Highlights
-
•
Prostheses result in lower pain than osteosyntheses in pathological hip fractures.
-
•
Surgeons in sarcoma centers generally use prostheses for pathological hip fractures.
-
•
Both methods use similar healthcare resources and effectively restore ambulation.
Keywords: Pathological, Hip, Fracture, Surgery, Prosthesis, Osteosynthesis, Pain, Function
Abstract
Aims
How endoprosthetic replacement compares to osteosynthesis in the treatment of pathologic hip fractures as far as functional outcome and use of healthcare resources is concerned remains largely unknown. We aimed to investigate this in a nationwide registry.
Methods
We analyzed the functional outcome after surgery for a pathological fracture of the hip in terms of post-operative pain and ambulatory capacity. The preferred surgical method depending on the level of the treating unit was also examined. Furthermore, we documented the length of hospital stay and the patterns of discharge and compared them between these two methods.
Results
Patients operated with an endoprosthesis reported significantly lower pain at follow-up. Both methods (endoprosthetic replacement and osteosynthesis) were equally effective in restoring the ambulatory capacity and demanded a similar length of stay in hospital. Orthopaedic surgeons working in hospitals with dedicated sarcoma teams were more likely to use a prosthesis rather than osteosynthesis, when compared to surgeons working at other university hospitals or emergency hospitals.
Conclusion
Endoprosthetic replacement results in a better functional outcome in terms of post-operative pain without consuming more healthcare resources. Orthopaedic surgeons working in hospitals with sarcoma centers are more likely to use prostheses as compared to surgeons working at hospitals where dedicated musculoskeletal oncology teams are not available.
1. Introduction
The most frequent site for symptomatic metastatic bone disease (MBD) of the appendicular skeleton is the proximal femur and hip. A pathological hip fracture is by rule treated surgically, in order to restore the patient’s ambulatory capacity and reduce pain[1]. There are two principal treatment methods for a pathological hip fracture: osteosynthesis and endoprosthetic reconstruction (hip replacement surgery). The former relies on mechanical fixation of the bone fragments with an implant such as an intramedullary rod, pins/screws or a plate-and-screw design. The latter entails resection of the humeral head and possibly other parts of the bone involved by the tumor, and replacement with a prosthesis that is usually attached to the remaining femur with bone cement.
Prostheses have been associated with lower risk for revision surgery to implant failure, since they are more able to withstand the mechanical loads over time[2], [3], [4], [5]. Osteosynthesis relies on implants designed for conventional, traumatic fractures, which normally heal over time. Pathological fractures on the other hand rarely heal, since the local invasion by tumor cells inhibits the bone healing process[6]. Many authorities thus recommend the preferential use of prostheses in cases of pathological hip fractures, although others have questioned these findings[7], [8], [9], [10]. However, other important parameters regarding the outcome of surgery, such as the functional outcome of the patient and the use of healthcare resources, have not been studied to the same extent as implant failure rate when comparing different treatment methods. These parameters should also be considered in the treatment decision since they affect the patients’ quality of life and the sustainability of the healthcare system in view of the increasing burden of MBD[11].
To answer these questions, we conducted a nationwide registry study to investigate the outcome of surgical treatment for pathological fractures of the hip and analyzed the functional outcome of surgery and the use of healthcare resources. The focus was whether endoprosthetic replacement is superior to osteosynthesis in these aspects. Furthermore, we explored the patterns of surgical treatment in hospitals of different levels (tertiary sarcoma/musculoskeletal cancer centers, university hospitals and emergency hospitals).
2. Patients and methods
Data for this nationwide cohort study were extracted from the Swedish Registry for Hip Fracture Patients and Treatment (RIKSHÖFT). 47 of the 52 orthopaedic clinics in Sweden report voluntarily to RIKSHÖFT and the coverage rate exceeded 80% during the years 2014–2018. Data is collected by nurses or contact secretaries, who transfer data into a web-based system (Comportosystem) at operation and at follow-up 4 months after surgery. Information regarding date of death was transferred from Statistics Sweden using the personal identification number assigned to all individuals living in Sweden. The study to the Helsinki Declaration and was approved by the Regional Ethics Committee of Stockholm (DNr: 2017/1088–31).
2.1. Inclusion and exclusion criteria
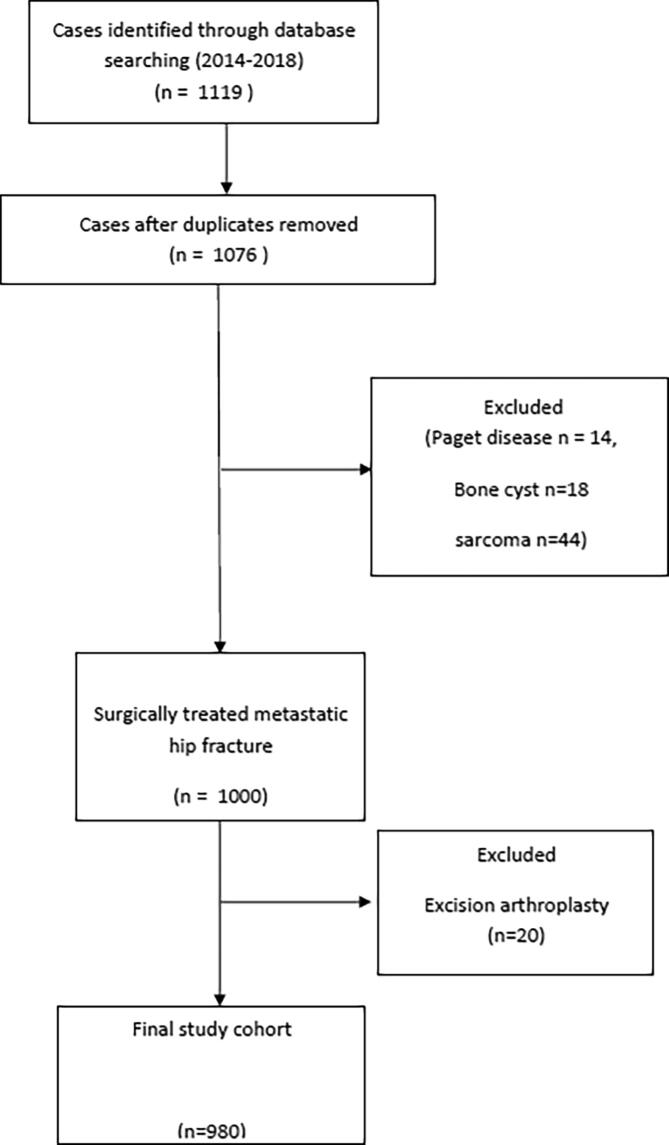
The flowchart of the study cohort is shown in Fig. 1. Patients with pathological hip fracture due to metastasis admitted to hospital between the 1st of January 2014 and the 31st of December 2018 were included. Patients with primary sarcoma, bone cyst or Paget's disease were excluded to create a homogeneous study material. Double treatment cases were also excluded.
Fig. 1.
Flowchart analysis of the cases included in the study.
2.2. Recorded variables and sub-group analysis
Relevant recorded variables were: gender, age at surgery (years), living condition prior to hospital admission (living in own home, hospice/palliative care or other hospital),type of fracture (sub-grouped in: cervical, intertrochanteric and subtrochanteric) and surgical method used (sub-grouped in: hemiarthroplasty, total hip replacement, osteosynthesis with pins/screws, osteosynthesis with plate/screws or sliding hip screw and osteosynthesis with intramedullary rod), treating hospital (sub-grouped in: university hospital with dedicated sarcoma center, referred also as sarcoma centers, other university hospitals and emergency hospitals), ASA grade prior to surgery as an index of comorbidity, time from admittance to surgery (in hours), length of hospital stay (days) and pattern of discharge (to home, hospice/palliative care, other hospital), reported pain (sub-grouped in: severe, moderate/activity and minor/none) and ambulatory capacity (independent outdoors, assisted outdoors, independent indoors, assisted indoors) at 4-month follow up, death and death date.
2.3. Statistics
Statistical calculations were performed in SPSS 25. Descriptive statistics are presented with number(s), proportions (%), range and median or mean values with standard deviations. Bars represent 95% confidence intervals. Comparisons of categorical data were done with the chi2 test. Survival analysis was done using the Kaplan – Meier method, with the log-rank test to evaluate differences between groups. Mean patient survival is presented in months with 95% confidence intervals shown in parentheses. A p-value below 0.05 was defined as statistically significant.
3. Results
3.1. Oncological characteristics of the cohort
The cohort consisted of 980 patients and its main characteristics are presented in Table 1. 104 patients were operated at hospitals with dedicated sarcoma teams, 150 in other university-level hospitals and 726 in emergency hospitals.
Table 1.
Description of the study cohort.
| Number of patients | Total | Prosthesis | Osteosynthesis |
|---|---|---|---|
| 980 | 508 | 472 | |
| Gender | P = 0.098 | ||
| Men/Women | 485/495 | 262/246 | 223/249 |
| Age | P = 0.062 | ||
| Median/Mean Range |
78/77 32–104 |
76/77 32–104 |
77/79 32–100 |
| Type of fracture | P < 0.001 | ||
| Cervical, non-displaced | 91 | 37 | 54 |
| Cervical, displaced | 432 | 395 | 37 |
| Basocervical | 38 | 17 | 21 |
| Intertrochanteric, 2-part | 134 | 20 | 114 |
| Intertrochanteric, multifragmentary | 91 | 11 | 80 |
| Subtrochanteric | 194 | 28 | 166 |
| Admitted from | P < 0.001 | ||
| Home | 708 | 352 | 356 |
| Nursing home/hospice | 125 | 57 | 76 |
| Emergency hospital | 131 | 96 | 35 |
| Other | 6 | 2 | 4 |
| Missing | 2 | ||
| Walking aids prior to fracture | P = 0.267 | ||
| Independent | 367 | 188 | 179 |
| Walking stick/cane | 155 | 85 | 70 |
| Walking frame/trolley | 372 | 199 | 173 |
| Wheelchair/bedridden | 65 | 26 | 39 |
| Missing | 21 | ||
| Discharged to | P = 0.065 | ||
| Home | 399 | 209 | 190 |
| Nursing home/hospice | 348 | 170 | 178 |
| Other hospital | 178 | 104 | 74 |
| Dead | 49 | 22 | 27 |
| Other | 5 | 2 | 3 |
| Missing | 2 | ||
| Status at last follow-up | P = 0.085 | ||
| Dead | 672 | 363 | 309 |
| Alive | 308 | 145 | 163 |
Patients operated in sarcoma centers had higher comorbidity grade (p = 0.024), since 82% were ASA 3 and 4 class, as compared to 66% of patients in other university-level hospitals and 70% of patients in emergency hospitals. Patients operated in sarcoma centers also had inferior oncologic outcome (p = 0.005), since their overall survival was only 16(12–20) months, as compared to the ones operated in other university hospitals and emergency hospitals, who had an overall survival of 21(17–26) months and 25(23–27) months respectively. Mean time from hospital admittance to surgery differed also among healthcare providers, with sarcoma centers and other university hospitals having a longer time from fracture to surgery (44 and 41 h respectively) as compared to other emergency hospitals (32 h) (p = 0.005).
3.2. Patterns of treatment of pathological hip fractures
Osteosynthesis was performed in 472 patients, in 85 of them with pins/screws, in 96 with plate and screws and in 291 with intramedullary rods. Endoprosthetic replacement was performed in 508 patients (hemiarthroplasty in 295 and total hip replacement in 213). Patients treated at sarcoma centers were more likely to be operated with a prosthesis rather than osteosynthesis (Table 2a). When data were separately analyzed for the 3 main types of pathological hip fractures (cervical, intertrochanteric and subtrochanteric), it became evident that surgeons working in sarcoma centers were more likely to use a prosthesis even for intertrochanteric and subtrochanteric fractures. The pattern of surgical treatment between university hospitals and other emergency hospitals was similar (Table 2b).
Table 2a.
Patterns of surgical treatment of pathological hip fractures in different hospitals across Sweden.
| Hospital level | Prosthesis | Osteosynthesis | P < 0.001 |
|---|---|---|---|
| Sarcoma Center | 86 | 19 | |
| University Hospital | 70 | 80 | |
| Emergency Hospital | 353 | 373 | |
| Total | 508 | 472 |
Table 2b.
Patterns of surgical treatment of pathological hip fractures depending on the anatomical location.
| Sarcoma Centers | |||
|---|---|---|---|
| Prosthesis | Osteosynthesis | P < 0.001 | |
| Cervical fracture | 55 | 1 | |
| Trochanteric fracture | 14 | 4 | |
| Subtrochanteric fracture | 16 | 14 | |
| Total | 85 | 19 | |
| University Hospitals and Emergency Hospitals | |||
| Prosthesis | Osteosynthesis | ||
| Cervical fracture | 377 | 90 | |
| Trochanteric fracture | 34 | 211 | |
| Subtrochanteric fracture | 12 | 152 | |
| Total | 423 | 453 | |
3.3. Correlation of treatment method with the functional outcome
The functional outcome was assessed 4 months after surgery, and both the pain levels as well as the patients’ ambulatory capacity were reported (Table 3). Data were available for 272 patients since there were not any recorded data for 249 patients and 359 patients were dead at this time-point. Patients operated with a prosthesis reported significantly lower pain than patients operated with osteosynthesis (p = 0.004) (Table 3).
Table 3.
Functional status of the patients 4 months after surgical treatment.
| Reported pain | Prosthesis | Osteosynthesis | P = 0.004 |
|---|---|---|---|
| Severe | 6 | 10 | |
| Moderate/activity-correlated | 43 | 63 | |
| Minor/none | 134 | 94 | |
| Unable to answer | 14 | 8 | |
| Total | 197 | 175 | |
| Ambulatory capacity | P = 0.928 | ||
| Independent outdoors | 100 | 83 | |
| Assisted, outdoors | 22 | 18 | |
| Independent, indoors | 35 | 34 | |
| Assisted, indoors | 21 | 19 | |
| Non-ambulatory | 19 | 21 | |
| Total | 197 | 175 | |
| Walking aids | P = 0.853 | ||
| None | 55 | 44 | |
| Walking stick/cane | 33 | 26 | |
| Walking frame/trolley | 88 | 80 | |
| Wheelchair/bed-ridden | 21 | 25 | |
| Total | 197 | 175 | |
After subgroup analysis for the 3 principal fracture patterns (cervical, intertrochanteric and subtrochanteric), this effect was attributed to the lower level of reported pain of patients with cervical fractures operated with a prosthesis, as compared to the ones operated with pins/screws (p = 0.004). The difference in reported pain among patients with intertrochanteric and subtrochanteric fractures, who were operated with either a prosthesis or with osteosynthesis, did not reach statistical significance (p = 0.800 and p = 0.371 for intertrochanteric and subtrochanteric fractures respectively).
In the subgroup of patients operated with a prosthesis, pain 4 months after surgery did not differ significantly between the ones who had a total hip arthroplasty and the ones who had a hemiarthroplasty (p = 0.421). In the subgroup of patients operated with osteosynthesis, reported pain was similar among patients who underwent fixation of the fracture with a dynamic screw and plate construct, as compared to the ones operated with pins/screws or intramedullary nails (p = 0.054).
Regarding ambulation, both treatment methods (prosthesis and osteosynthesis) were equally efficient in restoring the ambulatory capacity, as shown in Table 3 (p = 0.928). As shown in the same Table, there was no significant difference in the use of walking aids between the two principal groups at follow-up (p = 0.853).
3.4. Correlation of treatment methods to the use of healthcare resources
Patients were admitted to hospital for a mean of 7 days (median 6, range 1–58). The time period of the patient remaining in hospital was similar between patients operated with a prosthesis and the ones operated with osteosynthesis (p = 0.497), as well as between levels of the treating units (sarcoma centers, university hospitals, emergency hospitals) (p = 0.942). Patients previously living in their own home had similar mean length of stay in hospital (7 ± 13 days) as the ones coming from hospice/nursery homes (6 ± 3 days) and the ones already admitted to hospital (7 ± 6 days).
Most patients were discharged to their own home: 53% of patients operated with a prosthesis and 49% of patients operated with osteosynthesis could be discharged back to their home, irrespective of treatment method and treatment center. At follow-up, 4 months after surgery, there was no significant difference between groups regarding the dwelling condition of the patients (p = 0.903).
4. Discussion
The principal finding of this nationwide registry study is that the use of endoprosthetic devices for the surgical treatment of pathological hip fracture is associated with a superior functional outcome in terms of pain alleviation as compared to osteosynthesis. This complements previous knowledge that prostheses have lower risk of failure, which was considered the primary reason why they were recommended as the implants of choice in the setting of pathological fracture surgery[2], [3], [5]. Prostheses are implants primarily used in the surgical replacement of degenerate joints and thus designed to function as load-bearing devices for long time periods, that exceed by far the expected survival of a patient with MBD[12]. Their longevity is thus not surprising, and their main mode of failure is the failure of the remaining bone stock due to tumor progression. Their superiority in terms of pain relief can possibly be attributed to the fact that they allow for a more stable reconstruction than osteosynthesis. The latter usually allows for some movement between fracture fragments, which is considered beneficial in the context of traumatic fractures, since it promotes bone healing[13]. In MBD, where the implant is only stabilizes the fracture and no significant healing is expected, this may prove a source of pain for the patient.
There is a very limited number of previous studies addressing the functional outcome of patients operated for pathological hips fractures: Guzik reported superior result in terms of pain relief in patients operated with a prosthesis, as compared to osteosynthesis, in a cohort of 122 patients, whereas Harvey et al and Meynard et al reported similar functional outcome in cohorts of 158 and 299 patients respectively[5], [14]. Our data, from a comparatively large cohort with standardized follow-up, strongly support the superiority of endoprosthetic replacement in terms of pain relief. Regarding restoration of the ambulatory capacity the methods were directly comparable, corroborating the findings presented by Maynard et al.
The difference in functional outcome between osteosynthesis implants is probably the result of selection bias: it is likely that dynamic screw and plate devices were used in more stable, less displaced fractures, whereas intramedullary nails in unstable ones[15]. Pin/screw fixation usually results in poor biomechanical stability in MBD, whatever the fracture pattern. In our study functional results between hemiarthroplasty and total hip replacement were comparable, supporting the view that in MBD, where short-term functional results are of importance considering the short patient survival, the use of hemiarthroplasty rather than total hip replacement is preferable in the majority of patients since it is associated with a lower risk for dislocation and shorter operative time[16], [17]. This is contrary to the traumatic hip fracture scenario, where total hip arthroplasty is associated with better functional outcome[18]. Prognostication tools allow for choice of patients with MBD who are expected to have longer survival and thus benefit from total hip arthroplasty[19], [20].
We acknowledge that our work has significant limitations, being a registry study, where data have inherent treatment bias or may be lacking for several patients or even incorporate errors during registration. Furthermore, a major shortcoming of the present dataset is that primary diagnosis is unknown, and this precludes analysis particular to each cancer type. Moreover, megaprostheses were not specifically coded in the dataset. Given these limitations, another principal observation in the present study is the compliance of healthcare providers to the generally accepted between orthopaedic oncology surgeons in Sweden recommendation of using endoprostheses rather than performing osteosynthesis in pathological hip fractures. A previous study in a international group of orthopaedic oncologists has highlighted the variation in the choice of surgical approach[21]. Our national registry data, from a country with a comparatively small population and a general consensus in treatment protocols between orthopaedic oncology surgeons, in addition show that the latter comply better than orthopaedic surgeons at university or emergency hospitals. The limited penetration of this knowledge among orthopaedic surgeons other than the ones working in centers routinely treating patients with MBD raises considerations regarding the way this information is conveyed to the orthopaedic surgeon community. It is also noteworthy that surgeons in sarcoma centers abide by this recommendation even though they apparently treat patients who are more frail and/or have more extensive disease, as shown by the comorbidity grading and overall survival, where a general orthopaedic surgeon may be even more tempted to restrain from hip replacement in order to avoid more extensive surgery and the use of bone cement. A potential pitfall in this deduction is that we are not aware of the technical difficulty of the cases treated in each hospital level and cannot exclude that surgically demanding cases with major loss of bone stock, thus not amenable to osteosynthesis, are further admitted to hospitals with dedicated orthopaedic oncologists. Differences in the time to surgery may reflect, apart from the availability of healthcare resources and the differential time to optimize each patient for surgery, the need to transport demanding cases to higher-level care.
We did not observe any significant differences in the use of healthcare resources or efficacy of return to community between the two treatment groups. Both methods resulted in equivalent hospital stay and comparable discharge patterns as well as status of social care at follow-up. We did not take implant costs into account since these differ significantly between manufacturers and institutions around the world. Noticeably, the mean period of hospital stay of one week is quite short compared to non-pathological fractures, and probably reflects the effective pathway of referral of these patients back to palliative care[22].
Our study strongly supports the use of endoprosthetic replacement instead of osteosynthesis in MBD of the hip, since it results in a less painful extremity without requiring additional health resources, a finding which complements the superiority of endoprosthetic replacement in terms of risk for implant failure and need of revision surgery. This recommendation appears to be preferentially implemented by specialized orthopaedic oncology surgeons and has not been adopted by general orthopaedic surgeons not routinely treating MBD.
CRediT authorship contribution statement
Panagiotis Tsagkozis: Conceptualization, Methodology, Formal analysis, Writing - original draft, Writing - review & editing. Jessica Ehne: Conceptualization, Formal analysis, Writing - review & editing. Rikard Wedin: Methodology, Validation, Writing - review & editing. Margareta Hedström: Resources, Supervision, Project administration, Funding acquisition, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Coleman R.E. Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res Off J Am Assoc Cancer Res. 2006;12(20):6243s–6249s. doi: 10.1158/1078-0432.CCR-06-0931. [DOI] [PubMed] [Google Scholar]
- 2.Wedin R., Bauer H.C.F. Surgical treatment of skeletal metastatic lesions of the proximal femur: endoprosthesis or reconstruction nail? J Bone Joint Surg Br. 2005;87-B(12):1653–1657. doi: 10.1302/0301-620X.87B12.16629. [DOI] [PubMed] [Google Scholar]
- 3.Steensma M., Boland P.J., Morris C.D., Athanasian E., Healey J.H. Endoprosthetic treatment is more durable for pathologic proximal femur fractures. Clin Orthop. 2012;470(3):920–926. doi: 10.1007/s11999-011-2047-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.M.S. Sørensen P.F. Horstmann K. Hindsø M.M. Petersen 19 2019 100264 10.1016/j.jbo.2019.100264 [DOI] [PMC free article] [PubMed]
- 5.Harvey N., Ahlmann E.R., Allison D.C., Wang L., Menendez L.R. Endoprostheses last longer than intramedullary devices in proximal femur metastases. Clin Orthop. 2012;470(3):684–691. doi: 10.1007/s11999-011-2038-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.S. D’Oronzo R. Coleman J. Brown F. Silvestris Metastatic bone disease: Pathogenesis and therapeutic options: Up-date on bone metastasis management J Bone Oncol 15 2019 004 004 [DOI] [PMC free article] [PubMed]
- 7.Janssen S.J., Kortlever J.T.P., Ready J.E., Raskin K.A., Ferrone M.L., Hornicek F.J., Lozano-Calderon S.A., Schwab J.H. Complications After Surgical Management of Proximal Femoral Metastasis: A Retrospective Study of 417 Patients. J Am Acad Orthop Surg. 2016;24(7):483–494. doi: 10.5435/JAAOS-D-16-00043. [DOI] [PubMed] [Google Scholar]
- 8.Meynard P., Seguineau A., Laumonerie P., Fabre T., Foltran D., Niglis L., Descamps J., Bouthors C., Lebaron M., Szymanski C., Sailhan F., Bonnevialle P. Surgical management of proximal femoral metastasis: Fixation or hip replacement? A 309 case series. Orthop Traumatol Surg Res OTSR. 2020;106(6):1013–1023. doi: 10.1016/j.otsr.2020.05.007. [DOI] [PubMed] [Google Scholar]
- 9.Janssen S.J., Teunis T., Hornicek F.J., van Dijk C.N., Bramer J.A.M., Schwab J.H. Outcome after fixation of metastatic proximal femoral fractures: A systematic review of 40 studies. J Surg Oncol. 2016;114(4):507–519. doi: 10.1002/jso.24345. [DOI] [PubMed] [Google Scholar]
- 10.Di Martino A., Martinelli N., Loppini M., Piccioli A., Denaro V. Is endoprosthesis safer than internal fixation for metastatic disease of the proximal femur? A systematic review. Injury. 2017;48(Suppl 3):S48–S54. doi: 10.1016/S0020-1383(17)30658-7. [DOI] [PubMed] [Google Scholar]
- 11.Schulman K.L., Kohles J. Economic burden of metastatic bone disease in the U.S. Cancer. 2007;109(11):2334–2342. doi: 10.1002/cncr.22678. [DOI] [PubMed] [Google Scholar]
- 12.Junnila M., Laaksonen I., Eskelinen A., Pulkkinen P., Ivar Havelin L., Furnes O., Marie Fenstad A., Pedersen A.B., Overgaard S., Kärrholm J., Garellick G., Malchau H., Mäkelä K.T. Implant survival of the most common cemented total hip devices from the Nordic Arthroplasty Register Association database. Acta Orthop. 2016;87(6):546–553. doi: 10.1080/17453674.2016.1222804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Einhorn T.A., Gerstenfeld L.C. Fracture healing: mechanisms and interventions. Nat Rev Rheumatol. 2015;11(1):45–54. doi: 10.1038/nrrheum.2014.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guzik G. Oncological and functional results after surgical treatment of bone metastases at the proximal femur. BMC Surg. 2018;18(1):5. doi: 10.1186/s12893-018-0336-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Curtis M.J., Jinnah R.H., Wilson V., Cunningham B.W. Proximal femoral fractures: a biomechanical study to compare intramedullary and extramedullary fixation. Injury. 1994;25(2):99–104. doi: 10.1016/0020-1383(94)90111-2. [DOI] [PubMed] [Google Scholar]
- 16.Varady N.H., Ameen B.T., Hayden B.L., Yeung C.M., Schwab P.-E., Chen A.F. Short-Term Morbidity and Mortality After Hemiarthroplasty and Total Hip Arthroplasty for Pathologic Proximal Femur Fractures. J Arthroplasty. 2019;34(11):2698–2703. doi: 10.1016/j.arth.2019.06.019. [DOI] [PubMed] [Google Scholar]
- 17.Ogawa T., Yoshii T., Moriwaki M., Morishita S., Oh Y., Miyatake K., Nazarian A., Shiba K., Okawa A., Fushimi K., Fujiwara T. Association between Hemiarthroplasty vs Total Hip Arthroplasty and Major Surgical Complications among Patients with Femoral Neck Fracture. J Clin Med. 2020;9(10):3203. doi: 10.3390/jcm9103203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blomfeldt R., Törnkvist H., Eriksson K., Söderqvist A., Ponzer S., Tidermark J. A randomised controlled trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. J Bone Joint Surg Br. 2007;89-B(2):160–165. doi: 10.1302/0301-620X.89B2.18576. [DOI] [PubMed] [Google Scholar]
- 19.Forsberg J.A., Eberhardt J., Boland P.J., Wedin R., Healey J.H., El-Deiry W.S. Estimating survival in patients with operable skeletal metastases: an application of a bayesian belief network. PloS One. 2011;6(5):e19956. doi: 10.1371/journal.pone.0019956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson A.B., Wedin R., Fabbri N., Boland P., Healey J., Forsberg J.A. External Validation of PATHFx Version 3.0 in Patients Treated Surgically and Nonsurgically for Symptomatic Skeletal Metastases. Clin Orthop. 2020;478(4):808–818. doi: 10.1097/CORR.0000000000001081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Steensma M., Healey J.H. Trends in the surgical treatment of pathologic proximal femur fractures among Musculoskeletal Tumor Society members. Clin Orthop. 2013;471(6):2000–2006. doi: 10.1007/s11999-012-2724-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.P. Nordstrom Y. Gustafson K. Michaelsson A. Nordstrom Length of hospital stay after hip fracture and short term risk of death after discharge: a total cohort study in Sweden BMJ 350 feb20 1 2015 h696 h696 [DOI] [PMC free article] [PubMed]