Abstract
Keywords: Australia; COVID‐19; emergency medical services; SARS‐CoV‐2, coronavirus disease
To the Editors:
In August 2020, the World Health Organization reported that 89% of 105 surveyed countries reported disruption to essential health services during the coronavirus disease 2019 (COVID‐19) pandemic. 1 In late June 2020, when there were 2.5 million cumulative confirmed severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infections in the United States, 2 40.9% of 4977 surveyed US adults reported having delayed or avoided medical care due to COVID‐19 concerns. 3
Given the potential short‐ and long‐term consequences of medical care delay or avoidance, we sought to determine whether similar care avoidance was observed in a region with low SARS‐CoV‐2 prevalence. As of mid‐September 2020, the Australian state of Victoria reported fewer than 20,000 cumulative SARS‐CoV‐2 cases with a low positivity rate 4 in a population of approximately 6.7 million people. Cross‐sectional Internet‐based surveys were therefore administered to respondent panellists aged ≥18 years residing in Victoria by Qualtrics using quota sampling in the third Australian wave of The COVID‐19 Outbreak Public Evaluation (COPE) Initiative (www.thecopeinitiative.org). To assess medical care avoidance cross‐sectionally while minimizing potential confounders of varying mitigation measures or SARS‐CoV‐2 prevalence, surveys were administered during 15–24 September 2020, when peak COVID‐19 prevention measures were in place.
Participants were asked, ‘In the past month, have you delayed or avoided medical care due to concerns related to COVID‐19?’ Delay or avoidance was evaluated for emergency (e.g., immediate life‐threatening conditions), urgent (e.g., immediate non‐life‐threatening conditions) and routine (e.g., annual check‐ups) medical care. Urgent and emergency care avoidance were combined for analysis (urgent or emergency care) due to potential variance in perception of level of care needed, and a variable representing any care avoidance was created. Demographic and health information were collected as covariates, including sex, age, ancestry, regional versus metropolitan postcode, education attainment, employment status, unpaid caregiver status (providing unpaid care for children only, for adults only, for both age groups [multigenerational] or not an unpaid caregiver), disability status and support through the National Disabilities Insurance Scheme (NDIS) and presence of underlying conditions known to increase the risk of severe COVID‐19, including: obesity (BMI > 30 kg/m2), diabetes, hypertension, cardiovascular disease, chronic kidney disease, liver disease, chronic obstructive pulmonary disease and cancer.
Surveys underwent Qualtrics data‐quality screening procedures, including algorithmic and keystroke analysis for click‐through behaviour, duplicate responses, machine responses and inattentiveness. The investigators conducted secondary cleaning for missing sex and age, invalid postcodes and BMI below 14 or above 100 kg/m2. Iterative proportional fitting (raking) and weight trimming ([1/3] ≤ weight ≤ [3]) were employed to improve sample representativeness by age and sex according to Victorian population estimates from the Australian Bureau of Statistics 2016 Census of Population and Housing.
Rao–Scott adjusted Pearson chi‐square tests with a Bonferroni adjustment (10 comparisons) were used to test for differences in delay or avoidance of routine, urgent or emergency, and any medical care by demographic subgroups. Adjusted prevalence ratios (aPRs) and 95% CIs for delay or avoidance of any medical care were estimated using Poisson regressions with robust SEs among respondents who had complete data for the following variables: sex, age, ancestry, regional or metropolitan residence, education attainment, employment status and unpaid caregiver status. Additional models including these variables plus either disability status or presence of underlying medical conditions were used to estimate aPRs for these collinear variables. Statistical analyses were conducted with Python (version 3.7.8; Python Software Foundation) and R version 4.0.2 (The R Project for Statistical Computing) using the R survey package version 3.29; p < 0.05 were deemed statistically significant.
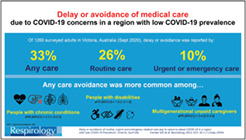
During 15–24 September 2020, 1260 of 4900 (25.7%) eligible invited Victorian adults completed surveys, including 1168 (92.7%) first‐time respondents and 92 (7.3%) re‐contacted respondents. Overall, 414 (32.9%) adults reported having delayed or avoided any medical care due to concerns about COVID‐19, including routine medical care (333 [26.4%]) and urgent or emergency care (128 [10.1%]) (Table 1).
TABLE 1.
Prevalence of and aPRs for having delayed or avoided medical care, by select respondent characteristics
| All respondents | Avoid or delay routine medical care | Avoid or delay urgent or emergency care | Avoid or delay any type of care | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % a | n | % a | n | % a | n | % a | aPR b (95% CI) | p | |
| Total respondents | 1260 | 100 | 333 | 26.4 | 128 | 10.1 | 414 | 32.9 | — | — |
| Sex | ||||||||||
| Female | 649 | 51.5 | 184 | 28.3 | 53 | 8.2 | 220 | 33.9 | 1.30 (1.09, 1.55) | 0.0036 |
| Male | 611 | 48.5 | 149 | 24.4 | 74 | 12.2 | 194 | 31.8 | 1 (Ref) | |
| Age group in years | c | c | c | |||||||
| 18–24 | 153 | 12.1 | 38 | 24.7 | 23 | 15.1 | 53 | 34.6 | 1.31 (0.79, 2.17) | 0.30 |
| 25–44 | 460 | 36.5 | 165 | 35.9 | 65 | 14.1 | 205 | 44.5 | 1.39 (0.95, 2.02) | 0.089 |
| 45–64 | 396 | 31.4 | 89 | 22.5 | 30 | 7.6 | 109 | 27.6 | 1.11 (0.77, 1.61) | 0.57 |
| ≥65 | 251 | 19.9 | 40 | 16.2 | 9 | 3.7 | 47 | 18.6 | 1 (Ref) | |
| Ancestry d | c | |||||||||
| Oceanian | 307 | 24.4 | 81 | 26.2 | 46 | 14.9 | 110 | 35.9 | 1 (Ref) | |
| North‐West European | 371 | 29.5 | 87 | 23.3 | 23 | 6.1 | 106 | 28.6 | 0.91 (0.73, 1.13) | 0.38 |
| Southern and Eastern European | 118 | 9.3 | 23 | 19.4 | 7 | 5.8 | 28 | 23.8 | 0.79 (0.56, 1.12) | 0.19 |
| South‐East Asian | 55 | 4.3 | 13 | 23.7 | 3 | 6.3 | 13 | 23.7 | 0.71 (0.44, 1.15) | 0.16 |
| North‐East Asian | 84 | 6.7 | 23 | 27.2 | 8 | 9.6 | 29 | 34.7 | 1.10 (0.78, 1.54) | 0.59 |
| Southern and Central Asian | 97 | 7.7 | 33 | 33.7 | 13 | 13.5 | 41 | 41.9 | 1.14 (0.85, 1.53) | 0.39 |
| North‐West European, Oceanian | 103 | 8.2 | 37 | 36.2 | 17 | 16.1 | 44 | 42.2 | 1.19 (0.90, 1.56) | 0.23 |
| Other ancestry or other combination | 110 | 8.7 | 30 | 27.6 | 8 | 7.2 | 35 | 32.3 | No estimate | |
| Unknown | 15 | 1.2 | 6 | 42.2 | 3 | 22.0 | 8 | 51.9 | No estimate | |
| Disability | c | c | c | |||||||
| No | 1091 | 86.6 | 271 | 24.9 | 94 | 8.6 | 333 | 30.6 | 1 (Ref) | |
| Yes, with support from the NDIS | 48 | 3.8 | 31 | 63.8 | 18 | 36.8 | 40 | 83.9 | 1.46 (1.21, 1.75) | 0.0001 |
| Yes, without support from the NDIS | 101 | 8.0 | 26 | 26.0 | 14 | 14.2 | 34 | 33.9 | 1.44 (1.06, 1.95) | 0.018 |
| Prefer not to say | 20 | 1.6 | 4 | 21.0 | 2 | 9.3 | 6 | 30.3 | No estimate | |
| Health conditions known to increase risk for severe COVID‐19 e | c | c | c | |||||||
| No | 664 | 52.7 | 150 | 22.6 | 41 | 6.1 | 177 | 26.6 | 1 (Ref) | |
| One | 317 | 25.2 | 80 | 25.1 | 35 | 11.0 | 101 | 31.7 | 1.45 (1.14, 1.83) | 0.0022 |
| Two or more | 278 | 22.1 | 103 | 36.8 | 52 | 18.7 | 137 | 49.0 | 2.02 (1.60, 2.54) | <0.0001 |
| Residence and COVID‐19 restrictions level f | ||||||||||
| Regional (Stage 3 lockdowns) | 256 | 20.3 | 63 | 24.7 | 26 | 10.1 | 80 | 31.2 | 1 (Ref) | |
| Metropolitan (Stage 4 lockdowns) | 1004 | 79.7 | 269 | 26.8 | 102 | 10.2 | 334 | 33.3 | 0.91 (0.74, 1.13) | 0.40 |
| Education attainment | c | c | c | |||||||
| Secondary school diploma or less | 398 | 31.6 | 84 | 21.1 | 24 | 5.9 | 97 | 24.4 | 0.87 (0.68, 1.10) | 0.24 |
| Some university | 204 | 16.2 | 43 | 21.0 | 18 | 8.9 | 57 | 27.8 | 0.91 (0.68, 1.23) | 0.55 |
| Bachelor's degree or equivalent | 492 | 39.1 | 135 | 27.5 | 54 | 11.0 | 173 | 35.1 | 1 (Ref) | |
| Doctoral or professional degree | 156 | 12.4 | 68 | 43.2 | 31 | 19.7 | 83 | 53.4 | 1.21 (1.00, 1.47) | 0.046 |
| Unknown | 9 | 0.7 | 3 | 31.7 | 1 | 11.1 | 4 | 42.7 | No estimate | |
| Employment status | c | c | ||||||||
| Employed non‐essential | 339 | 26.9 | 89 | 26.3 | 28 | 8.4 | 108 | 31.8 | 1 (Ref) | |
| Employed essential | 410 | 32.5 | 124 | 30.2 | 69 | 16.9 | 174 | 42.4 | 1.10 (0.90, 1.34) | 0.36 |
| Retired | 269 | 21.3 | 47 | 17.5 | 7 | 2.5 | 50 | 18.5 | 0.87 (0.59, 1.28) | 0.47 |
| Unemployed | 191 | 15.2 | 60 | 31.1 | 19 | 9.8 | 68 | 35.3 | 1.13 (0.86, 1.49) | 0.37 |
| Student | 51 | 4.1 | 13 | 25.5 | 5 | 9.2 | 15 | 29.9 | 0.86 (0.47, 1.55) | 0.60 |
| Unpaid caregiver status | c | c | c | |||||||
| Not unpaid caregiver | 759 | 60.2 | 160 | 21.1 | 45 | 5.9 | 180 | 23.7 | 1 (Ref) | |
| Unpaid caregiver for adults | 172 | 13.6 | 52 | 30.3 | 18 | 10.8 | 65 | 37.8 | 1.52 (1.17, 1.98) | 0.0017 |
| Unpaid caregiver for children | 140 | 11.1 | 30 | 21.5 | 10 | 7.4 | 41 | 29.0 | 1.08 (0.79, 1.48) | 0.64 |
| Multigenerational unpaid caregiver (i.e., for both age groups) | 189 | 15.0 | 90 | 47.7 | 54 | 28.6 | 128 | 67.8 | 2.42 (1.98, 2.97) | <0.0001 |
Abbreviations: aPR, adjusted prevalence ratio; COVID‐19, coronavirus disease 2019; NDIS, National Disabilities Insurance Scheme.
For all respondents (Columns 2 and 3), percentages are based on the number of respondents in a demographic group out of all respondents (n = 1260). For type of care avoided or delayed (Columns 4 through 9), percentages are reported based on the number of respondents who delayed or avoided care within that demographic group.
Multivariable Poisson regression models include all variables listed in table, except for disability status and health conditions, which were run in separate models that also included all demographic variables to avoid collinearity between these two variables. The primary demographic model included 1260 respondents. The model including disability status included 1112 respondents, and the model including health conditions included 1127 respondents.
Bonferroni‐adjusted Rao–Scott adjusted Pearson chi‐square test result was statistically significant (p < 0.05) for the demographic subgroup below the marker. Chi‐square tests excluded ‘Unknown’ and ‘Other ancestry or other combination’ categories.
The ‘Other ancestry or other combination’ category included persons who were North African and Middle Eastern, Sub‐Saharan African, People of the Americas or a combination of ancestries other than North‐West European and Oceanian. Estimates were not provided for Other or Unknown due to small counts and the inability to meaningfully characterize the ancestry off these respondents.
Obesity (BMI > 30 kg/m2), diabetes, hypertension, cardiovascular disease, chronic kidney disease, liver disease, sickle cell disease, chronic obstructive pulmonary disease and/or cancer.
Regional‐metropolitan classification and COVID‐19 restriction levels were determined using self‐reported postal codes according to the Victorian Department of Health and Human Services COVID‐19 local regional restrictions map (https://www.dhhs.vic.gov.au/victorias‐restriction‐levels‐covid‐19).
Populations that most commonly reported delay or avoidance of any medical care were those with disabilities with NDIS support (40 of 48 [83.9%]), multigenerational unpaid caregivers (128 of 189 [67.8%]), adults with higher education degrees (83 of 156 [53.4%]), adults with multiple medical conditions that increase the risk of severe COVID‐19 (137 of 278 [49.0%]) and essential workers (174 of 410 [42.4%]). Avoidance of any care did not differ significantly by sex; however, routine care avoidance was more common among female compared to male respondents (184 of 649 [28.3%] vs. 149 of 611 [24.4%], respectively), and urgent or emergency care avoidance was more common among male compared to female respondents (74 [12.2%] vs. 53 [8.2%], respectively).
Multivariate Poisson regression revealed that avoidance of any medical care was more common among multigenerational unpaid caregivers and unpaid caregivers for adults compared to those who were not unpaid caregivers (e.g., multigenerational, aPR = 2.42, 95% CI = 1.98–2.97, p < 0.0001); in those with multiple medical conditions compared to those without (one health condition, aPR = 1.45, 95% CI = 1.14–1.83, p = 0.0022; two or more health conditions, aPR = 2.02, 95% CI = 1.60–2.54, p < 0.0001); those with disabilities compared to those without disabilities (with NDIS support, aPR = 1.46, 95% CI = 1.21–1.75, p = 0.0001; without NDIS support, aPR = 1.44, 95% CI = 1.06–1.95, p = 0.018); females compared to males (aPR = 1.30, 95% CI = 1.09–1.55, p = 0.0036); and those with a doctoral or professional degree versus a bachelor's degree (aPR = 1.21, 95% CI = 1.00–1.47, p = 0.046).
These findings provide important insights regarding healthcare‐seeking behaviour during the COVID‐19 pandemic in a region with relatively low SARS‐CoV‐2 prevalence. Intentional medical care avoidance may have contributed to the observed 22% decrease in Victorian emergency department (ED) presentations during September 2020 compared to September 2019. 5
Individuals with multiple medical conditions associated with an increased risk of severe COVID‐19 more commonly avoided or delayed urgent or emergency care, a finding also observed in the United States. 3 This is particularly concerning, as in addition to higher risk of severe COVID‐19, these conditions put individuals at greater risk of other acute medical conditions for which time‐critical interventions can reduce morbidity and mortality. Decreased presentations of stroke and myocardial infarction occurred during July and August 2020 in Victoria, Australia, 5 and symptom‐to‐door‐time for patients with acute coronary syndrome requiring revascularization increased four‐fold during March and April 2020, whilst overall case presentations remained unchanged. 6 These observations suggest that people delayed seeking urgent care.
Early evidence of consequences of disrupted routine care during the COVID‐19 pandemic have been reported, particularly in relation to cancer screening and diagnoses. Reduced screening, referrals and presentations for lung and colorectal cancers in the UK have led to projections of 4.8% and 16.5% increased deaths, respectively, within 5 years of diagnosis. 7 , 8 In Victoria, on 11 September 2020, the Premier urged Victorians to stop delaying hospital visits and health check‐ups due to the pandemic, as not only had ED visits reduced, diagnoses for common cancers had reduced by approximately one‐third. 9 Findings from this study suggest that strategies to reduce COVID‐19‐related care avoidance may be warranted, with enhanced efforts among at‐risk groups.
Although quota sampling and survey weighting were employed to improve sample representatives of the Victorian population by age and sex, the sample may not be fully representative of the 2020 Victorian population. Furthermore, self‐reported data may be subject to recall and response biases, and this study did not assess reasons for COVID‐19 care avoidance or baseline patterns of care‐seeking or avoidance in this population; however, the results are consistent with trends in Victorian hospital and ED admissions data. Finally, although the survey items specified that the reason for delay or avoidance of medical care was COVID‐19 concerns, respondents did not detail sources of these concerns (e.g., fear of SARS‐CoV‐2 infection or spreading SARS‐CoV‐2 to others at the healthcare facility, during transportation to or from the facilities). Future research could identify such sources of COVID‐19‐related concerns, and what measures may lead to their alleviation.
Given that considerable portions of adults reported having delayed or avoided medical care due to COVID‐19 concerns in regions with minimal (Victoria) and substantial (United States) community transmission of SARS‐CoV‐2, determining the extent to which similar behaviour has continued in these regions and may be occurring in other regions is warranted. To that end, the World Health Organization has recently developed a population health surveillance tool to monitor delay or avoidance of medical care among the wider effects of the COVID‐19 pandemic. 10
Proactive public health messaging and targeted services to minimize healthcare avoidance—particularly for individuals with chronic medical conditions, people with disabilities and unpaid caregivers—may be critical to avoid preventable increases in all‐cause morbidity and mortality during and beyond the COVID‐19 pandemic.
AUTHOR CONTRIBUTIONS
Mark Czeisler: Conceptualization; data curation; formal analysis; investigation; methodology; writing‐original draft; writing‐review & editing. Jessica Kennedy: Conceptualization; formal analysis; investigation; writing‐original draft; writing‐review & editing. Joshua Wiley: Formal analysis; methodology; writing‐review & editing. Elise Facer‐Childs: Conceptualization; writing‐review & editing. Rebecca Robbins: Conceptualization; writing‐review & editing. Laura Barger: Conceptualization; writing‐review & editing. Charles Czeisler: Conceptualization; funding acquisition; methodology; writing‐review & editing. Shantha Rajaratnam: Conceptualization; funding acquisition; investigation; methodology; supervision; writing‐review & editing. Mark Howard: Conceptualization; funding acquisition; investigation; methodology; supervision; writing‐original draft; writing‐review & editing.
CONFLICT OF INTEREST
Mark É. Czeisler, Charles A. Czeisler, Shantha M. W. Rajaratnam and Mark E. Howard report grants from the CDC Foundation with funding from BNY Mellon, and grants from WHOOP and Hopelab, outside the submitted work. Mark É. Czeisler reported receiving personal fees from Vanda Pharmaceuticals outside the submitted work. Rebecca Robbins reports personal fees from Denihan Hospitality, Rituals Cosmetics, SleepCycle, Dagmejan and byNacht. Laura K. Barger reports a grant from the National Institute for Occupational Safety and Health and personal fees from the University of Pittsburgh, CurAegis, Casis, Puget Sound Pilots and Boston Children's Hospital. Charles A. Czeisler reported receiving grants to support. The COVID‐19 Outbreak Public Evaluation (COPE) Initiative and grants from Brigham and Women's Physician's Organization during the conduct of the study; being a paid consultant to or speaker for Ganésco, Institute of Digital Media and Child Development, Klarman Family Foundation, M. Davis and Co, Physician's Seal, Samsung Group, State of Washington Board of Pilotage Commissioners, Tencent Holdings, Teva Pharma Australia and Vanda Pharmaceuticals, in which Charles A Czeisler holds an equity interest; receiving travel support from Aspen Brain Institute, Bloomage International Investment Group, UK Biotechnology and Biological Sciences Research Council, Bouley Botanical, Dr Stanley Ho Medical Development Foundation, Illuminating Engineering Society, National Safety Council, Tencent Holdings and The Wonderful Co; receiving institutional research and/or education support from Cephalon, Mary Ann and Stanley Snider via Combined Jewish Philanthropies, Harmony Biosciences, Jazz Pharmaceuticals PLC, Johnson and Johnson, Neurocare, Peter Brown and Margaret Hamburg, Philips Respironics, Regeneron Pharmaceuticals, Regional Home Care, Teva Pharmaceuticals Industries, Sanofi S.A., Optum, ResMed, San Francisco Bar Pilots, Schneider National, Serta, Simmons Betting, Sysco and Vanda Pharmaceuticals; being or having been an expert witness in legal cases, including those involving Advanced Power Technologies, Aegis Chemical Solutions, Amtrak, Casper Sleep, C and J Energy Services, Complete General Construction, Dallas Police Association, Enterprise Rent‐A‐Car, Steel Warehouse Co, FedEx, Greyhound Lines, Palomar Health District, PAR Electrical, Product, and Logistics Services, Puckett Emergency Medical Services, South Carolina Central Railroad Co, Union Pacific Railroad, UPS and Vanda Pharmaceuticals; serving as the incumbent of an endowed professorship provided to Harvard University by Cephalon; and receiving royalties from McGraw Hill and Philips Respironics for the Actiwatch‐2 and Actiwatch Spectrum devices. Charles A. Czeisler's interests were reviewed and are managed by the Brigham and Women's Hospital and Mass General Brigham in accordance with their conflict of interest policies. Shantha M. W. Rajaratnam reported receiving institutional consulting fees from CRC for Alertness, Safety, and Productivity, Teva Pharmaceuticals, Vanda Pharmaceuticals, Circadian Therapeutics, BHP Billiton and Herbert Smith Freehills; receiving grants from Teva Pharmaceuticals and Vanda Pharmaceuticals; and serving as chair for the Sleep Health Foundation outside the submitted work. No other disclosures were reported.
HUMAN ETHICS APPROVAL DECLARATION
The Monash University Human Research Ethics Committee (Melbourne, Australia) approved the study (24036). The participants provided informed electronic consent prior to data collection.
Supporting information
Visual_Abstract
ACKNOWLEDGEMENTS
The authors thank all of The COPE Initiative survey respondents, along with Qualtrics research team members Mallory Colys, Sneha Baste, Daniel Chong and Rebecca Toll for their assistance in the survey administration. Research funding: The authors gratefully acknowledge funding for this study from the Turner Institute for Brain and Mental Health of Monash University, and institutional support from Brigham and Women's Hospital through Philips Respironics, Inc., and from the Institute for Breathing and Sleep of Austin Health. Mark É. Czeisler gratefully acknowledges funding from the Australian‐American Fulbright Commission administered through a 2020 Fulbright Future Scholarship funded by The Kinghorn Foundation. Elise R. Facer‐Childs acknowledges funding from the Science and Industry Endowment Fund Ross Metcalf STEM+ Business Fellowship administered by the Commonwealth Scientific and Industrial Research Organisation, Canberra, Australia.
Czeisler MÉ, Kennedy JL, Wiley JF, et al. Delay or avoidance of routine, urgent and emergency medical care due to concerns about COVID‐19 in a region with low COVID‐19 prevalence: Victoria, Australia. Respirology. 2021;26:707–712. 10.1111/resp.14094
Mark É Czeisler and Jessica L Kennedy contributed equally to this study.
Handling Editor: Philip Bardin
Funding information Turner Institute for Brain and Mental Health , Monash University; Commonwealth Scientific and Industrial Research Organisation, Canberra, Australia; Science and Industry Endowment Fund Ross Metcalf STEM+ Business Fellowship; The Kinghorn Foundation; Australian‐American Fulbright Commission
REFERENCES
- 1. World Health Organization . Pulse survey on continuity of essential health services during the COVID‐19 pandemic – interim report 27 August 2020. In: World Health Organization, editor. COVID‐19: essential health services. WHO; 2020. p. 21. Geneva, Switzerland. https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2020.1
- 2. Dong E, Du H, Gardner L. An interactive web‐based dashboard to track COVID‐19 in real time. Lancet Infect Dis. 2020;20:533–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Czeisler MÉ, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, et al. Delay or avoidance of medical care because of COVID‐19‐related concerns – United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Australian Government Department of Health. Coronavirus (COVID‐19) current situation and case numbers. 2020. https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/coronavirus-covid-19-current-situation-and-case-numbers#cases-active-cases-and-deaths-by-state-and-territory. Accessed 24 Mar 2021.
- 5. Berecki‐Gisolf J, Sheppard D, Stathakis V, Fernando T, Hayman J, Rezaei‐Darzi E, et al. Injuries during the COVID‐19 pandemic. 2020. https://www.monash.edu/muarc/research/research‐areas/home‐and‐community/visu/injuries‐during‐the‐covid‐19‐pandemic. Accessed 24 Mar 2021.
- 6. Toner L, Koshy AN, Hamilton GW, Clark D, Farouque O, Yudi MB. Acute coronary syndromes undergoing percutaneous coronary intervention in the COVID‐19 era: comparable case volumes but delayed symptom onset to hospital presentation. Eur Heart J Qual Care Clin Outcomes. 2020;6:225–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dinmohamed AG, Visser O, Verhoeven RHA, Louwman MWJ, van Nederveen FH, Willems SM, et al. Fewer cancer diagnoses during the COVID‐19 epidemic in the Netherlands. Lancet Oncol. 2020;21:750–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R, et al. The impact of the COVID‐19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population‐based, modelling study. Lancet Oncol. 2020;21:1023–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Andrews D. Hospitals ready and waiting to support all Victorians. 2020. https://www.premier.vic.gov.au/hospitals-ready-and-waiting-support-all-victorians. Accessed 24 Mar 2021.
- 10. World Health Organization: Regional Office for Europe . Strengthening population health surveillance: a tool for selecting indicators to signal and monitor the wider effects of the COVID‐19 pandemic. World Health Organization: Regional Office for Europe; Copenhagen, Denmark. 2021. https://apps.who.int/iris/handle/10665/340720. License: CC BY‐NC‐SA 3.0 IGO. Accessed date, 7 May 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Visual_Abstract


