Abstract
Aim
To evaluate mothers’ satisfaction with childbirth experience in a cohort of women who delivered during COVID pandemia and to compare them to a pre‐COVID cohort.
Design
We performed a cross‐sectional study in a low‐risk Maternity Unit.
Methods
Women who delivered during COVID‐19 pandemic were compared to a pre‐COVID cohort recruited in 2018 in the same setting. Italian version of the Birth Satisfaction Scale‐Revised (I‐BSS‐R) was used.
Results
Three hundred and seventy‐seven women were included (277 pre‐COVID and 100 during COVID pandemic). No differences in terms of satisfaction at birth were reported (I‐BSS‐R mean 27.0, SD 5.3 versus mean 27.6, SD 6.1, p 0.34), despite an increased rate of active intrapartum interventions. Intrapartum variables that significantly reduced satisfaction were the same in the two groups: epidural analgesia (p < .0001 in both groups), prolonged active phases (p < .0001 in both), oxytocin administration (p < .0001 in both) and operative delivery (p 0.0009 versus p 0.0019).
Keywords: childbirth experience, COVID‐19, intrapartum intervention
1. INTRODUCTION
Women's satisfaction with their childbirth experience has short and long‐term consequences for women and babies' health, in terms of a future good relationship with the newborn. Both the 2016 World Health Organization's (WHO) guidelines for antenatal and 2018 guidelines for intrapartum care highlight the importance for women of having a positive childbirth experience.
Thus, maternal satisfaction with birth has become a contemporary area of research and is now considered one of the most relevant indicators in the evaluation of the quality of maternity services.
Defining “satisfaction with childbirth experience” is complex in meaning and includes a multifaceted collage of components. In 2011, Hollins Martin and Fleming (Hollins Martin & Fleming, 2011 did the first attempt to develop a measuring tool, based on the evidence of previous studies (Green, 1993; Hodnett, 2002; Waldenstrom and Nilsson, 1993).
Since satisfaction with childbirth is not an object or a practical tool (as stated by Hollins Martin), it is acknowledged that women will have different perceptions of what comprises a rewarding birth experience. It can be summarized as satisfaction in three main fields: quality of care perceived, women personal attribute and stress experienced.
This process can also influence the attitude toward motherhood that contributes to the woman's sense of competence and confidence (Hinic, 2017; Karlström et al., 2015; Larkin et al., 2009).
The recent epidemic from a new coronavirus isolated in Wuhan (China) at the end of 2019 (SARS‐CoV‐2), among other clinical and public health problems, also raised those issues related to the perception of labour and birth, in relation to the preventative measures in pregnancy/labour/birth, the possible maternal‐infant transmission of the infection, the safety of the management of the mother‐neonate and breastfeeding. After entering Italy, SARS‐CoV‐2 spread fast. The region that was mostly hit was Lombardy, in the North (Narang et al., 2020; Odone et al., 2020).
2. BACKGROUND
In 2018, two years before the spreading of the infection, we performed a cross‐sectional study involving 277 women who delivered in a low‐risk maternity unit in Northern Italy (Fumagalli et al., 2020). Satisfaction with birth was measured using the Italian version of the Birth Satisfaction Scale‐Revised (I‐BSS‐R). The BSS‐R is a validated 10 items, a self‐report scale that was developed in the UK to evaluate women's satisfaction with birth starting from the original Birth Satisfaction Scale of 30 items (Hollins Martin & Martin, 2014). The Italian version of the BSS‐R has been recently developed following an extensive translation process (Nespoli et al., 2020). Our theoretical definition for satisfaction with the childbirth experience is based on Hollins Martin's quantitative 'Birth Satisfaction Scale scores'. Her epistemological stance formed the basis for our theoretical framework. The BSS‐R seemed to be a comprehensive, reliable and efficient tool, with multidimensional and psychometric characteristics able to evaluate maternal satisfaction with birth, considering themes which take into account also the subjective perception of the quality of the care received.
We showed that intrapartum interventions were negatively associated with maternal outcomes and, therefore, also with maternal satisfaction at birth. Variables significantly associated with the I‐BSS‐R total score affected the three Sub‐Scales (Quality of Care [QC], Women personal Attribute [WA] and Stress Experienced [SE]) differently. For example, multi‐parity, antenatal class attendance and intact perineum variables were significantly associated only with the SE Sub‐Scale and were not involved with the other two Sub‐Scales. Epidural analgesia, oxytocin administration and the active phase of labour being greater than 12 hr were significantly associated with both the SE and WA Sub‐Scales and not with the QC Sub‐Scale.
Recent studies reported that women's expectations and concerns regarding childbirth changed significantly as a result of the COVID‐19 pandemic in Italy (Ravaldi et al., 2020). Women needed particular attention as they seem to experience higher levels of concern. The aim of this study was to compare mothers’ satisfaction with childbirth experience and changes in intrapartum care in a cohort of women who delivered during COVID‐19 pandemic to a pre‐COVID cohort of 2018 in the same setting and in relation to socio‐demographic characteristics, obstetric history and obstetric care variables. Specifically, we first hypothesized to find lower levels of satisfaction with childbirth during COVID pandemia compared to the pre‐COVID setting, due to the increased level of stress experienced by women (which is one of the three domains of the BSS‐R) caused by the emergency.
Secondly, we hypothesized to find differences in our intrapartum practice, in particular, we expected to find a higher rate of active interventions and a lower quality of midwives' assistance (rate of one‐to‐one assistance, mobility during labour, intermittent auscultation of the Fetal Cardiac Frequency) due to the emergency context.
Third, we hypothesized that those variables that impacted negatively on childbirth satisfaction before COVID pandemia (in particular, epidural analgesia, prolonged active phases >12 hr, oxytocin administration and operative delivery) could impact negatively also during the pandemia.
3. MATERIAL AND METHODS
3.1. Design
We performed a cross‐sectional study in a low‐risk Maternity Unit in Lombardy, Northern Italy.
3.2. Method
The study was conducted in a Level I Maternity Hospital in Northern Italy. The research site has approximately 1,300 births per year and one of the lowest rates of caesarean section in Italy. The overall caesarean section (CS) rate is 15.9% (compared with the national CS rate of 35.4%), of which 5% are primary CS that are performed on women giving birth for the first time.
In the hospital's labour ward there are four rooms, where women remain for 2 hr following birth, before being transferred to the postnatal ward, where there are twenty‐six beds. Usually, women following a vaginal birth are discharged after 72 hr. During COVID pandemic, the length of stay was reduced to 48 hr for those who had a vaginal birth without any complications, to minimize the time spent in the hospital. Discharge after a caesarean section was maintained after 72 hr. Midwifery care was provided in both labour and postnatal wards.
There were 23 midwives working on the labour ward, three midwives per shift with a mean number of four births per day (planned CS are included in this number).
The research site was committed to offer a one‐midwife‐to‐one‐woman ratio for all women in labour.
COVID‐19 pandemic raised the need for a deep reorganization in order to guarantee the safety of mothers, neonates, and healthcare providers. Practice changes were implemented in response to COVID‐19 to provide for mother/partner testing, management of positive cases, partner presence, and requirements for personal protective equipment (Table S1). The adoption of these labour and delivery management measures was shared with the Italian Superior Institute for Health, which at that time elaborated its guidelines.
Participants were recruited through a consecutive mode, from 25 March 2020 to 18 May 2020, which corresponded to the new Ministerial decree for communicating less restrictive measures due to the drop of cases. Exclusion criteria were COVID symptoms or positive swab and the predefined criteria used in the pre‐COVID cohort (language barrier, women who did not consent to the study, pre‐term [<37 weeks] or post‐term [>42 weeks] birth, previous CS, pre‐labour caesarean section, pre‐existing severe medical conditions or pregnancy complications [such as cardiac disease, haemoglobinopathies, renal disease, neurological disease, pre‐eclampsia or complications), new‐borns in poor condition at birth or who required any form of resuscitation.
At least 24 hr after delivery, women who met the inclusion criteria were invited to take part in the study by one of the four researchers involved in the recruitment, who explained to them the aim of the study, their involvement and asked them to sign the consent form. The researcher who recruited the woman was never the one who provided maternity care, since reports of dissatisfaction may be inhibited. Women were enrolled every day of the week. Surveys were completed by mothers alone and returned before discharge.
Data were collected through the Italian version of the Birth Satisfaction Scale‐Revised (I‐BSS‐R).
Participants’ perceptions were measured using a series of simple statements with a five‐point Likert scale. Four of the items are reverse‐coded (e.g. ‘I found giving birth a distressing experience’). Three main themes that affect birth satisfaction are assessed throughout three Sub‐Scales: quality of care provision–QC–(four items involving helping women to feel in charge of the labour, birth environment, support and relationships with health care professionals), women's personal attributes–WA–(two items concerning the ability to cope during labour, feeling in control, childbirth preparation and relationship with the baby) and stress experienced during labour–SE–(four items related to distress, obstetric injuries, receiving sufficient care, obstetric interventions, pain, long labour and baby's health). Socio‐demographic, obstetric and intrapartum data (gestational age, onset of labour, pain relief used, oxytocin augmentation, length of active phase >12 hr, method of fetal heart rate monitoring, mobilization, continuity of midwifery care, mode of birth and perineum outcome), were available from the birth register and the electronic records.
3.3. Analysis
Continuous variables were described by mean and standard deviation and categorical variables by percentages. Descriptive statistics was performed on the whole sample, separately for each cohort and within each subcohort on subsamples defined by classification variables. Comparisons between distributions of continuous and categorical distributions were obtained by hypothesis testing across cohorts and within each cohort. T‐test and Chi‐square test were used for continuous and categorical variables respectively. p‐values were two‐sided. Data management and statistical analysis were carried out by Stata software version 16.
3.4. Ethics
Ethical approval was obtained from the hospitals’ Ethical Review Board (Approval number: 37/2018) and amended in 2020 for the second part of the study. Written informed consent was gained from all the participants.
4. RESULTS
4.1. Socio‐demographic characteristics and obstetric history
Among 158 women who gave birth during the study period, 27 (17%) did not receive the questionnaire, one woman did not consent to participate, 15 (9.4%) were not recruited for the language barrier and 15 (9.4%) underwent pre‐labour CS. There were 2 out of 158 (1.26%) women who resulted in COVID 19 positive and since they were transferred to the HUB centre immediately after birth, they were counted in the 27 (17%) that did not receive the questionnaire. Thus, the study group (COVID) comprised 100 women (Figure 1) who were compared to a cohort of 277 women (pre‐COVID) recruited in a previous study performed in 2018 in the same setting (Fumagalli et al., 2020), for a total of 377 women. Socio‐demographic characteristics and obstetric history are reported in Table 1. No differences were reported in terms of maternal age, education, rate of employment, ethnicity and parity. The lack of confounders justified to proceed with the subsequent comparison of satisfaction of birth between the two groups.
FIGURE 1.
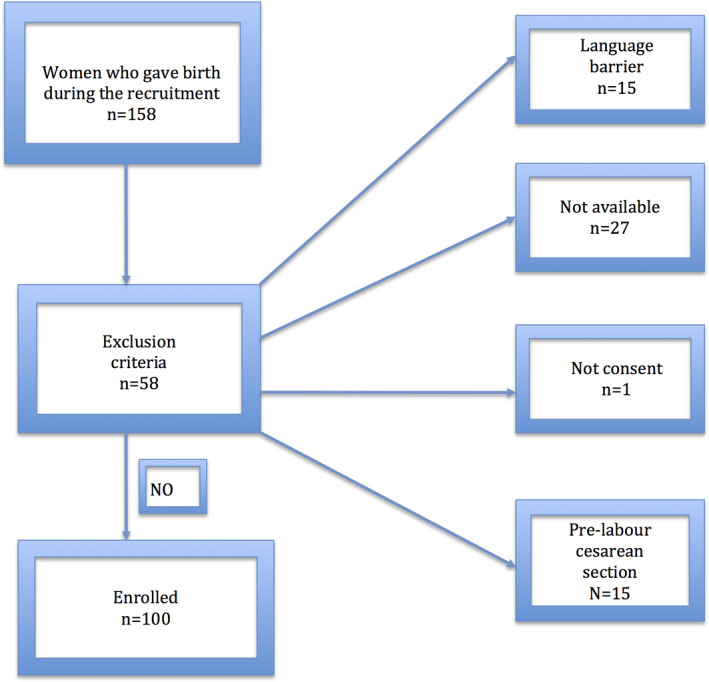
Sample size flow chart
TABLE 1.
Description of the study sample
| Variable | Overall (n = 377) | Pre COVID (n = 277) | COVID (n = 100) | p‐value | ||||
|---|---|---|---|---|---|---|---|---|
| Socio‐demographic | mean | SD | mean | SD | mean | SD | ||
| Maternal age (years) | 32.9 | 4.8 | 32.9 | 4.9 | 32.9 | 4.5 | .92 | |
| n | % | n | % | n | % | |||
| Education (graduated) | 160 | 42.4 | 112 | 40.4 | 48 | 48.0 | .18 | |
| Employed | 320 | 84.9 | 234 | 84.5 | 86 | 86.0 | .71 | |
| Origin (Caucasian) | 363 | 96.3 | 268 | 96.8 | 95 | 95.0 | .42 | |
| Ostetric history | Parity (primiparous) | 211 | 56.0 | 149 | 53.8 | 62 | 62,0 | .15 |
No differences were reported in terms of satisfaction at birth in the two groups (I‐BSS‐R mean 27.0, SD 5.3 in pre‐COVID versus mean 27.6, SD 6.1 in COVID, p .348, Table 2), also for the three subthemes (Quality of Care Provision p .43, Women's personal attributes p 0.40, Stress experienced during labour p .13).
TABLE 2.
Satisfaction at birth
| Item (N) | Overall (n = 377) | Pre COVID (n = 277) | COVID (n = 100) | p‐value | ||||
|---|---|---|---|---|---|---|---|---|
| mean | SD | mean | SD | mean | SD | |||
| BSS‐R Total | 10 | 27.1 | 5.6 | 27.0 | 5.3 | 27.6 | 6.1 | 0.34 |
| Sub‐themes | ||||||||
| Quality of care provision | 4 | 14.1 | 1.9 | 14.1 | 1.8 | 13.9 | 2.2 | 0.43 |
| Women's personal attributes | 2 | 4.7 | 2.0 | 4.6 | 2.0 | 4.8 | 1.9 | 0.40 |
| Stress experienced during labour | 4 | 8.4 | 3.3 | 8.3 | 3.2 | 8.8 | 3.5 | 0.13 |
Concerning intrapartum care, a lower number of women attended childbirth classes (51% pre‐COVID versus 26% COVID, p < .0001). Moreover, we found a higher rate of induction [25% pre‐COVID versus 40%, COVID p .004], fewer active phases >12 hr [15% pre‐COVID versus 6% COVID, p .018], more acceleration with oxytocin [24.9% pre‐COVID versus 35% COVID, p .05]. The rate of epidural analgesia was not significantly decreased (32% pre‐COVID versus 27% COVID, p .30). A reduced rate of one‐to‐one assistance, mobility during labour and rate of intermittent auscultation was registered, as reported in Table 3. Further, the two groups were comparable also in terms of mode of delivery, showing the same rate of spontaneous delivery (89.5% versus 90%, p .69).
TABLE 3.
Intrapartum care
| Intrapartum Care | Variable | Overall n = 377 | Pre‐COVID n = 277 | COVID n = 100 | p‐value | |||
| n | % | n | % | n | % | |||
| Antenatal Classes (yes) | 168 | 44.6 | 142 | 51.3 | 26 | 26.0 | <0.0001 | |
| Spontaneous Labour (yes) | 268 | 71.1 | 208 | 75.1 | 60 | 60.0 | 0.004 | |
| Active Phase >12 hr | 48 | 12.7 | 42 | 15.2 | 6 | 6.0 | 0.01 | |
| Midwifery Care | ||||||||
| One to One | 371 | 98.4 | 275 | 99.3 | 96 | 96.0 | 0.02 | |
| Mobility | 361 | 95.8 | 277 | 100,0 | 84 | 84.0 | <0.0001 | |
| Intermittent Ausculation FCF | 62 | 16.5 | 55 | 19.9 | 7 | 7.0 | 0.003 | |
| Intrapartum Interventions | ||||||||
| Oxitocin (yes) | 104 | 27.6 | 69 | 24.9 | 35 | 35.0 | 0.05 | |
| Epidural analgesia (yes) | 117 | 31.0 | 90 | 32.5 | 27 | 27.0 | 0.30 | |
| Episiotomy (yes) | 92 | 24.4 | 74 | 26.7 | 18 | 18.0 | 0.08 | |
| Intact perineum (yes) | 45 | 11.9 | 32 | 11.6 | 13 | 13.0 | 0.70 | |
| Mode of birth | ||||||||
| Spontaneous | 338 | 89.6 | 248 | 89.5 | 90 | 90.0 | 0.69 | |
| Vacuum assisted | 27 | 7.2 | 19 | 6.9 | 8 | 8.0 | ||
| C section | 12 | 3.2 | 10 | 3.6 | 2 | 2.0 | ||
Intrapartum variables that impacted negatively on maternal satisfaction were the same in the two periods (Table 4): epidural analgesia (p < .0001 versus p < .0001), prolonged active phases >12 hr (p < .0001 versus p .0001), oxytocin administration (p < .0001 versus p < .0001) and operative delivery (p .0009 versus p .0019). On the other hand, induction reduced satisfaction (p .11 in pre‐COVID versus p .004 in COVID), while antenatal classes and episiotomy/intact perineum were no more correlated with satisfaction at birth in COVID era. The absolute lowest scores in COVID era were found in those women who underwent active phases >12 hr (mean score 19, SD 6 compared to the mean score in COVID 27.6) and CS in labour (mean score 17, SD 12 compared to mean score 27.6).
TABLE 4.
Impact of Intrapartum variables on I‐BSS‐R (Total)
| Variables | Pre COVID (n = 277) | COVID (n = 100) | ||||
|---|---|---|---|---|---|---|
| Mean | SD | p‐value | Mean | SD | p‐value | |
| Nulliparous | 26.28 | 5.78 | 0.02 | 26.10 | 6.09 | 0.001 |
| Multiparous | 27.77 | 4.68 | 30 | 5.40 | ||
| Antenatal classes (yes) | 26.32 | 5.59 | 0.03 | 26.69 | 6.66 | 0.28 |
| Antenatal classes (no) | 27.65 | 5.00 | 28.15 | 5.69 | ||
| Spontaneous labour | 27.26 | 5.13 | 0.11 | 28.98 | 5.21 | 0.004 |
| Induction of labour | 26.08 | 5.90 | 25.47 | 6.80 | ||
| Epidural (yes) | 24.7 | 5.95 | <0.0001 | 22.63 | 6.43 | <0.0001 |
| Epidural (no) | 28.06 | 4.66 | 29.41 | 4.88 | ||
| Active Phase >12 hr | 23.31 | 5.60 | <0.0001 | 18.17 | 6.01 | 0.0001 |
| Active Phase <=12 hr | 27.63 | 4.95 | 28.18 | 5.64 | ||
| Oxytocin (yes) | 24.20 | 6.04 | <0.0001 | 24 | 6.25 | <0.0001 |
| Oxytocin (no) | 27.89 | 4.76 | 29.51 | 5.12 | ||
| Spontaneous | 27.37 | 5.05 | 0.0009 | 28.24 | 5.24 | 0.0019 |
| Vacuum assisted | 23.21 | 5.92 | 22.75 | 9.57 | ||
| C section | 24.1 | 7.84 | 17 | 12.73 | ||
| Episiotomy (yes) | 25.97 | 5.63 | 0.06 | 25.94 | 6.23 | 0.21 |
| Episiotomy (no) | 27.33 | 5.20 | 27.93 | 6.07 | ||
| Intact Perineum (yes) | 29.31 | 3.77 | 0.008 | 28.76 | 5.64 | 0.45 |
| Intact Perineum (no) | 26.66 | 5.45 | 27.40 | 6.19 | ||
From a qualitative point of view, women were also asked to report which factor affected most their childbirth experience (Figure 2). 99 out of 100 women interviewed answered. 31% complained about the fact that birth partners were allowed to stay only during labour and 2%, specifically, complained about the absence of birth partners during induction. 26% reported that COVID pandemic did not affect their childbirth experience in any way. 16% was upset due to the general stressful situation of a pandemic. Wearing the PPE during labour annoyed 13%. 8% reported that, although upset, the support of the staff reassured them. 1% reported that the particular circumstance became an occasion for positive introspection. One was worried about the availability of epidural analgesia. Only one reported that she was worried about being infected by other patients.
FIGURE 2.
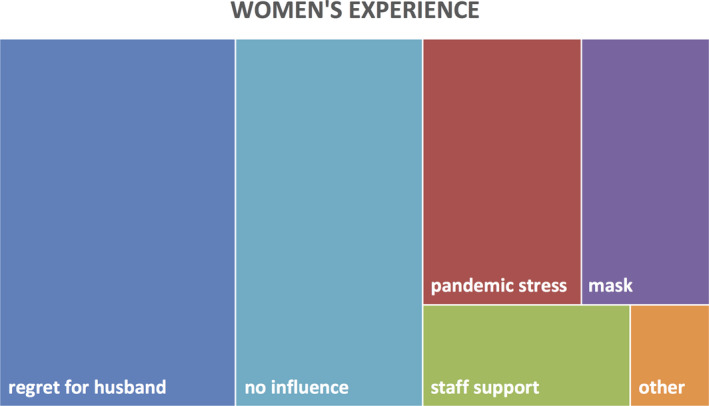
Treemap chart of the frequency of themes in a hierarchical order
5. DISCUSSION
In contrast to our first hypothesis, no difference in terms of mothers' satisfaction with their childbirth experience was demonstrated comparing those who delivered during COVID pandemic to those who gave birth before the pandemic, in the same context of a low‐risk maternity unit in Northern Italy. We found three possible explanations of this unexpected result: first, we continued to recruit women also in the first half of May 2020, when the global burden of the emergency started to decrease, thus probably determining a better perception compared to the first study period (see also in the Limitations of the study). Second, it is possible that our efforts in paying attention to women's needs despite the emergency context (for example, in contrast to other hospitals in Italy, we always gave permission to birth partner to enter during active labour) were appreciated by them, determining a high level of satisfaction. Third, we have only a little knowledge in general on quality scales in obstetrics, and, in particular, on the possible consequences of external circumstances (like the pandemia) on a private and intimate event such as childbirth.
Similarly, a recent study pointed out that the psychological impact and anxiety of the COVID‐19 epidemic seemed to be more severe in women who were in the first trimester of pregnancy during the outbreak (Saccone et al., 2020).
Concerning our second hypothesis, related to changes in practice, fewer women attended childbirth classes and this can be explained by COVID‐related restrictions such as the conversion of live lessons into online modules to avoid social contacts. Taking into account this different modality, attending antenatal classes did not affect in any way satisfaction at birth in contrast to our previous investigation.
As expected, an increased rate of intervention was found (higher rate of induction, fewer active phases >12 hr, more acceleration with oxytocin) and this can be due to the specific context of the COVID pandemic. The desire to reduce antenatal checks, duration of labour, hospitalization and reduced availability of epidural analgesia could have promoted a more interventional obstetric approach. Further, as hypothesized, a slight reduction in midwives' assistance quality was observed (reduced rate of one‐to‐one assistance, lower mobility during labour and lower rate of intermittent auscultation). We can argue that this can be a consequence of the stressful environment during an emergency, although it did not affect the global satisfaction of women.
Concerning intrapartum variables that could affect satisfaction, similarly to the perception before COVID (Fumagalli et al., 2020) and to other research (Fleming et al., 2016; Rijnders et al., 2008; Çalik et al., 2018) we showed that lower birth satisfaction was experienced with interventions, such as epidural analgesia, active phases longer than 12 hr, oxytocin administration and operative delivery. However, the impact of induction of labour changed according to the period of interest. Specifically, it was not associated with satisfaction in women treated before the pandemic, whereas it was associated with lower satisfaction in those treated during the emergency. This finding can be partly explained by the absence of birth partners before active labour and it is also confirmed by women's free reports on the experience in the hospital during COVID (31% complained about the fact that birth partners were allowed to stay only during labour). This observation is also linked to another interesting finding, namely the absolute lowest scores in COVID era were in those women who underwent active phases longer than 12 hr and CS in labour, considering that both conditions are often related to prolonged times.
5.1. Strength and limitations
This is for our knowledge the first study on practice‐changing and satisfaction at birth during COVID pandemic. The possibility of comparing these women to a pre‐COVID cohort from the same maternity unit and with the same methods is a point of strength in order to ensure homogeneity in obstetric care.
However, our study is not devoid of limitations. First, it was performed only in one hospital and, consequently, we cannot know to what extent our findings are generalizable. Second, we continued to recruit women also in the first half of May 2020, when the global burden of the emergency started to decrease, thus probably determining a different perception. On the other side, the preventive measures adopted in the hospital remained unchanged for the whole duration of the study.
6. CONCLUSIONS
No differences were reported concerning global satisfaction at birth, although an increased rate of active intervention was noticed (higher rate of induction, fewer active phases longer than 12 hr, more acceleration with oxytocin). Induction, active phases longer than 12 hr and CS in labour were less accepted in COVID era. This specific context can help us in analysing which factors can be improved with the assistance of women, in order to guarantee a good perception both in emergent and routinely scenarios.
CONFLICT OF INTEREST
There are no conflicts of interests to declare.
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
We would like to express our gratitude to all the doctors and nurses who helped in developing this project, in particular D.V. and S.V.
Inversetti A, Fumagalli S, Nespoli A, et al. Childbirth experience and practice changing during COVID‐19 pandemic: A cross‐sectional study. Nurs Open. 2021;8:3627–3634. 10.1002/nop2.913
Funding information
No external funding was used in the conduct of this study.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author AL upon reasonable request.
REFERENCES
- Çalik, K. Y. , Karabulutlu, Ö. , & Yavuz, C. (2018). First do no harm — interventions during labour and maternal satisfaction: A descriptive cross‐sectional study. BMC Pregnancy Childbirth, 18, 415. 10.1186/s12884-018-2054-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming, S. E. , Donovan‐Batson, C. , Burduli, E. , Barbosa‐Leiker, C. , Hollins Martin, C. J. , & Martin, C. R. (2016). Birth Satisfaction Scale/Birth Satisfaction Scale‐Revised (BSS/BSS‐R): A large scale United States planned home birth and birth centre survey. Midwifery, 4, 9–15. 10.1016/j.midw.2016.07.008 [DOI] [PubMed] [Google Scholar]
- Fumagalli, S. , Colciago, E. , Antolini, L. , Riva, A. , Nespoli, A. , & Locatelli, A. (2020). Variables related to maternal satisfaction with intrapartum care in Northern Italy. Women and Birth, 34(2), 154–161. 10.1016/j.wombi.2020.01.012 [DOI] [PubMed] [Google Scholar]
- Green, J. M. (1993). Expectations and experiences of pain in labour: Findings from a large prospective study. Birth, 20(2), 65–72. [DOI] [PubMed] [Google Scholar]
- Hinic, K. (2017). Understanding and promoting Birth satisfaction in New Mothers. MCN. American J Matern Child Nurs, 42, 210–215. 10.1097/NMC.0000000000000345 [DOI] [PubMed] [Google Scholar]
- Hodnett, E. D. (2002). Caregiver support for women during childbirth. Cochrane Database Systematic Review, 2002;(1):CD000199. [DOI] [PubMed] [Google Scholar]
- Hollins Martin, C. J. , & Fleming, V. (2011). The Birth Satisfaction Scale (BSS). International Journal of Health Care Quality Assurance., 24(2), 124–135. 10.1108/09526861111105086 [DOI] [PubMed] [Google Scholar]
- Hollins Martin, C. J. , & Martin, C. R. (2014). Development and psychometric properties of the Birth Satisfaction Scale‐Revised (BSS‐R). Midwifery., 30(6), 610–619. 10.1016/j.midw.2013.10.006 [DOI] [PubMed] [Google Scholar]
- Karlström, A. , Nystedt, A. , & Hildingsson, I. (2015). The meaning of a very positive birth experience: Focus groups discussions with women. BMC Pregnancy Childbirth, 15, 251. 10.1186/s12884-015-0683-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larkin, P. , Begley, C. M. , & Devane, D. (2009). Women’s experiences of labour and birth: An evolutionary concept analysis. Midwifery, 25, e49–e59. 10.1016/j.midw.2007.07.010 [DOI] [PubMed] [Google Scholar]
- Narang, K. , Ibirogba, E. R. , Elrefaei, A. , Abrao Trad, A. T. , Theiler, R. , Nomura, R. et al (2020). SARS‐CoV‐2 in Pregnancy: A Comprehensive Summary of Current Guidelines. Journal of Clinical Medicine, 9, 1521. 10.3390/jcm9051521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nespoli, A. , Colciago, E. , Fumagalli, S. , Locatelli, A. , Hollins Martin, C. J. , & Martin, C. R. (2020). Validation and factor structure of the Italian version of the Birth Satisfaction Scale‐Revised (BSS‐R). Journal of Reproductive and Infant Psychology, 21, 1–16. 10.1080/02646838.2020.1836333 [DOI] [PubMed] [Google Scholar]
- Odone, A. , Delmonte, D. , Scognamiglio, T. , & Signorelli, C. (2020). Covid‐19 deaths in Lombardy, Italy: Data in context. Lancet Public Health, 5, e310. 10.1016/S2468-2667(20)30099-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravaldi, C. , Wilson, A. , Ricca, V. , Homer, C. , & Vannacci, A. (2020). Pregnant women voice their concerns and birth expectations during the COVID‐19 pandemic in Italy. Women and Birth, 13(20), 1871–5192. 10.1016/j.wombi.2020.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rijnders, M. , Baston, H. , Schönbeck, H. , van der Pal, K. , Prins, M. , Green, J. et al (2008). Perinatal factors related to negative or positive recall of birth experience in women 3 years postpartum in the Netherlands. Birth, 35, 107–116. 10.1111/j.1523-536X.2008.00223.x [DOI] [PubMed] [Google Scholar]
- Saccone, G. , Florio, A. , Venturella, R. , De Angelis, M. C. , Locci, M. , Bifulco, G. et al (2020). Psychological impact of COVID‐19 during pregnancy. American Journal of Obstetrics and Gynecology, 223, 293–295. 10.1016/j.ajog.2020.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldenstrom, U. , & Nilsson, C. A. (1993). Women’s satisfaction with birth centre care: A randomised, controlled study. Birth, 21(1), 3–13. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
The data that support the findings of this study are available from the corresponding author AL upon reasonable request.


