 8 | Fair |
| Khasakhala [73] | Kenya | Cross-sectional | 250 | Youth attending clinic with psychiatric or substance use disorder | 13–25 | Father | Urban | Suicidal ideation/behaviour | 7 | Fair |
| Khasakhala [65] | Kenya | Cross-sectional | 250 | Youth attending psychiatric clinic | 13–22 | Father | Urban | Depression/anxiety and other psychiatric disorders | 7 | Fair |
| Kheokao [41] | Thailand | Cross-sectional | 5184 | School students | 9–22 | Family | Not specified | Problem behaviours; cognitive delay/disorder | 8 | Fair |
| Lee 2019 [61] | Laos, Mongolia, Nepal, Sri Lanka | Cross-sectional | 4098 | High school students | Approx 12–17 (grade 7–11) | Parents | Urban | Depression/anxiety and other psychiatric disorders | 8 | Fair |
| Madruga [47] | Brazil | Cross-sectional | 761 | Secondary school children | 14–19 | Household | Mixed | Substance use | 8 | Fair |
| Mansharamani [58] | India | Cross-sectional | 100 | Outpatients and inpatients at a psychiatric ward of a tertiary facility | 4–14 | Parents | Mixed | Cognitive delay/disorder; depression/anxiety and other psychiatric disorders; emotional dysfunction | 6 | Fair |
| Meyer [44] | Thailand | Cross-sectional | 23 | Children/youth | 9–17 | Caregiver | Refugee camp | Problem behaviours; emotional dysfunction | 6 | Fair |
| Omkarappa and Rentala [59] | India | Cross-sectional | 200 | Secondary school students at government schools | 12–16 | Parents | Urban | Depression/anxiety and other psychiatric disorders; emotional dysfunction | 9 | Good |
| Ozcan and Ozcan [53] | Turkey | Cross-sectional | 4767 | Middle school and high school students | 10–18 | Parents | Urban | Substance use | 8 | Fair |
| Pillay and van der Veen [66] | South Africa | Cross-sectional | 100 | Children admitted to an inpatient psychiatric unit | 4–17 | Parents | Urban | Depression/anxiety and other psychiatric disorders | 6 | Fair |
| Praharaj [36] | India | Cross-sectional | 9 | Street children and adolescents abusing typewriter correction fluid | 10–17 | Father | Urban | Substance use | 5 | Poor |
| Rahi [60] | India | Cross-sectional | 620 | Slum children | 4–14 | Father | Urban | Depression/anxiety and other psychiatric disorders | 7 | Fair |
| Riva [50] | Botswana | Cross-sectional | 1936 | Students in public secondary schools | IQR 14–17 | Household | Urban | Substance use | 9 | Good |
| Singh [74] | India | Cross-sectional | 94 | Adolescents admitted after attempted suicide by ingestion | 15–18 | Parents | Urban | Suicidal ideation/behaviour | 6 | Fair |
| Singh [64] | India | Cross-sectional | 542 | Secondary school students | 14–18 | Father | Urban | Depression/anxiety and other psychiatric disorders | 7 | Fair |
| Sonmez [51] | Turkey | Cross-sectional | 8483 | High school students | Mean 16.12 (SD 0.99) | Parents | Urban | Substance use | 6 | Fair |
| Swahn [69] | Uganda | Cross-sectional | 457 | Youth living in the slums of Kampala | 14–24 | Parents | Urban | Problem behaviours | 9 | Good |
| Swahn [72] | Uganda | Cross-sectional | 457 | Youth living in the slums of Kampala | 14–24 | Parents | Urban | Suicidal ideation/behaviour | 9 | Good |
| Tavares [49] | Brazil | Cross-sectional | 2410 | Adolescents 9-11th grades | 10–19 | Family | Urban | Substance use | 8 | Fair |
| Tot [52] | Turkey | Cross-sectional | 3282 | Sixth grade, tenth grade and university students | Mean 15.75* | Parents | Urban | Substance use | 7 | Fair |
| Wood [35] | South Africa | Cross-sectional | 20 | Children and adolescents convicted of sex offences | 7–15 | Parents/household | Mixed | Problem behaviours | 6 | Fair |
| Xing [70] | China | Cross-sectional | 12,470 | High school students | 11–19 | Family | Mixed | Suicidal ideation/behaviour | 8 | Fair |
| Yarney [38] | Ghana | Cohort | 17 | Young people orphaned by AIDS | 12–17 | Caregiver | Mixed | Problem behaviours | 6 | Fair |
| Yurtseven [57] | Turkey | Cohort | 131 | Adolescents presenting to ED with drug use and positive tests | 13–18 | Parents | Mixed | Substance use | 7 | Fair |
| Zeren [39] | Turkey | Cross-sectional | 351 | Juveniles involved in a crime as suspects or victims | 0–18 (majority 16–18) | Parents | Urban | Problem behaviours | 7 | Fair |
| Zouini [63] | Morocco | Cross-sectional | 375 | High school students | 15–18 | Parents | Urban | Problem behaviours, Depression/anxiety and other psychiatric disorders; emotional problems | 6 | Fair |
*Overall population SD not reported
Sample and Household Characteristics
Four studies included only female adolescents, of which one looked only at pregnant females [34]; two at only males [35, 36], and the others included both genders. Most studies recruited adolescent participants from schools, although eight studies recruited directly from psychiatric facilities, both inpatient and outpatient. One study looked specifically at alcohol misuse impact on adolescents affected by caregiver HIV [37], one study looked at adolescents orphaned due to AIDS [38]. Another examined young sex offenders [35], and another juveniles who committed or were victims of crimes [39].
The majority (30 studies) were of urban households (e.g. [40]). One did not specify whether urban or rural [41]. Eight studies included households from mixed locations, incorporating both urban centres and rural areas (e.g. [35]). Three were rural locations [37, 42, 43], and one study was in a refugee camp [44].
Quality of Included Studies
NHLBI Quality Assessment Tool included studies ranged between 5 and 11 (out of 14). These scores were used to produce an ‘overall rating’ for which 32 studies were rated as ‘fair’, ten were rated ‘good’ and one ‘poor’. Overall ratings can be seen in Table 2. Studies commonly scored well for subjects being recruited from appropriate similar populations, and for clearly defining outcome measures. Few assessed exposures stratified by different levels of exposure (i.e. different levels of alcohol exposure).
Seventeen of the studies adjusted statistically for confounding variables. Only five studies measured different levels of exposure to alcohol; the remainder did not differentiate. All but one of the studies were of sufficient quality to be included in the main body of the results [36].
Household Alcohol Consumption
Alcohol exposure is summarised in Table 3. 'Family' included parents and siblings. 'Household' included all relatives living in the household. A number of studies that looked at parental alcohol exposure reported results for maternal and paternal exposure separately. One study looked at the effect of maternal alcohol consumption alone.
Table 3.
Summary of household alcohol exposure sources
| Household alcohol exposure | Number of studies | Adolescent Outcomes |
|---|---|---|
| Parents | 19 [34, 39, 43, 61–63, 54, 56–59, 61, 51–54, 56–58] | Depression/anxiety and other psychiatric disorders; substance use; teenage pregnancy; problem behaviours; emotional dysfunction; cognitive delay/disorder; suicidal ideation/behaviour |
| Family | 11 [35, 40–42, 46, 48, 49, 67, 70, 71, 85] | Suicidal ideation and behaviour; teenage pregnancy; self-harm; substance use; problem behaviours; emotional dysfunction; cognitive delay/disorder |
| Caregiver | 4 [37, 38, 44, 68] | Depression/anxiety and other psychiatric disorders; problem behaviours; emotional dysfunction |
| Household | 4 [35, 47, 50, 55] | Substance use; problem behaviours |
| Father | 4 [60, 64, 65, 73] | Suicidal ideation and behaviour; depression/anxiety and other psychiatric disorders |
| Mother | 1 [45] | Emotional dysfunction |
Few of the studies made any attempt to quantify alcohol use or to consider the different forms in which it was consumed; as an example, Burlaka et al. estimated the number of annual drinks [45]. Among others, Andrade et al. set a minimum threshold for being defined as a ‘high consumer’ of 250 ml of beer or 40 ml of distilled beverages on more than 1–2 days a week [46]. Many studies referred to ‘alcohol use’, ‘alcohol abuse’, ‘alcoholic’, and ‘problem drinking’, however definitions of these categories were often vague or non-existent. Four recognised alcohol scales were described across the studies: AUDIT [37], an Alcohol Abuse checklist [43], the Hispanic Americans Baseline Alcohol Survey [47], and the WHO-Thai Health Harm to Others from Drinking questionnaire [48].
Behavioural Outcomes
Behavioural outcomes assessed by included studies are summarised in Table 4. Some studies included more than one type of outcome. Results were heterogeneous, and therefore key study findings have been described individually in the sections below.
Table 4.
Summary of adolescent outcomes in included studies
| Adolescent outcome | Number of studies |
|---|---|
| Substance use (other than alcohol) | 12 [34, 46, 47, 49, 50, 49–55] |
| Depression/anxiety and other psychiatric disorders | 10 [37, 58–66] |
| Emotional dysfunction | 8 [43–45, 48, 58, 59, 63, 67] |
| Problem behaviour | 8 [35, 38, 39, 41, 44, 63, 68, 69] |
| Suicidal ideation and behaviour | 6 [37, 42, 70, 72–74] |
| Teenage pregnancy | 3 [34, 40, 75] |
| Cognitive delay/disorder | 3 [41, 58, 85] |
| Self-harm (non-suicidal) | 1 [71] |
Substance Use (Other Than Alcohol)
The most frequently linked adolescent outcome was substance use (of substances other than alcohol). Twelve studies showed some association between household alcohol misuse and adolescent substance use; tobacco was the most common outcome studied, but other substances were also mentioned. As stated in the methods, adolescents’ own use of alcohol was not a focus of this review. In Tavares et al. (Brazil), the prevalence ratio of drug use was 1.50 (95% Confidence Interval (CI) 1.19–1.90, p = 0.000) in adolescents who had alcoholism in the family [49]. This was similar to Riva et al. (Botswana) who reported a relative risk of 1.7 (95% CI 1.4–2.1) of illicit drug use in those with a problem drinker at home; however, this factor was no longer significant after incorporation in multivariable models [50]. In Madruga et al. (Brazil), the odds ratio for any illegal drug use in those exposed to domestic violence related to alcohol was 5.29 (95% CI 1.52–18.38) [47]. Sonmez et al. (Turkey) investigated impact of mothers and fathers drinking separately [51]. They found a significantly greater proportion of adolescents whose mothers misused alcohol used a number of substances compared to adolescents whose mothers did not drink. These included tobacco (38.2% vs 20.9%), cannabis (3.9% vs 1.0%), cocaine (1.3% vs 0.1%), heroin (0.9% vs 0.1%), and benzodiazepines (3.4% vs 0.2%) (p < 0.01 for all) [51]. Similar positive associations were found for paternal alcohol use (p < 0.05 for all, except adolescent heroin use, which was not statistically significant).
Regarding smoking, Tot et al. (Turkey) reported similar results for the prevalence of adolescent tobacco use; 31.7% in the children of maternal alcohol drinkers compared to 23.5% in children of maternal non-drinkers (p = 0.001); the equivalent figure for children whose fathers were alcohol drinkers being 28.0% vs 20.9% (p = 0.0001) [52]. Ozcan and Ozcan (Turkey) found with binomial logistic regression that paternal use of alcohol increased adolescent probability of smoking by 1.48 (p = 0.019), but maternal use had no significant effect [53]. Andrade et al. (Brazil) found a statistically significant association between adolescent tobacco smoking and maternal alcohol use (Adjusted Odds Ratio (OR) 1.91 (95% CI 1.00–3.66), p = 0.049); however, for paternal alcohol use there was no significant association (Adjusted OR 2.37 (95% CI 0.86–6.47) [46]. Evren et al. (Turkey) identified an increased risk of adolescent tobacco use when participants experienced problems due to the alcohol use of parents (OR 1.62, 95% CI 1.31–1.99) [54]. However, Francisco et al. (Mexico) in a study of adolescent girls with planned or unplanned pregnancy reported that alcohol drinking in the home was not associated with smoking in either group [34].
Hamdulay and Mash (South Africa) found that 59.8% of adolescents exposed to alcohol consumption at home smoked cannabis, compared to 40.2% among those who were not exposed (p = 0.05) [55]. Ciftci Demirci et al. (Turkey) found that 9.3% of adolescents admitted for treatment of substance use disorder (no control group) had parents who heavily abused alcohol; in Yurtseven et al., also in Turkey, 83% of illicit-drug using adolescents had a parent who consumed alcohol more than once a month [56, 57].
Depression/Anxiety and Other Psychiatric Disorders
Ten studies explored depression and other psychiatric disorders associated with exposure to household alcohol, with mixed results. Two studies in India reported significantly greater mean scores for depression and anxiety in the children of alcoholics compared to the children of non-alcoholics [58, 59]. In particular, Mansharamani et al. also found a significant difference in total scores using the ‘Childhood Psychopathology Measurement Schedule’ which was mean 6.10 in children of alcoholics, and mean 3.12 in children of non-alcoholics (p = 0.0001) [58]. Chaudhury et al. (Rwanda) noticed adolescents' self-reported anxiety and depression improved following an intervention aimed at reduction in caregiver alcohol use; the association reaching statistical significance [37]. In a sample of 620, Rahi et al. observed a higher prevalence of psychopathological disorder in children whose fathers abused alcohol than those whose fathers did not (20.2% vs 13.6%, p < 0.05) [60]. In a multi-country study in Laos, Mongolia, Nepal, and Sri Lanka, Lee et al. reported significantly increased odds ratios of psychological distress in the children of parents who used alcohol across three of four countries in unadjusted analyses; however this association was no longer significant in multivariate analyses [61]. Catani et al. found that paternal alcohol consumption was associated with increased family violence (p < 0.01) in a study in Sri Lanka [62]. In this study, family violence in turn was associated with significantly increased risk of PTSD in adolescents (p < 0.001), though there was no direct examination of the association between parental alcohol consumption and PTSD [62].
The other four studies investigating depression and other psychiatric disorders reported no direct association between household alcohol exposure and depression and anxiety disorders. In Zouini et al. there was no significant difference in mean scores for depression, somatisation, obsessive compulsiveness, psychoticism and anxiety between adolescents reporting parental alcohol us and the comparison group [63]. When assessing the prevalence of depression associated with the frequency of paternal drinking, Singh et al. (India) found that of those whose fathers drank every day (n = 21), 67% had depression; of those whose fathers drank occasionally (n = 100), 50.0% had depression; and of those whose fathers drank rarely (n = 54), 57.4% were depressed [64]. Khasakhala et al. (Kenya) found that there was no statistically significant association between major depressive disorder in adolescents whose fathers drink any alcohol, compared to adolescents whose fathers did not (OR 1.13, 95% CI 0.65–1.97) [65], and Pillay and van der Veen found there was no statistically significant association between prior substance abuse at home, 93% involving alcohol, and depression amongst child and adolescent psychiatric inpatients, in a small sample in South Africa [66].
Emotional Dysfunction
Eight studies explored varied emotional effects on adolescents exposed to household alcohol misuse. For example, Omkarappa and Rentala (2019) (India) found that children of alcoholics had a mean self-esteem score lower than children of non-alcoholics (19.54 vs 26.46, p = 0.001). Meyer et al., in a qualitative study of adolescents in a refugee camp in Thailand, described parental/caregiver drinking leading to fighting between caregivers and adolescents feeling ‘afraid’, ‘shy’, ‘mentally affected’, ‘melancholy’, and ‘stressed’ [44]. It was suggested that parents’ drinking and fighting were chronic stressors. In a study in India of 7560 students, 53.9% of boys and 33.0% of girls reported experiencing psychological harm from others’ drinking, with examples including being called names or insulted [48].
However, five studies reported mixed/negative outcomes in this domain. Karatay and Bas (Turkey) initially found that self-efficacy score was lower in those who had alcohol users in the family vs those who did not (88.21 vs 95.81, p < 0.001) but this was no longer significant after multiple regression analysis [67]. Gulati and Dutta (India) found in a multiple linear regression analysis that the father’s alcohol abuse status was not significant as a risk variable for internalised or externalised behaviours [43]. Similarly, Burlaka et al. (Ukraine) found no association between internalising behaviours and maternal alcohol misuse, and Mansharamani et al. found no difference in scores for ‘physical illness with emotional problems’ between children with alcoholics and children of non-alcoholics (mean 0.48 vs 0.46, p = 0.88) [45]. Finally, Zouini et al. (Morocco) found no significant difference in mean scores for interpersonal sensitivity between the adolescents reporting parental alcohol use and the comparison group [63].
Problem Behaviour
Eight studies investigated a range of problem behaviours associated with exposure to household alcohol, with mixed associations found. Jogdand and Naik (2014) (India) found 56.3% of adolescents with parent/carer alcoholism exhibited behavioural problems (OR 1.56, 95% CI 1.12–2.17) [68]. Meyer et al., in a qualitative study of adolescents in refugee camps in Thailand, reported behavioural effects of exposure to adult drinking: adolescents 'don't attend school, don't go among people, go against parents, hiding’ [44]. Kheokao et al. (Thailand) reported a significant correlation between family drinking and absenteeism [41]. Yarney et al., in another qualitative study looking at adolescents in Ghana orphaned by AIDS, suggested that orphans were vulnerable to “pilfering and other social vices” when caregivers spent money on time on social activities including drinking, suggesting this was because it reduced worsened finances and caregiver presence at home [38]. In a study of 20 young people convicted of sex offences in South Africa, Wood et al. found that 75% of the sample one or more family members abused alcohol [35]. However, in Swahn et al. (Uganda) an initial elevated odds ratio (OR 4.59, 95% CI 1.18–17.96) of violence perpetration in youth who reported parental neglect due to alcohol use was no longer significant after adjustment (Adjusted OR 2.55 (95% CI 0.48–13.63) [69]. In Zeren et al., when comparing characteristics of young people suspected of committing, or victims of, crimes, there was little difference between the proportion of suspects and victims with fathers who abused alcohol (4.9% vs 5.6%); this was not assessed for statistical significance [39]. Only 3 participants (1%) had mothers who abused alcohol. In Zouini et al. (Morocco) there was no significant difference in mean scores for hostility in those adolescents reporting parental alcohol use problems versus the comparison group [63].
Suicidal Ideation and Behaviour
Six studies examined the associations, varying in strength, between exposure to household alcohol and suicidal ideation and/or behaviour. Xing et al. found an increased prevalence of suicide attempts in the past year in those who had a family member with an alcohol abuse problem (4.4% vs 2.2%, p < 0.001) [70]. Guvendeger Doksat et al. (Turkey) found that a history of alcohol use by parents increased the risk of suicide attempts in their adolescents hospitalised for substance use (OR 1.664, p = 0.001) [71]. Swahn et al. (Uganda) found that of youth reporting parental neglect due to alcohol use, there was an elevated adjusted odds ratio for suicidal ideation (Adjusted OR 2.09 (1.16–3.77) [72]. Conversely, Khasakhala et al. (Kenya) found that there was no significant association between the presence of paternal alcohol use disorder and the occurrence of suicidal behaviour (OR 1.86, 95% CI 0.88–3.92) [73]. There were two descriptive studies; Betancourt et al., in a study in rural Rwanda, found that 4 out of 20 youths reporting current suicidality identified alcohol abuse in the family as a reason for suicidal behaviour (42). In Singh et al. (India), 9.6% of adolescents admitted to a paediatric unit for suicide attempts by ingestion had alcoholism in the family [74].
Teenage Pregnancy
Three studies suggested an association between teenage pregnancy and household alcohol misuse. Caputo and Bordin (Brazil) found a statistically significant association, with 17% of pregnant girls having a family member getting drunk more than once a week compared to 8.4% of non-pregnant girls (OR 2.2, 95% CI 1.1–4.3, p = 0.014) [40]. It was suggested that harmful alcohol use in the family acted as a permanent stress factor. Faler et al. (Brazil) also found an association (OR 1.33, 95% CI 1.05–1.68, p = 0.016) with parental alcohol problems [75]. Francisco et al. (Mexico) looked specifically at pregnant girls to see whether pregnancy was planned or unplanned, finding that alcohol consumption at home was present in 60.4% of planned pregnancies compared with 77.5% of unplanned pregnancies (p < 0.05) [34].
Self-harm
Guvendeger Doksat et al. found that in a large study of adolescents admitted to a psychiatric hospital in Turkey for treatment of substance use disorder, non-suicidal self-injury was present in over half of those whose relatives used alcohol compared to those who did not (57.3% vs 42.7%, p = 0.016) [71]. The association between paternal alcohol use and the presence of non-suicidal self-injury was statistically significant (63.9% vs 36.1%, p < 0.0001), but not the presence of maternal alcohol use (68.8% vs 31.2%, p = 0.175), although the sample size was small in the latter case.
Neurodevelopmental Outcomes in Adolescents
Although this systematic review sought to include neurodevelopmental outcomes (such as attention deficit hyperactivity disorder, autism spectrum disorder, global developmental delay, intellectual disability), the majority of studies of adolescents identified did not investigate these outcomes, and no studies investigated these outcomes in a purely adolescent population. The parallel paper to this review, focusing on neurodevelopmental and behavioural outcomes in children, reported a high number of relevant papers, indicating a greater focus of the research field into specifically neurodevelopmental outcomes at the younger years.
Mechanisms/Subgroup Analysis
Very few studies provided information on household socioeconomic status, malnutrition, or stunting. Where such information was provided, it was not linked to alcohol consumption or behavioural outcomes. Therefore, no conclusions can be drawn about the impact of these factors on the associations found.
The majority of studies focused on households in urban locations. Trends in terms of outcomes were similar across studies in urban and mixed locations. Due to the variety of outcomes and the lack of studies of rural households, it is not possible to comment on differences between urban/rural households, except that no outcomes were reported as unique to rural households.
The role of adolescent resilience as a mediating factor was raised by a few studies; adolescents with higher levels of resilience were reported as being better able to withstand the impact of household alcohol misuse, exhibiting less emotional dysfunction and problem behaviours. Other studies in high income countries have noted similar findings [37].
Discussion
What is Already Known on This Topic
Exposure to excessive household alcohol drinking is known to increase the risk of adverse child and adolescent health outcomes in high income countries [76]. This is known to be particularly true for maternal alcohol consumption [77]. These adverse outcomes are known to include a wide range of behavioural problems, cognitive effects, and increased rates of mental illness, as well as physical health problems [1]. Isolated studies have suggested the same relationship between adverse experiences and outcomes is true in low- and middle-income countries (see, for example, [78, 79]).
What This Study Adds
This review confirms that, despite the heterogeneity of results, exposure to more than modest household alcohol use seems to be associated with some negative adolescent behavioural outcomes in many lower- and middle-income countries, just as in higher income countries. Many studies found statistically significant associations between household alcohol misuse and adolescent mental illness, problem behaviours, self-harm, and teenage pregnancy. Both maternal and paternal alcohol misuse emerged as key risk factors contributing to impact on adolescents.
Studies included in this review also speculated on mechanisms that might explain the link between household alcohol misuse and adverse adolescent outcomes. Parental alcohol misuse was theorised to act as chronic stressor, a marker of broader family dysfunction, and a shaper of adolescent attitudes to lifestyle and health behaviours. Studies frequently did not adjust for confounding factors, so it is not possible to identify a direct causal link between household alcohol alone and adverse impacts.
The heterogeneity in the results, the relative lack of statistical approaches and of appropriate control groups, necessitate that more studies be undertaken, using control groups or population samples, with clear definitions of use and misuse of alcohol and/or careful quantification of household alcohol use, in order that more concrete conclusions can be drawn. Alcohol use patterns including amount, frequency, type, and location of drinking need to be measured. Studies need to include measures of other factors which could increase adolescent risk such as socioeconomic deprivation, education, peer influence, and protective factors within the family and household.
Control groups were lacking in several studies; prospective cohort studies would address this. The inclusion of questions on household alcohol use and misuse in future prospective cohort studies of adolescents would provide valuable data. Numerous high-income countries already conduct regular surveys of adolescent health; questions on household alcohol misuse in all countries could be added to these [80, 81]. Better designed case control studies would be recommended, using as cases adolescents experiencing an outcome identified in this review and securing better information on both maternal, paternal and household alcohol use. As most of the studies thus far have focused on urban settings, more research in rural households would add to generalisability. Risk factors, negative adolescent outcomes, and potential mechanisms may well be significantly different in rural environments. Similarly, there is a need for studies to address other LMICs not included in this review, results from which would add nuance, highlight differences, and expand on our findings.
Further research also needs to be done to illuminate the mechanisms through which household alcohol misuse may impact on negative behavioural outcomes among adolescents. The absence of robust data on other exposures and the lack of comparison groups necessitates further research to allow evaluation of speculated mechanisms. Inclusion of information on important covariates, household income, partner violence, harsh discipline, physical or sexual adolescent abuse, and family functioning would allow research to consider confounding or mediating factors and interaction affecting the relationship between household alcohol misuse and negative adolescent outcomes. Previous studies have included alcohol as one of a list of ACEs [1] whereby it has not been possible to explore the independent role of household alcohol misuse and its relationship with other adverse experiences.
Significantly, very few of the included studies attempted to explicitly explore the relationship between amount of alcohol consumed and adolescent outcomes. Loose definitions of 'alcohol abuse' or 'problem drinking' were used to compare outcomes with little quantification of amount or context. It is not at all clear from the studies available whether there is a correlation between amount of alcohol exposure and severity of or frequency of adolescent problems. Consequently, it has not been possible to identify whether or not there is a level of household alcohol use that might be considered safe, or indeed to suggest what amount might be harmful. The nature of exposure to household alcohol was also poorly defined in the included studies. There was little indication of the extent to which adolescents were directly exposed either to drinking or drunkenness; it was not clear whether alcohol use mostly occurred at home in the adolescents' presence or outside the house. Furthermore, it was not always clear whether exposure to alcohol was historic or contemporaneous. This distinction may have important consequences in terms of outcomes, as well as potentially influencing causal relationships and consequently policy development. The majority of studies took place in urban areas, indicating a large proportion of children in LMICs have thus far been excluded from research in this area. Finally, though the systematic review also aimed to summarise adolescent studies describing neurodevelopmental outcomes, no study focused on this outcome in this age range.
Limitations of this Review
Limitations of the review included the decision to exclude studies published before 1990, which meant that potentially relevant studies may have been missed. Excluding studies not available in English meant that some potentially important studies could not be considered. As in any systematic review, publication bias means that studies that did not find associations tended to be underrepresented.
The decision to include a wide age range of subjects from 10 to 18 meant that it was possible that a small minority of subjects had not yet started puberty, or had completed puberty, and were therefore not ‘adolescents’ in the traditional sense. This was done in order to avoid excluding otherwise relevant high quality studies. Detailed subgroup analyses of these studies would not have been possible, as the majority merely reported ages and did not assess puberty status, or report results by age categories. Definitive assessment of puberty and adolescence is difficult, a subject of ongoing academic debate, and can be based on variable categories and guidelines [82, 83]. Age is a common proxy for adolescence, and puberty is complex to assess (see RCPCH guidelines [84]). It is inevitable therefore that a small amount of misclassification may have occurred.
This review incorporated studies from a wide range of LMICs across Asia, Africa, and South America. Findings may well be somewhat generalisable. This being said, LMICs are not homogeneous, and varying cultural and socio-economic circumstances directly impact both understandings of alcohol misuse and adolescent outcomes, thereby limiting transferability of findings. In particular, given that only English language studies were included, otherwise relevant research may have been overlooked. Given that attitudes towards alcohol use and misuse, and particularly understandings of what is excessive or inappropriate, vary widely across cultural contexts, conclusions should be extended to different contexts with caution.
Summary
This review shows that exposure to household alcohol misuse in the context of low- and middle-income countries is associated with a range of adverse adolescent outcomes. This was the case across a wide range of countries. Although results were heterogeneous and amounts of alcohol poorly quantified, some statistically significant associations were described between parental alcohol misuse and adolescent suicidality, depression, anxiety, substance use, problem behaviour, teenage pregnancy, and self-harm. Further research is called for, with more studies needed to allow hypotheses to be tested, and study of differences associated with country-specific contexts. In particular, careful quantification of alcohol misuse and characterization as risky drinking, dependent drinking or binge drinking might help to better establish the impact of exposure on the adolescents in the home. In addition, inclusion of key covariates and study designs including control groups would help an investigation of the mechanisms by which alcohol exposure is associated with these outcomes.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author Contributions
LLD and LM conceived of and led the review. TH developed the protocol and performed initial searches, supervised by EA. TJ and TH undertook the majority of the screening and data extraction, supervised and assisted by EA. PP, ID and DB contributed to the screening and data extraction. EA and PP undertook the 2020 search, extraction and update. TJ wrote the first draft of the review and EA, LLD, LM and TH provided the majority of further contributions to refining the draft and producing the final manuscript. All authors contributed to and approved of the final version of the manuscript.
Funding
Logan Manikam is funded by a UK National Institute for Health Research Advanced Fellowship (Ref: NIHR300020) and is Director of Aceso Global Health Consultants Limited. The research work by Davidson PI reported in this publication was supported in part by the National Institutes of Health, Fogarty International Center, National Institutes of Health, and Office of Behavioral and Social Sciences Research, Office of Disease Prevention under Award Number R01-TW011228. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Compliance with Ethical Standards
Conflicts of interest
Logan Manikam is funded by a UK National Institute for Health Research Advanced Fellowship (Ref: NIHR300020) and is Director of Aceso Global Health Consultants Limited. The research work by Davidson PI reported in this publication was supported in part by the National Institutes of Health, Fogarty International Center, National Institutes of Health, and Office of Behavioral and Social Sciences Research, Office of Disease Prevention under Award Number R01-TW011228. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Ethical Approval
All procedures performed in this study were in accordance with the ethical standards of the institution of the authors and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was registered in PROSPERO, CRD42017070209. This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed consent is not applicable as this article is a review.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Heal. 2017;2(8):e356–e366. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- 2.Wazen RM, Kuroda S, Nishio C, Sellin K, Brunski JB, Nanci A. Adolescent precocious development and young adult health outcomes. Adv Life Course Res. 2014;8(9):1385–1395. [Google Scholar]
- 3.Blum RW, Bastos FIPM, Kabiru CW, Le LC. Adolescent health in the 21st century. Lancet. 2012;379(9826):1567–1568. doi: 10.1016/S0140-6736(12)60407-3. [DOI] [PubMed] [Google Scholar]
- 4.Davidson LL, Grigorenko EL, Boivin MJ, Rapa E, Stein A. A focus on adolescence to reduce neurological, mental health and substance-use disability. Nature. 2015;527:S161. doi: 10.1038/nature16030. [DOI] [PubMed] [Google Scholar]
- 5.Garrido EF, Weiler LM, Taussig HN. Adverse childhood experiences and health-risk behaviors in vulnerable early adolescents. J Early Adolesc. 2018;38(5):661–680. doi: 10.1177/0272431616687671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anda RF, Whitfield CL, Felitti VJ, Chapman D, Edwards VJ, Dube SR, et al. Adverse childhood experiences, alcoholic parents, and later risk of alcoholism and depression. Psychiatr Serv. 2002;53(8):1001–1009. doi: 10.1176/appi.ps.53.8.1001. [DOI] [PubMed] [Google Scholar]
- 7.Dörrie N, Föcker M, Freunscht I, Hebebrand J. Fetal alcohol spectrum disorders. Eur Child Adolesc Psychiatry. 2014;23(10):863–875. doi: 10.1007/s00787-014-0571-6. [DOI] [PubMed] [Google Scholar]
- 8.O’Connor MJ. Mental health outcomes associated with prenatal alcohol exposure: genetic and environmental factors. Curr Dev Disord Reports. 2014;1(3):181–188. [Google Scholar]
- 9.Smyth A, Teo KK, Rangarajan S, O’Donnell M, Zhang X, Rana P, et al. Alcohol consumption and cardiovascular disease, cancer, injury, admission to hospital, and mortality: a prospective cohort study. Lancet. 2015;386(10007):1945–1954. doi: 10.1016/S0140-6736(15)00235-4. [DOI] [PubMed] [Google Scholar]
- 10.Bongaarts J, Zimmer Z. Living arrangements of older adults in the developing world: an analysis of demographic and health survey household surveys. J Geronotology Soc Sci. 2002;57B(3):S145–S157. doi: 10.1093/geronb/57.3.s145. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organisation (2018) 3, Household crowding [Internet]. WHO Housing and Health Guidelines. https://www.ncbi.nlm.nih.gov/books/NBK535289/. Accessed 24 May 2019
- 12.Metzler M, Merrick MT, Klevens J, Ports KA, Ford DC. Adverse childhood experiences and life opportunities: shifting the narrative. Child Youth Serv Rev. 2017;72:141–149. doi: 10.1016/j.childyouth.2016.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bhutta ZA, Guerrant RL, Nelson CA. Neurodevelopment, nutrition, and inflammation: the evolving global child health landscape. Pediatrics. 2017;139(Supplement 1):S12–22. doi: 10.1542/peds.2016-2828D. [DOI] [PubMed] [Google Scholar]
- 14.Huq T, Alexander EC, Manikam L, Jokinen T, Patil P, Benjumea D, Das I, Davidson LL (2020) A systematic review of household and family alcohol use and childhood developmental outcomes in low- and middle-income countries. [Unpublished] [DOI] [PMC free article] [PubMed]
- 15.The World Bank. Low & Middle Income [Internet]. 2017 [cited 2017 Apr 1]. Available from: https://data.worldbank.org/income-level/low-and-middle-income
- 16.American Psychological Association. Developing Adolescents: A Reference for Professionals [Internet]. Washington, DC, US; 2002. Available from: https://www.apa.org/pi/families/resources/develop.pdf
- 17.Blakemore S-J, Burnett S, Dahl RE. The role of puberty in the developing adolescent brain. Hum Brain Mapp. 2010;31(6):926–933. doi: 10.1002/hbm.21052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Giedd JN, Blumenthal J, Jeffries NO, Castellanos FX, Liu H, Zijdenbos A, et al. Brain development during childhood and adolescence: a longitudinal MRI study. Nat Neurosci. 1999;2:861. doi: 10.1038/13158. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organisation. Recognizing adolescence [Internet]. Adolescence: a period needing special attention. 2014 [cited 2020 Jul 23]. Available from: https://apps.who.int/adolescent/second-decade/section2/page1/recognizing-adolescence.html
- 20.Biro FM, Greenspan LC, Galvez MP, Pinney SM, Teitelbaum S, Windham GC, et al. Onset of breast development in a longitudinal cohort. Pediatrics. 2013;132(6):1019LP–1027LP. doi: 10.1542/peds.2012-3773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.UNICEF, Youth Polcy Lab. Age Matters! Age-related barriers to service access and the realisation of rights for children, adolescents and youth [Internet]. 2017. Available from: https://agemattersnow.org/downloads/YPL_Age_Matters_Final_Report_Oct2016.pdf
- 22.World Health Organisation. Fact Sheets: Alcohol [Internet]. 2018 [cited 2019 Feb 9]. Available from: https://www.who.int/en/news-room/fact-sheets/detail/alcohol
- 23.Yap MBH, Cheong TWK, Zaravinos-tsakos F, Lubman DI. Modifiable parenting factors associated with adolescent alcohol misuse: a systematic review and meta-analysis of longitudinal studies. Addiction. 2017;112(7):1142–1162. doi: 10.1111/add.13785. [DOI] [PubMed] [Google Scholar]
- 24.Rossow I, Keating P, Felix L, Mccambridge J. Does parental drinking influence children’s drinking? A systematic review of prospective cohort studies. Addiction. 2016;111(2):204–217. doi: 10.1111/add.13097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marshall EJ. Adolescent alcohol use: risks and consequences. Alcohol Alcohol. 2014;49(2):160–164. doi: 10.1093/alcalc/agt180. [DOI] [PubMed] [Google Scholar]
- 26.McMorris BJ, Catalano RF, Kim MJ, Toumbourou JW, Hemphill SA. Influence of family factors and supervised alcohol use on adolescent alcohol use and harms: similarities between youth in different alcohol policy contexts. J Stud Alcohol Drugs. 2011;72(3):418–428. doi: 10.15288/jsad.2011.72.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The Cochrane Library. LMIC Filters [Internet]. 2017 [cited 2017 Jul 1]. Available from: https://epoc.cochrane.org/lmic-filters
- 28.Puchalski Ritchie LM, van Lettow M, Hosseinipour MC, Rosenberg NE, Phiri S, Landes M, et al. The effectiveness of interventions to improve uptake and retention of HIV-infected pregnant and breastfeeding women and their infants in prevention of mother-to-child transmission care programs in low- and middle-income countries: protocol for a systemati. Syst Rev. 2015;4(1):144. doi: 10.1186/s13643-015-0136-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khatib R, Arevalo YA, Berendsen MA, Prabhakaran S, Huffman MD. Presentation, evaluation, management, and outcomes of acute stroke in low- and middle-income countries: a systematic review and meta-analysis. Neuroepidemiology. 2018;51(1–2):104–112. doi: 10.1159/000491442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hansoti B, Kelen GD, Quinn TC, Whalen MM, DesRosiers TT, Reynolds SJ, et al. A systematic review of emergency department based HIV testing and linkage to care initiatives in low resource settings. PLoS ONE. 2017;12(11):e0187443. doi: 10.1371/journal.pone.0187443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Siriwardhana DD, Hardoon S, Rait G, Weerasinghe MC, Walters KR. Prevalence of frailty and prefrailty among community-dwelling older adults in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Open. 2018;8(3):e018195. doi: 10.1136/bmjopen-2017-018195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.NICE. NICE Glossary [Internet]. National Institute of Clinical Excellence (NICE). 2017 [cited 2017 Apr 1]. Available from: https://www.nice.org.uk/glossary
- 33.National Heart Lung and Blood Institute (NHLBI). Study Quality Assessment Tools [Internet]. Study Quality Assessment Tools. 2020 [cited 2020 May 10]. Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- 34.Francisco V-N, Carlos V-R, Eliza V-R, Octelina C-R, Maria II. Tobacco and alcohol use in adolescents with unplanned pregnancies: Relation with family structure, tobacco and alcohol use at home and by friends. Afr Health Sci. 2016;16(1):27–35. doi: 10.4314/ahs.v16i1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wood C, Welman M, Netto L. A profile of young sex offenders in South Africa. South African J Child Adolesc Ment Heal. 2000;12(1):45–58. [Google Scholar]
- 36.Praharaj SK, Verma P, Arora M. Inhalant abuse (typewriter correction fluid) in street children. J Addict Med. 2008;2(4):175–177. doi: 10.1097/ADM.0b013e31817be5bc. [DOI] [PubMed] [Google Scholar]
- 37.Chaudhury S, Brown FL, Kirk CM, Mukunzi S, Nyirandagijimana B, Mukandanga J, et al. Exploring the potential of a family-based prevention intervention to reduce alcohol use and violence within HIV-affected families in Rwanda. AIDS Care. 2016;28(sup2):118–129. doi: 10.1080/09540121.2016.1176686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yarney L, Mba C, Asampong E. Qualitative study on the socio-cultural determinants of care of children orphaned by AIDS in the Ashanti and Eastern regions of Ghana. BMC Public Health. 2015;15(1):1–13. doi: 10.1186/s12889-014-1332-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zeren C, Arslan MM, Yengil E, Karanfil R, Arçan R, Oksuz M. Socio-demographic characteristics of juvenile delinquents in Turkey. J Forens Psychiatry Psychol. 2013;24(6):688–698. [Google Scholar]
- 40.Caputo VG, Bordin IA. Teenage pregnancy and frequent use of alcohol and drugs in the home environment. Rev Saude Publica. 2008;42(3):402–410. doi: 10.1590/s0034-89102008000300003. [DOI] [PubMed] [Google Scholar]
- 41.Kheokao JK, Kirkgulthorn T, Yingrengreung S, Singhprapai P. Effects of school, family and alcohol marketing communication on alcohol use and intentions to drink among Thai students. Southeast Asian J Trop Med Public Heal. 2013;44(4):718–726. [PubMed] [Google Scholar]
- 42.Betancourt T, Smith Fawzi MC, Stevenson A, Kanyanganzi F, Kirk C, Ng L, et al. Ethics in community-based research with vulnerable children: perspectives from Rwanda. PLoS ONE. 2016 doi: 10.1371/journal.pone.0157042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gulati JK, Dutta J. Risk, conflict between parents and child adjustment in families experiencing persistent poverty in India. J Fam Stud. 2008;14(1):107–123. [Google Scholar]
- 44.Meyer S, Murray LK, Puffer ES, Larsen J, Bolton P. The nature and impact of chronic stressors on refugee children in Ban Mai Nai Soi camp, Thailand. Glob Public Health. 2013;8(9):1027–1047. doi: 10.1080/17441692.2013.811531. [DOI] [PubMed] [Google Scholar]
- 45.Burlaka V, Kim YJ, Crutchfield JM, Lefmann TA, Kay ES. Predictors of internalizing behaviors in ukrainian children. Fam Relations An Interdiscip J Appl Fam Stud. 2017;66(5):854–866. doi: 10.1111/fare.12289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Andrade RCC, Ferreira AD, Ramos D, Ramos EMC, Scarabottolo CC, Saraiva BTC, et al. Smoking among adolescents is associated with their own characteristics and with parental smoking: cross-sectional study. Sao Paulo Med J. 2017;135(6):561–567. doi: 10.1590/1516-3180.2017.0154220717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Madruga CS, Laranjeira R, Caetano R, Pinsky I, Zaleski M, Ferri CP. Use of licit and illicit substances among adolescents in Brazil—a national survey. Addict Behav. 2012;37(10):1171–1175. doi: 10.1016/j.addbeh.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 48.Jaisoorya TS, Beena KV, Ravi GS, Thennarasu K, Benegal V. Alcohol harm to adolescents from others’ drinking: a study from Kerala. Indian J Psychiatry. 2018;60(1):90–96. doi: 10.4103/psychiatry.IndianJPsychiatry_186_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tavares BF, Béria JU, Lima MS de. Fatores associados ao uso de drogas entre adolescentes escolares . Vol. 38, Revista de Saúde Pública . scielo ; 2004. p. 787–96. [DOI] [PubMed]
- 50.Riva K, Allen-Taylor L, Schupmann WD, Mphele S, Moshashane N, Lowenthal ED. Prevalence and predictors of alcohol and drug use among secondary school students in Botswana: a cross-sectional study. BMC Public Health. 2018;18(1):1396. doi: 10.1186/s12889-018-6263-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sonmez MB, Cakir D, Cinar RK, Gorgulu Y, Vardar E. Substance use and parent characteristics among high school students: Edirne sample in Turkey. J Child Adolesc Subst Abus. 2016;25(3):260–267. [Google Scholar]
- 52.Tot S, Yazc K, Yazc A, Metin O, Bal N, Erdem P. Psychosocial correlates of substance use among adolescents in Mersin, Turkey. Public Health. 2004;118(8):588–593. doi: 10.1016/j.puhe.2004.02.009. [DOI] [PubMed] [Google Scholar]
- 53.Ozcan YZ, Ozcan KM. Determinants of youth smoking—evidence from Turkey. Subst Use Misuse. 2002;37(3):313–336. doi: 10.1081/ja-120002481. [DOI] [PubMed] [Google Scholar]
- 54.Evren C, Ogel K, Demirci A, Evren B, Yavuz B, Bozkurt M. Prevalence of lifetime tobacco, alcohol and drug use among 10th grade students in Istanbul. Klin Psikofarmakol Bul Clin Psychopharmacol. 2014;24(3):201. [Google Scholar]
- 55.Hamdulay A, Mash R. The prevalence of substance use and its associations amongst students attending high school in Mitchells Plain, Cape Town. South African Fam Pract. 2011;53(1):83–90. [Google Scholar]
- 56.Ciftçi Demirci A, Erdoğan A, Yalçın O, Yıldızhan E, Koyuncu Z, Eseroğlu T, et al. Sociodemographic characteristics and drug abuse patterns of adolescents admitted for substance use disorder treatment in Istanbul. Am J Drug Alcohol Abuse. 2014;30(3):1–8. doi: 10.3109/00952990.2014.973961. [DOI] [PubMed] [Google Scholar]
- 57.Yurtseven A, Turan C, Yuncu Z, Annette Akgur S, Saz EU. Substance use frequency and related characteristics among adolescents presenting to an emergency department in Turkey. J Ethn Subst Abuse. 2019;5:1–11. doi: 10.1080/15332640.2019.1685048. [DOI] [PubMed] [Google Scholar]
- 58.Mansharamani H, Patil PS, Behere PB, Mansharamani D, Nagdive A. Psychiatric morbidity in children of alcoholic parents. Ind Psychiatry J. 2018;27(2):226–230. doi: 10.4103/ipj.ipj_57_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Omkarappa D, Rentala S. Anxiety, depression, self-esteem among children of alcoholic and nonalcoholic parents. J Fam Med Prim Care. 2019;8(2):604. doi: 10.4103/jfmpc.jfmpc_282_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rahi M, Kumavat AP, Garg S, Singh MM. Socio-demographic co-relates of psychiatric disorders. Indian J Pediatr. 2005;72(5):395–398. doi: 10.1007/BF02731734. [DOI] [PubMed] [Google Scholar]
- 61.Lee H, Lee EY, Greene B, Shin Y. Psychological distress among adolescents in Laos, Mongolia, Nepal, and Sri Lanka. Asian Nurs Res (Korean Soc Nurs Sci) 2019;13(2):147–153. doi: 10.1016/j.anr.2019.04.001. [DOI] [PubMed] [Google Scholar]
- 62.Catani C, Jacob N, Schauer E, Kohila M, Neuner F. Family violence, war, and natural disasters: a study of the effect of extreme stress on children’s mental health in Sri Lanka. BMC Psychiatry. 2008 doi: 10.1186/1471-244X-8-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zouini B, Sfendla A, Hedman Ahlström B, Senhaji M, Kerekes N. Mental health profile and its relation with parental alcohol use problems and/or the experience of abuse in a sample of Moroccan high school students: an explorative study. Ann Gen Psychiatry. 2019;18(1):27. doi: 10.1186/s12991-019-0251-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Singh MM, Gupta M, Grover S. Prevalence & factors associated with depression among schoolgoing adolescents in Chandigarh, north India. Indian J Med Res. 2017;146(2):205–215. doi: 10.4103/ijmr.IJMR_1339_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Khasakhala LI, Ndetei DM, Mathai M, Harder V. Major depressive disorder in a Kenyan youth sample: relationship with parenting behavior and parental psychiatric disorders. Ann Gen Psychiatry. 2013;12(1):15. doi: 10.1186/1744-859X-12-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pillay AL, van der Veen MB. Prevalence of parental substance-abuse among child psychiatric inpatients. Percept Mot Skills. 1997;84(3 Pt 1):947–953. doi: 10.2466/pms.1997.84.3.947. [DOI] [PubMed] [Google Scholar]
- 67.Karatay G, Baş N. Factors affecting substance use and self-efficacy status of students in eastern Turkey. Cien Saude Colet. 2019;2(24):1317–1326. doi: 10.1590/1413-81232018244.30252017. [DOI] [PubMed] [Google Scholar]
- 68.Jogdand SS, Naik J. Study of family factors in association with behavior problems amongst children of 6–18 years age group. Int J Appl basic Med Res. 2014;4(2):86–89. doi: 10.4103/2229-516X.136783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Swahn MH, Gressard L, Palmier JB, Kasirye R, Lynch C, Yao H. Serious violence victimization and perpetration among youth living in the slums of Kampala, Uganda. West J Emerg Med. 2012;13(3):253–259. doi: 10.5811/westjem.2012.3.11772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Xing X-Y, Tao F-B, Wan Y-H, Xing C, Qi X-Y, Hao J-H, et al. Family factors associated with suicide attempts among Chinese adolescent students: a national cross-sectional survey. J Adolesc Health. 2010;46(6):592–599. doi: 10.1016/j.jadohealth.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 71.Guvendeger Doksat N, Zahmacioglu O, Ciftci Demirci A, Kocaman GM, Erdogan A. Association of suicide attempts and non-suicidal self-injury behaviors with substance use and family characteristics among children and adolescents seeking treatment for substance use disorder. Subst Use Misuse. 2017;52(5):604–613. doi: 10.1080/10826084.2016.1245745. [DOI] [PubMed] [Google Scholar]
- 72.Swahn MH, Palmier JB, Kasirye R, Yao H. Correlates of suicide ideation and attempt among youth living in the slums of Kampala. Int J Environ Res Public Health. 2012;9(2):596–609. doi: 10.3390/ijerph9020596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Khasakhala LI, Ndetei DM, Mathai M. Suicidal behaviour among youths associated with psychopathology in both parents and youths attending outpatient psychiatric clinic in Kenya. Ann Gen Psychiatry. 2013;12(1):13. doi: 10.1186/1744-859X-12-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Singh P, Sengupta D, Deshpandey U. Adolescents communicating distress through suicidal behaviours. Natl J Med Res. 2015;5(2):132–135. [Google Scholar]
- 75.Faler CS, Câmara SG, Aerts DRGC, Alves GG, Béria JU. Family psychosocial characteristics, tobacco, alcohol, and other drug use, and teenage pregnancy. Cad Saude Publica. 2013;29(8):1654–1663. doi: 10.1590/0102-311x00107812. [DOI] [PubMed] [Google Scholar]
- 76.Christoffersen MN, Soothill K. The long-term consequences of parental alcohol abuse: a cohort study of children in Denmark. J Subst Abuse Treat. 2003;25(2):107–116. doi: 10.1016/s0740-5472(03)00116-8. [DOI] [PubMed] [Google Scholar]
- 77.Hafekost K, Lawrence D, O’Leary C, Bower C, Semmens J, Zubrick SR. Maternal alcohol use disorder and child school attendance outcomes for non-Indigenous and Indigenous children in Western Australia: a population cohort record linkage study. BMJ Open. 2017;7:e015650. doi: 10.1136/bmjopen-2016-015650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ramiro LS, Madrid BJ, Brown DW. Adverse childhood experiences (ACE) and health-risk behaviors among adults in a developing country setting. Child Abuse Negl. 2010;34(11):842–855. doi: 10.1016/j.chiabu.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 79.Xiao Q, Dong MX, Yao J, Li WX, Ye DQ. Parental alcoholism, adverse childhood experiences, and later risk of personal alcohol abuse among Chinese medical students. Biomed Environ Sci. 2008;21(5):411–419. doi: 10.1016/S0895-3988(08)60062-8. [DOI] [PubMed] [Google Scholar]
- 80.Harris KM, Udry JR. National Longitudinal Study of Adolescent to Adult Health (Add Health), 1994–2008 [Public Use] [Internet]. Carolina Population Center, University of North Carolina-Chapel Hill, Inter-university Consortium for Political and Social Research; 2018. Available from: https://www.cpc.unc.edu/projects/addhealth
- 81.NHS Digital. National Study of Health and Wellbeing: Children and Young People [Internet]. NHS Digital. 2018 [cited 2019 May 16]. Available from: https://digital.nhs.uk/data-and-information/areas-of-interest/public-health/national-study-of-health-and-wellbeing-children-and-young-people
- 82.Marceau K, Ram N, Houts RM, Grimm KJ, Susman EJ. Individual differences in boys’ and girls’ timing and tempo of puberty: modeling development with nonlinear growth models. Dev Psychol. 2011;47(5):1389–1409. doi: 10.1037/a0023838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Casey BJ, Jones RM, Hare TA. The adolescent brain. Ann N Y Acad Sci [Internet]. 2008 Mar;1124:111–26. Available from: https://pubmed.ncbi.nlm.nih.gov/18400927 [DOI] [PMC free article] [PubMed]
- 84.Royal College of Paediatrics and Child Health. UK-WHO growth charts - childhood and puberty close monitoring (CPCM) chart [Internet]. 2013 [cited 2020 Jul 7]. Available from: https://www.rcpch.ac.uk/resources/uk-who-growth-charts-childhood-puberty-close-monitoring-cpcm-chart
- 85.da Rocha AF, Leite C da C, Rocha FT, Massad E, Cerri GG, Angelotti SA de O, et al. Mental retardation: a MRI study of 146 Brazilian children. Vol. 64, Arquivos de Neuro-Psiquiatria. scielo; 2006. p. 186–92. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.