Abstract
OBJECTIVE
We aimed to explore the associations between type 2 diabetes onset age and cardiovascular disease (CVD) and all-cause mortality in the Chinese population.
RESEARCH DESIGN AND METHODS
This study included 101,080 participants free of prevalent diabetes and CVD at baseline from the Kailuan Study. All participants were monitored biennially until 31 December 2017. During follow-up, 11,384 participants were diagnosed as having type 2 diabetes. For each case subject, one control subject was randomly selected, matched for age (± 1 years) and sex. The final analysis comprised 10,777 case-control pairs. Weighted Cox regression models were used to evaluate the average hazard ratios (AHRs) and 95% CIs of incident CVD and all-cause mortality among patients with new-onset type 2 diabetes versus control subjects across age-groups.
Results
During a median follow-up of 5.57 years, 1,794 incident events (907 CVD events, of which there were 725 strokes and 887 deaths) occurred. After adjustment for potential confounders, participants with type 2 diabetes diagnosed at age <45 years had the highest relative risks of CVD and all-cause mortality relative to the matched control subjects, with AHRs of 3.21 (95% CI 1.18–8.72) for CVD, 2.99 (95% CI 1.01–9.17) for stroke, and 4.79 (95% CI 1.95–11.76) for all-cause mortality. The risks gradually attenuated with each decade increase in type 2 diabetes onset age.
CONCLUSIONS
The relative risks of CVD and all-cause mortality differed across type 2 diabetes onset age-groups, and the associations were more evident in younger-onset type 2 diabetes.
Introduction
With rapid socioeconomic and lifestyle changes, the prevalence of diabetes in China has increased dramatically in the past few decades, from 0.67% in 1980 to 11.2% in 2017 (1,2). The total number of people with diabetes was 116.4 million in 2019 and is expected to increase to 147.2 million by 2045 among Chinese adults (3). Type 2 diabetes represents 95% of all cases of diabetes (4). Type 2 diabetes, conventionally considered a disease of middle and older age, is increasingly diagnosed at a younger age (5). A large national survey (2015–2017) in China reported that the prevalence of diabetes was 2.0% in people aged 18–29 years and 6.3% in those aged 30–39 years (2). Furthermore, a growing body of evidence suggests that people with younger-onset type 2 diabetes have worse cardiometabolic risk profiles than those with older age at diagnosis (6,7). Thus, it is likely that younger-onset type 2 diabetes may pose relatively greater risk of cardiovascular mortality and morbidity compared with later-onset type 2 diabetes.
Indeed, previous studies have reported that people with type 2 diabetes at a younger age are more prone to developing vascular complications earlier in life, which may be associated with a higher risk of mortality and, therefore, lower life expectancy (7–10). However, these existing studies mainly estimated the health consequences of prevalent type 2 diabetes age rather than new-onset type 2 diabetes age and did not monitor the participants from their time of diagnosis, such that the effect of the duration of diabetes was not controlled for. Recently, a prospective study from Sweden reported that the relative risk of CVD and mortality compared with the general population was increased more in those with younger-onset type 2 diabetes (11). However, this study was of White populations in high-income countries, and therefore the associations between the age at onset of type 2 diabetes and CVD and mortality in the Chinese population are still unclear. Therefore, the aim of our study was to estimate the risks of CVD and all-cause mortality among patients with new-onset type 2 diabetes, compared with control subjects, according to onset age-groups in a large Chinese cohort study.
Research Design and Methods
Study Participants
The Kailuan Study is an ongoing prospective occupational cohort study conducted in Tangshan, China. All participants in the Kailuan Study are employees and retirees of the Kailuan Group, which is a coal mining company in Tangshan. Details of the study design and procedure have been described elsewhere (12,13). Briefly, from June 2006 to December 2015, 171,415 individuals aged 18–98 years were enrolled to participate in a biennial questionnaire interview and clinical and laboratory examinations at 11 hospitals affiliated with the Kailuan Group. The study was conducted in accordance with the guidelines of the Declaration of Helsinki and was approved by the Kailuan General Hospital Ethics Committee.
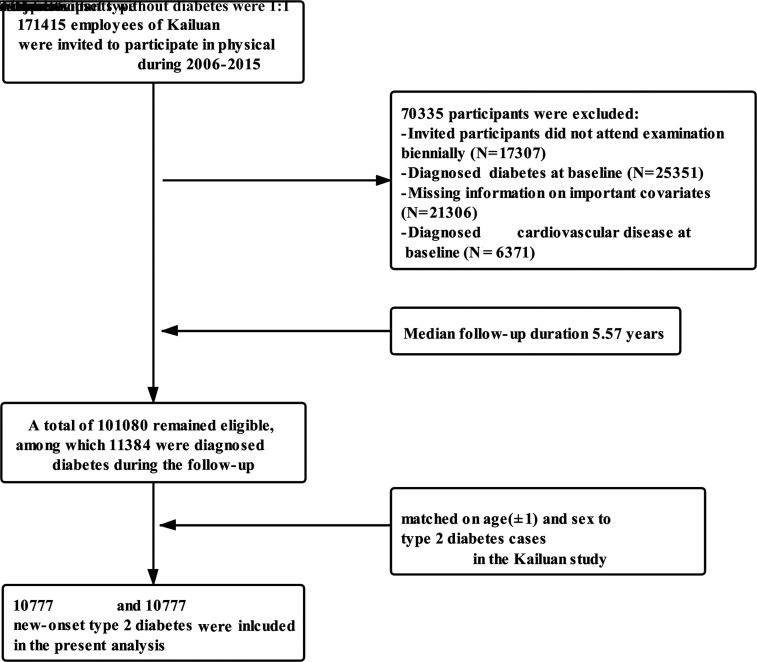
For the current study, we excluded 17,307 participants who did not attend the biennial examination, 25,351 who had diabetes at baseline, 21,306 with missing important covariates (e.g., fasting blood glucose [FBG], history of diabetes, use of hypoglycemic drugs, age, or sex), and 6,371 with a history of CVD at baseline, leaving 101,080 participants who met the inclusion criteria. Of the 101,080 participants free of type 2 diabetes at baseline, 11,384 were diagnosed with type 2 diabetes during follow-up. The date of type 2 diabetes onset was defined as the date of the examination at which type 2 diabetes was first diagnosed. For each case subject with new-onset type 2 diabetes, one control subject was randomly selected from the participants without diabetes during follow-up who attended the examination in the same year and matched for age (±1 years) and sex. Ultimately, data from 10,777 case-control pairs were analyzed (Fig. 1). The follow-up period started from the date of diagnosis for the case subjects with type 2 diabetes and from the same year for the matched control subjects (14). For example, if type 2 diabetes was first diagnosed in a 50-year-old male participant in 2010, then a control subject was randomly selected from the study population who was male, aged 49–51 years, did not have diabetes during follow-up, and underwent examination in 2010, and both participants were monitored from 2010.
Figure 1.
Flowchart of the current study.
Assessment of New-Onset Type 2 Diabetes
During each examination, venous blood samples were collected from participants after a fast of at least 8 h, and FBG was measured using an Hitachi 7600 auto-analyzer (Hitachi, Tokyo, Japan) at the central laboratory of Kailuan General Hospital. Type 2 diabetes was defined as a FBG level ≥7.0 mmol/L, or treatment with hypoglycemic drugs, or self-reported physician-diagnosed type 2 diabetes (11,15). The numbers and proportions of type 2 diabetes diagnosed by FBG, treatment with hypoglycemic drugs, and self-reported previous diagnosis are reported in Supplementary Table 1.
Outcomes
The main outcomes of our study were incident CVD events (including myocardial infarction and stroke), stroke, and all-cause mortality. Assessment of incident CVD events and all-cause mortality has been previously described in detail (12,13,16). Briefly, potential CVD events were ascertained from the Municipal Social Insurance Institution that covered all study participants, the discharge registers of all 11 Kailuan hospitals, and a questionnaire survey (biennially since 2006). Potential CVD cases were identified on the basis of the ICD-10. For suspected CVD events identified by the ICD-10 and questionnaire, a panel of three experienced physicians reviewed the medical records and adjudicated the cases annually. The definition of myocardial infarction was according to the World Health Organization Multinational Monitoring of Trends and Determinants in Cardiovascular Disease criteria (17). Stroke was diagnosed according to the World Health Organization criteria on the basis of combined neurological signs and symptoms and imaging examinations, including computed tomography scans or MRI (18). Confirmation of death was based on information from local government vital statistics offices. Participants were monitored until 31 December 2017 for all outcomes.
Data Collection
Information on demographic and lifestyle characteristics (age, sex, smoking status, drinking status) and medical history (diabetes, hypertension, and CVD, family history of diabetes, use of antihypertensive and hypoglycemic drugs) was collected via face-to-face interviews using a standard questionnaire and updated every 2 years thereafter, as detailed elsewhere (12). Measurements of height, weight, and blood pressure were conducted by trained physicians, following a standardized protocol. BMI was calculated as weight (kg) divided by height squared (m2). Obesity was defined as a BMI ≥28 kg/m2 (19). Physical activity was defined as aerobic exercise ≥3 times/week, for ≥30 min/session. Hypertension was defined as systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg, use of antihypertensive drugs, or self-reported history of physician-diagnosed hypertension. All participants fasted for at least 8 h, and 5 mL of venous blood was taken on the morning of the physical examination. The levels of FBG, LDL cholesterol (LDL-C), HDL cholesterol (HDL-C), and serum creatinine were measured using a Hitachi 7600 auto-analyzer. The estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration creatinine equation (20).
Statistical Analysis
Case subjects with new-onset type 2 diabetes and matched control subjects were classified into four groups according to onset age as follows: <45 years, 45–54 years, 55–64 years, and ≥65 years. Continuous variables are reported as mean ± SD, and categorical variables as the percentage. The baseline characteristics of the case subjects with new-onset type 2 diabetes and the matched control subjects were compared using the Student t test for continuous variables and the χ2 test for categorical variables. The linear trend for individual factors across type 2 diabetes onset age-groups was conducted by assigning the median value of each onset age-group as a continuous variable in a separate model. A general linear model was used for continuous variables, and a logistic model was used for categorical variables. The P values for trend were calculated using the Wald test.
We calculated the incidence rates (per 1,000 person-years) and cumulative incidence of CVD, stroke, and all-cause mortality among participants with new-onset type 2 diabetes versus control subjects across onset age-groups. Because the proportional hazards assumption was violated in our analysis, we used the weighted Cox regression model (21), not constrained by the proportional hazards assumption, to calculate the average hazard ratios (AHRs) and 95% CIs of incident CVD and all-cause mortality among participants with new-onset type 2 diabetes versus control subjects across onset age-groups. The few cases of myocardial infarction across some type 2 diabetes onset age-groups meant there may not have been adequate statistical power to assess the relative risks of myocardial infarction across type 2 onset age-groups. Therefore, we did not present the results for myocardial infarction in our analysis. The multivariate-adjusted models were further adjusted for smoking status (never- or ever-smoker), drinking status (never- or ever-drinker), hypertension (yes or no), obesity (yes or no), LDL-C (continuous), HDL-C (continuous), physical exercise (<3 or ≥3 times/week), and eGFR (continuous). We used multiple imputation by chained equations to impute missing value for covariates (22).
To assess the robustness of our findings, we performed several sensitivity analyses. First, we excluded outcome events occurring within the first year of follow-up to address the potential reverse causation. Second, to minimize the influence of treatment with hypoglycemic drugs on our results, we excluded participants who were diagnosed with diabetes via treatment with hypoglycemic drugs. Third, we repeated our analyses of incident CVD using Fine-Gray models instead, which can account for noncardiovascular death as a competing risk. All statistical analyses were performed using SAS 9.3 software (SAS Institute, Cary, NC).
Results
Baseline Characteristics
Participants’ baseline characteristics are presented in Table 1. Among 10,777 participants with type 2 diabetes and 10,777 control subjects, 83.1% were men. The mean onset age of type 2 diabetes was 55.8 ± 10.9 years. Compared with control subjects, participants with new-onset type 2 diabetes had higher BMI, LDL-C, and eGFR, lower HDL-C and physical exercise level, and higher prevalence of hypertension, obesity, and family history of diabetes (Table 1). Participants with younger-onset type 2 diabetes had higher BMI, HDL-C, and eGFR, were more likely to be ever-smokers, ever-drinkers, and physically inactive, and had higher prevalence of obesity and family history of diabetes than those with older-onset age (Table 1). It should be noted that for most of these parameters, the differences were very small, albeit statistically significant.
Table 1.
Baseline characteristics of participants
| Variables | New-onset type 2 diabetes | Control subjects | P value | Type 2 diabetes onset age (years) | P for trend | |||
|---|---|---|---|---|---|---|---|---|
| <45 | 45–54 | 55–64 | ≥65 | |||||
| Participants, n | 10,777 | 10,777 | 1,530 | 3,497 | 3,840 | 1,910 | — | |
| Age, years | 55.8 ± 10.9 | 55.8 ± 10.9 | — | 38.2 ± 6.4 | 50.6 ± 2.8 | 59.6 ± 2.8 | 71.6 ± 5.2 | <0.01 |
| Male sex | 83.1 | 83.1 | — | 90.1 | 83.4 | 79.8 | 83.4 | <0.01 |
| BMI, kg/m2 | 26.2 ± 3.4 | 24.8 ± 3.1 | <0.01 | 26.7 ± 3.8 | 26.1 ± 3.3 | 26.2 ± 3.3 | 25.9 ± 3.5 | <0.01 |
| HDL-C, mmol/L | 1.43 ± 0.54 | 1.46 ± 0.46 | <0.01 | 1.42 ± 0.60 | 1.46 ± 0.56 | 1.41 ± 0.50 | 1.40 ± 0.49 | <0.01 |
| LDL-C, mmol/L | 2.8 ± 0.9 | 2.7 ± 0.9 | <0.01 | 2.75 ± 0.97 | 2.77 ± 0.91 | 2.91 ± 0.96 | 2.90 ± 0.89 | <0.01 |
| eGFR, mL/min/1.73 m2 | 89.1 ± 23.6 | 88.3 ± 20.6 | <0.01 | 101.0 ± 28.5 | 91.8 ± 22.1 | 87.7 ± 20.8 | 77.6 ± 21.6 | <0.01 |
| Obesity | 26.7 | 14.3 | <0.01 | 34.8 | 25.3 | 25.9 | 24.3 | <0.01 |
| Ever-smoker | 40.9 | 40.8 | 0.82 | 54.0 | 51.3 | 34.9 | 23.9 | <0.01 |
| Ever-drinker | 42.4 | 43.1 | 0.34 | 55.8 | 51.6 | 36.0 | 27.9 | <0.01 |
| Hypertension | 62.9 | 45.3 | <0.01 | 45.2 | 57.8 | 68.5 | 75.2 | <0.01 |
| Physical exercise | 18.2 | 20.0 | <0.01 | 9.4 | 12.1 | 21.8 | 29.3 | <0.01 |
| Family history of diabetes | 4.1 | 2.4 | <0.01 | 7.2 | 5.6 | 3.1 | 1.2 | <0.01 |
Data are presented as mean ± SD or percentages. Characteristics were assessed in the examination cycle when new-onset diabetes was first identified.
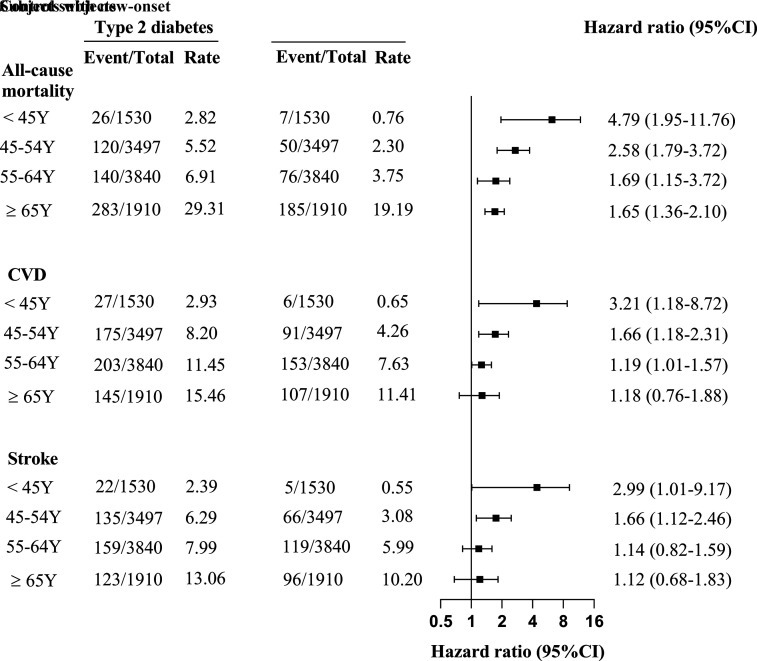
CVD and Mortality
During a median of 5.57 years (119,409 person-years) of follow-up, we documented 1,794 incident events (907 CVD events, of which were 725 strokes, and 887 deaths). The number of missed visits is reported in Supplementary Table 2. The incidence rates per 1,000 person-years of CVD, stroke, and all-cause mortality among participants with new-onset type 2 diabetes versus control subjects across onset age-groups are presented in Fig. 2. We also graphically illustrated the cumulative incidence of CVD, stroke, and all-cause mortality in Supplementary Fig. 1.
Figure 2.
AHRs (95% CIs) for incident CVD and all-cause mortality among patients with new-onset type 2 diabetes versus control subjects, across age-groups. The rate is per 1,000 person-years. All models were adjusted for smoking status, drinking status, hypertension, LDL-C, HDL-C, obesity, eGFR, and physical exercise. Y, years of age.
After adjustment for smoking status, drinking status, hypertension, LDL-C, HDL-C, obesity, eGFR, and physical exercise, participants with new-onset type 2 diabetes were at a higher risk of CVD events and all-cause mortality relative to their matched control subjects across onset age-groups, although some of the differences were not statistically significant. For all-cause mortality, there was a significant increase for all age-groups, and that for CVD it was significantly higher in all but the oldest age-group. Participants with type 2 diabetes onset age <45 years had the highest relative risks for the study outcomes, with adjusted AHRs of 3.21 (95% CI 1.18–8.72) for CVD, 2.99 (95% CI 1.01–9.17) for stroke, and 4.79 (95% CI 1.95–11.76) for all-cause mortality. Additionally, the incremental risks gradually decreased with each 10-year increase of onset age. The corresponding AHRs of CVD and all-cause mortality were 1.66 (95% CI 1.18–2.31) and 2.58 (95% CI 1.79–3.72) for age 45–54 years, 1.19 (95% CI 1.01–1.57) and 1.69 (95% CI 1.15–2.10) for age 55–64 years, and 1.18 (95% CI 0.76–1.88) and 1.65 (95% CI 1.36–2.10) for age ≥65 years, respectively (Fig. 2).
The distribution of causes of death among participants with type 2 diabetes and matched control subjects is presented in Supplementary Fig. 2. The numbers and proportions of CVD, cancer, respiratory diseases, other, and unknown causes of deaths were 170 (29.9%), 131 (23.0%), 33 (5.8%), 88 (15.5%), and 147 (25.8%), respectively, in the case subjects with type 2 diabetes, and 86 (27.0%), 74 (23.3%), 19 (6.0%), 46 (14.5%), and 93 (29.3%), respectively, in the matched control subjects.
Sensitivity Analyses
In the sensitivity analyses, the risks of incident CVD and all-cause mortality among participants with new-onset type 2 diabetes versus control subjects across all onset age-groups remained consistent after excluding participants with outcome events within the first year of follow-up (Supplementary Table 3) or excluding participants receiving treatment with hypoglycemic drugs (Supplementary Table 4). To account for the competing risk of mortality, we conducted a competing risk model to evaluate the relationship between type 2 diabetes onset age and CVD, and the results were similar to main results (Supplementary Table 5).
Conclusions
In the current study, we found that participants with type 2 diabetes diagnosed at age <45 years were at the highest relative risks of CVD and all-cause mortality compared with age- and sex-matched control subjects. Furthermore, the relative risks of CVD and all-cause mortality gradually decreased as the onset age of type 2 diabetes increased by one decade.
To date, only limited data are available for the effects of age at diagnosis on CVD and mortality in people with type 2 diabetes. A cross-sectional study using data from the Australian National Diabetes Audit (ANDA) reported that people diagnosed with type 2 diabetes at an older age were more likely to have macrovascular complications (23) by virtue of their older age. Another Australian study indicated that younger-onset type 2 diabetes was associated with an increased risk of premature death, especially from CVD (8), but this study lacked access to the control subjects and did not consider nonfatal outcomes. In addition, using only two onset age-groups, data from the China National HbA1c Surveillance System (CNHSS) showed a higher risk of nonfatal CVD in people with young-onset versus late-onset type 2 diabetes (7). Moreover, in a study from Hong Kong, young-onset type 2 diabetes was associated with an increased risk of cardiovascular-renal complications compared with late-onset type 2 diabetes at any given age (9), whereas the association became nonsignificant when further adjusted for type 2 diabetes duration. These studies, however, mainly focused on participants with prevalent type 2 diabetes and did not start follow-up at the time of diagnosis. In the current study, new-onset type 2 diabetes occurred during the follow-up period, which might reduce the impact of potential prevalence–incidence bias. In line with our results, a more recent study conducted by Sattar et al. (11) reported that people with younger-onset type 2 diabetes had higher risk for mortality and CVD outcomes compared with age-, sex-, and county-matched control subjects, but potential confounding factors were not adjusted for. Sattar et al. (11) also observed a higher risk of heart failure in younger-onset type 2 diabetes, and this has been recently reported to be an important and frequent complication of type 2 diabetes (24,25). In the current study, we did not consider heart failure as an outcome.
Although the underlying mechanisms for higher risks of CVD events and all-cause mortality among participants with younger-onset type 2 diabetes remain unclear, our findings are biologically plausible. Accumulating evidence supports that type 2 diabetes in younger people has a more rapid deterioration of β-cell function than is seen in later-onset type 2 diabetes (26–28). This loss of β-cell function might result in higher systolic blood pressure and LDL-C concentrations due to increased oxidative stress and activation of the renin-angiotensin system, which would accelerate atherosclerosis and increase the risk of CVD (29–31). Another possible explanation for our findings is that individuals with younger-onset type 2 diabetes are likely to be obese and have higher blood glucose levels, poorer glycemic control, and lower adherence to therapy compared with those who were diagnosed at an older age (6,32,33), which in turn led to greater relative increases in CVD and all-cause mortality risks.
The findings of the current study suggest that preventive measures against CVD are needed in the populations with younger-onset type 2 diabetes, especially for those <45 years of age. Over the past three decades, the prevalence of young-onset diabetes has dramatically increased in China, resulting from increases in sedentary behavior and a suboptimal diet (2,34). Several major studies have shown that lifestyle interventions in people with impaired glucose tolerance can prevent and/or delay the onset of type 2 diabetes until older age and reduce the incidences of CVD events and all-cause mortality (35–38). Therefore, more intensive lifestyle modification should be actively encouraged among people younger-onset type 2 diabetes, including regular physical activity, healthy eating patterns, and weight loss. Our study also provided valuable clinical implications. Previous studies have reported that patients with type 2 diabetes can benefit considerably from intensive therapy for the prevention of CVD and death (39,40). Thus, there is an urgent need to introduce measures to promote the early intensive management of patients with type 2 diabetes.
The current study has several strengths. This is a large prospective study conducted to investigate the effect of type 2 diabetes onset age on CVD and all-cause mortality by tracking people from the time of diagnosis in China. In addition, we included age- and sex-matched control subjects without diabetes, which could fully consider and reduce the effects of such confounding factors. Moreover, the entire study population was covered by the Municipal Social Insurance Institution, the hospitals’ discharge register, and the biennial medical examinations, which enabled us to track the outcome events in all participants.
However, we also acknowledge several limitations in our study. First, the diagnosis of type 2 diabetes was based on a single measurement of FBG rather than oral glucose tolerance testing or the measurement of hemoglobin A1c, and therefore the incidence of type 2 diabetes might have been underestimated.
Second, we did not distinguish between type 1 and type 2 diabetes in our study. However, according to the Chinese clinical guideline for preventing diabetes (4), type 2 diabetes represents 95% of all cases of diabetes. In addition, the average age at the diagnosis of diabetes was 55.8 years in our study, so misclassification of other types of diabetes was minimal. Moreover, similar results from sensitivity analysis excluding patients being treated with hypoglycemic drugs can be used to strengthen the case that our cohort is mostly type 2 diabetes, because it is unlikely that many people with type 1 diabetes are not using any drugs.
Third, although we adjusted for a variety of factors, residual confounders may still exist.
Fourth, the onset age of type 2 diabetes was calculated as the date of the physical examination when diabetes was first diagnosed minus the patient’s birth date, which have slightly differed from the actual age at diagnosis. However, participants in our study underwent physical examination biennially; therefore, discrepancies in the onset age would not have a meaningful influence on the results.
Fifth, some causes of death could not be ascertained due to the lack of a medical diagnosis and were coded as “unknown” in our study. Given that the main outcome of our study was all-cause mortality, we believe that this would not affect the overall conclusion regarding the importance of the age of onset of diabetes.
Finally, all participants were employees and retirees of the Kailuan Group, and most of them were men; thus, the generalizability of the results is relatively limited.
Conclusion
In summary, the relative risks of CVD and all-cause mortality differ across the age at diagnosis of type 2 diabetes, and the associations were more evident in participants with type 2 diabetes diagnosed at a younger age. Identification and quantification of the increased risk of CVD and all-cause mortality conferred by younger-onset type 2 diabetes may allow risk stratification of people early in the condition and thus provide greater opportunities for interventions (such as intensive therapy and lifestyle interventions) to reduce risk of complication-related morbidity and mortality for this increasing population with young-onset type 2 diabetes.
Article Information
Acknowledgments. The authors thank all the survey teams of the Kailuan Study Group for their contribution and the study participants who contributed their information.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. M.Z. performed the statistical analysis. M.Z., L.So., L.Su., M.W., C.W., S.Y., Y.L., C.Y., S.Z., Z.H., and Y.S. interpreted data. M.Z. and L.So. interpreted the findings and drafted the manuscript. S.W. and H.X. designed and supervised the study. All authors reviewed the manuscript, edited it for intellectual content, and gave final approval for this version to be published. L.So., S.W., and H.X. are the guarantors of this work and, as such, had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains supplementary material online at https://doi.org/10.2337/figshare.14173313.
M.Z. and L.So. contributed equally to the study.
References
- 1. Zhong XL. Diabetes mellitus survey in China. Chin Med J (Engl) 1982;95:423–430 [PubMed] [Google Scholar]
- 2. Li Y, Teng D, Shi X, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ 2020;369:m997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. International Diabetes Federation . IDF Diabetes Atlas, 9th edition, 2019. Accessed 18 November 2019. Available from https://www.diabetesatlas.org/en/
- 4. Chinese Diabetes Society . Clinical guideline for prevention and treatment of type 2 diabetes in China. Chinese J Diabetes 2014;22:2–42 [Google Scholar]
- 5. Magliano DJ, Sacre JW, Harding JL, Gregg EW, Zimmet PZ, Shaw JE. Young-onset type 2 diabetes mellitus - implications for morbidity and mortality. Nat Rev Endocrinol 2020;16:321–331 [DOI] [PubMed] [Google Scholar]
- 6. Steinarsson AO, Rawshani A, Gudbjörnsdottir S, Franzén S, Svensson AM, Sattar N. Short-term progression of cardiometabolic risk factors in relation to age at type 2 diabetes diagnosis: a longitudinal observational study of 100,606 individuals from the Swedish National Diabetes Register. Diabetologia 2018;61:599–606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Huo X, Gao L, Guo L, et al. Risk of non-fatal cardiovascular diseases in early-onset versus late-onset type 2 diabetes in China: a cross-sectional study. Lancet Diabetes Endocrinol 2016;4:115–124 [DOI] [PubMed] [Google Scholar]
- 8. Huo L, Magliano DJ, Rancière F, et al. Impact of age at diagnosis and duration of type 2 diabetes on mortality in Australia 1997-2011. Diabetologia 2018;61:1055–1063 [DOI] [PubMed] [Google Scholar]
- 9. Chan JC, Lau ES, Luk AO, et al. Premature mortality and comorbidities in young-onset diabetes: a 7-year prospective analysis. Am J Med 2014;127:616–624 [DOI] [PubMed] [Google Scholar]
- 10. Nanayakkara N, Curtis AJ, Heritier S, et al. Impact of age at type 2 diabetes mellitus diagnosis on mortality and vascular complications: systematic review and meta-analyses. Diabetologia 2021;64:275–287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sattar N, Rawshani A, Franzén S, et al. Age at diagnosis of type 2 diabetes mellitus and associations with cardiovascular and mortality risks. Circulation 2019;139:2228–2237 [DOI] [PubMed] [Google Scholar]
- 12. Zhang Q, Zhou Y, Gao X, et al. Ideal cardiovascular health metrics and the risks of ischemic and intracerebral hemorrhagic stroke. Stroke 2013;44:2451–2456 [DOI] [PubMed] [Google Scholar]
- 13. Wu S, An S, Li W, et al. Association of trajectory of cardiovascular health score and incident cardiovascular disease. JAMA Netw Open 2019;2:e194758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang C, Yuan Y, Zheng M, et al. Association of age of onset of hypertension with cardiovascular diseases and mortality. J Am Coll Cardiol 2020;75:2921–2930 [DOI] [PubMed] [Google Scholar]
- 15. Fox CS, Golden SH, Anderson C, et al.; American Heart Association Diabetes Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Clinical Cardiology, Council on Cardiovascular and Stroke Nursing, Council on Cardiovascular Surgery and Anesthesia, Council on Quality of Care and Outcomes Research; American Diabetes Association . Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care 2015;38:1777–1803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jin C, Chen S, Vaidya A, et al. Longitudinal change in fasting blood glucose and myocardial infarction risk in a population without diabetes. Diabetes Care 2017;40:1565–1572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas AM, Pajak A. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation 1994;90:583–612 [DOI] [PubMed] [Google Scholar]
- 18. Stroke--1989 . Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO Task Force on Stroke and other Cerebrovascular Disorders. Stroke 1989;20:1407–1431 [DOI] [PubMed] [Google Scholar]
- 19. Cooperative Meta-Analysis Group of the Working Group on Obesity in China . Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults--study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci 2002;15:83–96 [PubMed] [Google Scholar]
- 20. Levey AS, Stevens LA, Schmid CH, et al.; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) . A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150:604–612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schemper M, Wakounig S, Heinze G. The estimation of average hazard ratios by weighted Cox regression. Stat Med 2009;28:2473–2489 [DOI] [PubMed] [Google Scholar]
- 22. van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw 2011;45:1–67 [Google Scholar]
- 23. Nanayakkara N, Ranasinha S, Gadowski A, et al. Age, age at diagnosis and diabetes duration are all associated with vascular complications in type 2 diabetes. J Diabetes Complications 2018;32:279–290 [DOI] [PubMed] [Google Scholar]
- 24. Birkeland KI, Bodegard J, Eriksson JW, et al. Heart failure and chronic kidney disease manifestation and mortality risk associations in type 2 diabetes: a large multinational cohort study. Diabetes Obes Metab 2020;22:1607–1618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rawshani A, Rawshani A, Franzén S, et al. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2018;379:633–644 [DOI] [PubMed] [Google Scholar]
- 26. Zhou S, Meng X, Wang S, et al. A 3-year follow-up study of β-cell function in patients with early-onset type 2 diabetes. Exp Ther Med 2016;12:1097–1102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. TODAY Study Group . Effects of metformin, metformin plus rosiglitazone, and metformin plus lifestyle on insulin sensitivity and β-cell function in TODAY. Diabetes Care 2013;36:1749–1757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. RISE Consortium; RISE Consortium Investigators . Effects of treatment of impaired glucose tolerance or recently diagnosed type 2 diabetes with metformin alone or in combination with insulin glargine on β-cell function: comparison of responses in youth and adults. Diabetes 2019;68:1670–1680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chehade JM, Gladysz M, Mooradian AD. Dyslipidemia in type 2 diabetes: prevalence, pathophysiology, and management. Drugs 2013;73:327–339 [DOI] [PubMed] [Google Scholar]
- 30. Liguori A, Abete P, Hayden JM, et al. Effect of glycaemic control and age on low-density lipoprotein susceptibility to oxidation in diabetes mellitus type 1. Eur Heart J 2001;22:2075–2084 [DOI] [PubMed] [Google Scholar]
- 31. Chen J, Mehta JL. Interaction of oxidized low-density lipoprotein and the renin-angiotensin system in coronary artery disease. Curr Hypertens Rep 2006;8:139–143 [DOI] [PubMed] [Google Scholar]
- 32. TODAY Study Group, Zeitler P, Hirst K, Pyle L, et al. A clinical trial to maintain glycemic control in youth with type 2 diabetes. N Engl J Med 2012;366:2247–2256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nanayakkara N, Pease AJ, Ranasinha S, et al. Younger people with Type 2 diabetes have poorer self-care practices compared with older people: results from the Australian National Diabetes Audit. Diabet Med 2018;35:1087–1095 [DOI] [PubMed] [Google Scholar]
- 34. Xu Y, Wang L, He J, et al.; 2010 China Noncommunicable Disease Surveillance Group . Prevalence and control of diabetes in Chinese adults. JAMA 2013;310:948–959 [DOI] [PubMed] [Google Scholar]
- 35. Gong Q, Zhang P, Wang J, et al.; Da Qing Diabetes Prevention Study Group . Morbidity and mortality after lifestyle intervention for people with impaired glucose tolerance: 30-year results of the Da Qing Diabetes Prevention Outcome Study. Lancet Diabetes Endocrinol 2019;7:452–461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Knowler WC, Barrett-Connor E, Fowler SE, et al.; Diabetes Prevention Program Research Group . Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Lindström J, Ilanne-Parikka P, Peltonen M, et al.; Finnish Diabetes Prevention Study Group . Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet 2006;368:1673–1679 [DOI] [PubMed] [Google Scholar]
- 38. Herman WH, Hoerger TJ, Brandle M, et al.; Diabetes Prevention Program Research Group . The cost-effectiveness of lifestyle modification or metformin in preventing type 2 diabetes in adults with impaired glucose tolerance. Ann Intern Med 2005;142:323–332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 2008;358:580–591 [DOI] [PubMed] [Google Scholar]
- 40. Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 2008;359:1577–1589 [DOI] [PubMed] [Google Scholar]