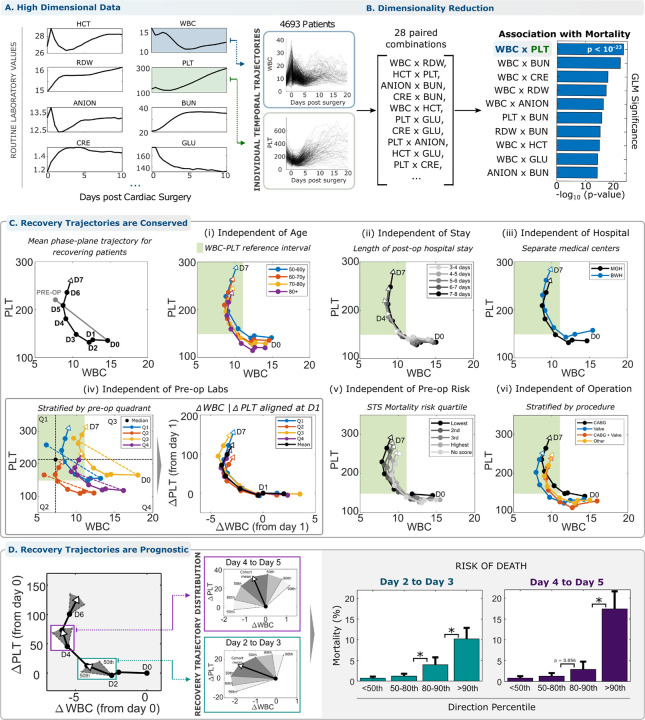
Figure 1 – Reduced -dimension analysis of acute inflammatory response in the WBC-PLT phase plane reveals a consistent shape of recovery.
(A) High dimensional trajectories of cellular and serum markers following cardiac surgery are associated with patient outcome. (B) Reducing dimensionality of trajectories retains significant association with patient outcome. The WBC-PLT phase plane retains high association consistent with understanding of inflammatory response mechanisms. (C) The average patient with a good recovery (surviving with LOS < 14 days) follows a WBC-PLT trajectory that departs from both WBC and PLT reference intervals (green region) and returns toward the pre-operative baseline over about 5 days. This shape of a good inflammatory recovery persists independent of (i) patient age, (ii) length of hospital stay, (iii) hospital of service, (iv) baseline patient WBC-PLT, (v) pre-op risk defined by the Society of Thoracic Surgeons risk score30,31, (vi) cardiac surgery sub-type, patient gender, year of surgery, and general pre-op risk. (See supplemental materials 1.5). (D) Deviation from the mean recovery trajectory is prognostic for adverse outcomes. The mean trajectory along with the 50th, 80th and 90th percentiles for daily directional changes are shown. Deviation from the direction of the mean trajectory is associated with significant (*, p<0.05) increased risk of death, 14x (CI 8.0–24.1, 0.7% to 10.2%) on day 3 after surgery and 22x (CI: 11.7–39.8, 0.8% to 17.4%) on day 5, between patients below the 50th and above the 90th percentiles. Percentile thresholds were calculated in the exploratory cohort, and outcome rates from the validation cohort. The identification of WBC x PLT as the optimal 2D pair was performed solely using the exploratory cohort. Circles in panels (D) denote 1-day time intervals, or from pre-op to immediately post-op.