FIGURE 2.
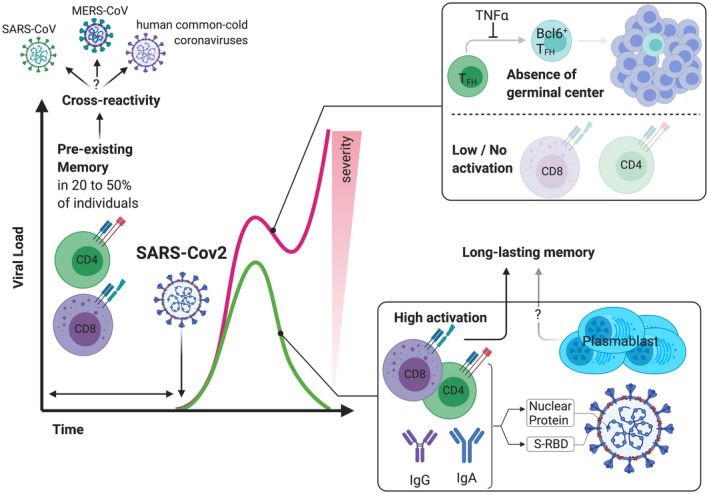
Differential T and B cell immune responses lead to a wide‐range of clinical outcome in patients with COVID‐19. SARS‐CoV‐2 infection results in a lymphopenia and especially of CD4 and CD8 lymphopenia. The control of many virus requires usually 7 to 10 days to mount an effective T cell immune response, and this is typically a critical time for COVID‐19 patients regarding development of severe disease or resolution of viral infection. The ability to generate SARS‐CoV‐2 specific T cell responses and to mount a humoral response (with up to 30% of plasma cells among B cells) has been associated with the ability to clear viral infection whereas patients with severe form of COVID‐19 exhibit low activation of CD4/CD8 T cells and a defect in the differentiation of TFH to Bcl6+ TFH that results in an inability to form germinal center. The CD4 and CD8 specific SARS‐CoV‐2 T cell response is often correlated with the titer of SARS‐CoV‐specific antibodies and protective memory T cells were still detectable even when humoral responses vanished. Finally, pre‐existing SARS‐CoV‐2 specific T cell memory is widely observed in the general population (20 to 50% of patients who had not been infected) suggesting a high cross‐reactivity of T cell responses
