Abstract
Background
The United Kingdom entered ‘lockdown’ on the 23 March 2020 due to the COVID‐19 pandemic. This resulted in school closures forcing children to remain at home. Dental‐facial trauma was still likely to be common place due to falls and injuries exercising. The aim of this study was to explore the impact of the COVID‐19 pandemic on clinical practice in a paediatric population in a tertiary care hospital and a linked Dental Institute.
Method
A proforma was designed to capture the demographics, presenting complaints, type of dental‐facial injury, treatment need and the treatment received for all paediatric patients presenting face to face with dental‐facial trauma to King's College Hospital during the ‘lockdown’ period (23 March‐ 14 June 2020).
Results
Four hundred and twenty calls were triaged, converting to 102 patients seen face‐to‐face for dental‐facial trauma. The remainder were able to be triaged ‘virtually’. Injuries seen included 56 (54.9%) dentoalveolar injuries, 37 (36.2%) lacerations, five (4.9%) suspected facial fractures and four (3.9%) dog bites. Males and females were equally affected. The majority of incidents occurred in the home environment (n = 60, 58.8%), with the remainder (n = 42, 41.2%) occurring outside the home environment. The main causes of dental‐facial trauma were falls (n = 47, 46.1%) and bicycles/scooters (n = 29, 28.4%). The most common type of dentoalveolar injury was lateral luxation (n = 15, 26.7%), followed by avulsion (n = 12, 21.4%). Only one child required treatment under general anaesthesia (GA).
Conclusion
The demographic, presenting complaints and treatment needs of patients who presented during the lockdown period with dental‐facial trauma were unusual. The overwhelming majority were able to be treated without the use of GA. The attendance protocol in a tertiary care setting and the use of ‘teledentistry’ ensured only the most severe trauma cases were seen. This highlights how more complex trauma can still occur during ‘lockdown’ and requires immediate management.
Keywords: COVID‐19, dental‐facial, paediatric, trauma
1. INTRODUCTION
The COVID‐19 pandemic has had a profound impact upon daily life around the world. The announcement by the United Kingdom (UK) government of a ‘lockdown’ on 23 March 2020 resulted in the closure of all non‐essential shops and businesses as the public were advised to ‘stay at home, protect the National Health Service (NHS), save lives’, to limit the spread of the virus. The result of this led to a significant decrease in Emergency Department attendances throughout the ‘lockdown’ period. 1 Given the nature of the stay at home advice, this was to be expected. However, there was concern from many quarters that dental‐facial trauma would occur as a result of possible domestic violence. 2 Furthermore, as traumatic dental‐facial injuries occur more often in the home in younger cohorts of patients (up to 60% of primary tooth injuries in some reported studies) 3 lockdown was unlikely to result in a decrease in the numbers of traumatic dental‐facial injuries requiring treatment. In addition, in the UK, people were still allowed one period of daily exercise outside of the household, meaning injuries from running, bicycles and scooters were still likely to occur.
Throughout the UK, there was an agreed consensus upon the management of general, acute paediatric emergencies. 4 Specific guidance for dental trauma was developed by numerous societies including the Royal College of Surgeons (RCS), 5 the Scottish Dental Clinical Effectiveness Programme (SDCEP) 6 and Dental Trauma UK in conjunction with the British Society of Paediatric Dentistry. 7 These guidelines varied, with some advocating that patients should be seen for all traumatic injuries and others attempting to mitigate the risk of patient attendance (and possible contraction of COVID‐19) against the benefit of receiving immediate treatment. This inevitably led to some compromise in treatment—for example normal follow‐ups regarding splint removal and radiographs may have been delayed and instead conducted virtually. Many units treating acute dental trauma therefore developed their own local policies designed to safeguard the well‐being of staff and patients, whilst still ensuring those with the most acute need could be seen and treated. 8 King's College Hospital (KCH) operated an initial telephone triage and ‘virtual’ service, to ensure that patients were not being seen face to face unnecessarily. This was followed by virtual or telephone reviews to again prevent unnecessary attendance whilst still ensuring patients with dental‐facial trauma were adequately followed up.
Due to staff redeployment and the overwhelming demand for hospital services during the peak of the pandemic, there was a minimization of the use of general anaesthetic (GA) services in both the dental and main hospitals at KCH, and no sedation services were available in the paediatric emergency department of the main hospital. This led to dental trauma being redirected during normal working hours to the paediatric dental department where the use of inhalation sedation was more readily available.
To date, there are no papers that have reported the impact of COVID 19 on the paediatric population from oral and maxillofacial and paediatric dentistry perspectives. Hence, the aim of this service evaluation was to explore the impact of the COVID‐19 pandemic on clinical practice in a paediatric population in a tertiary care hospital with a level 1 trauma status (KCH) and a linked dental institute. This study was registered with the trust governance team.
2. MATERIALS AND METHOD
Data were collected prospectively from the beginning of ‘lockdown’ (23 March 2020) to the easing of lockdown restrictions (14 June 2020). During this time period, the details of any paediatric patient (under 16 years of age) presenting to King's College Hospital with dental‐facial trauma were recorded.
Patients were identified from the clinical notes in the Dental Institute if they presented in normal ‘9–5’ working hours to the paediatric dental team. Those presenting ‘out of hours’ to the oral and maxillofacial team were identified using the emergency department electronic database. Most patients presenting with dental trauma during normal working hours had been triaged by telephone by a member of the paediatric dental team using the Scottish Dental Clinical Effectiveness Programme guidance, which patients accessed through calling the NHS 111 service. The NHS 111 service is a 24 hour, 7 days a week, free to call, urgent but non‐emergency medical helpline which runs in England, Scotland and parts of Wales. It is staffed by medical practitioners, nurses and paramedics who can provide advice or they direct patients to the nearest medical centre. Those attending with dental‐facial lacerations or other facial trauma presented face to face as usual in the paediatric emergency department.
Data were recorded prospectively using a data collection sheet to highlight the ages of patients attending, their main complaint, location and mechanism of injury, treatment which was completed and the treatment modality. These were verified against the emergency department electronic database.
Patients who presented with pain and infection of a dentoalveolar origin were excluded as this was analysed in a separate service evaluation. Data were analysed with descriptive statistics using Microsoft Excel (2020).
3. RESULTS
During the 8‐week ‘lockdown’ period, over 420 telephone calls were triaged for paediatric dental‐facial emergencies. This converted to 171 (40%) face‐to‐face appointments, of which 102 patients presented with dental‐facial trauma.
Injuries included 56 (54.9%) dentoalveolar injuries, 37 (36.2%) lacerations, 5 (4.9%) suspected facial fractures and 4 (3.9%) dog bites.
There was a relatively even gender spread with 47 (46.1%) females and 55 (53.9%) males. The age ranged from 1 to 16 years. There did not appear to be any variation in the trauma presentation in relation to the time of the ‘lockdown period’.
Most patients (n = 87, 85.2%) were fit and well. Other notable conditions included: epilepsy (n = 2, 1.9%), asthma (0.9%, n = 1), learning difficulties (n = 1, 0.9%) and autism (n = 1, 0.9%). The majority of incidents occurred in the home or garden (n = 60, 58.8%), with the remainder (n = 42, 41.2%) occurring outside of the home. The main causes of dental‐facial trauma were falls (n = 47, 46.1%) and bicycles, scooters and skateboards (n = 29, 28.4%).
Just under half (48%) of the trauma patients accessed care through the paediatric emergency department. The full range of presentations is shown in Table 1. The most common presentation of the dental‐facial paediatric trauma was dentoalveolar trauma (n = 56, 54.9%). There was a relatively equal gender predisposition with 55.3% (n = 31) of dentoalveolar injuries sustained by females in comparison to males (n = 25, 44.6%). The average age of patients presenting with a dentoalveolar injury was nine years.
TABLE 1.
How patients accessed the urgent dental services
| Paediatric Emergency Department | 48% |
| Via NHS 111 (phone triage) | 36% |
| Referred from other secondary care units | 9% |
| Referred by GDP/booked review | 7% |
Most cases of dentoalveolar trauma were treated in the paediatric dental department during normal working hours (n = 38, 67.8%), with the remainder (n = 18, 32.2%) treated in the paediatric emergency department.
The majority of patients (n = 41, 73%) sustained injury to the anterior teeth with 69% (n = 39) in the maxillary arch.
Over half of the patients (n = 30, 53.5%) suffered trauma in the home environment, with the remainder (n = 26, 46.4%) occurring outside of the home.
In terms of the mechanism of injury, 27 (48.2%) involved a fall or a trip, 15 (26.7%) involved a scooter or bicycle, 3 (5.6%) involved an alleged assault and a further 6 (10.7%) involved an exercise regime. Other mechanisms included water ‘fights’ and seizures (Table 2).
TABLE 2.
Number of patients presenting with dentoalveolar trauma, the place of occurrence and the cause of injury
| Home and garden | Outside the home environment | Total | |
|---|---|---|---|
| Cause of injury | |||
| Fall | 15 (26.7%) | 12 (21.4%) | 27 (48.2%) |
| Scooter/Bike | 6 (10.7%) | 9 (16.1%) | 15 (26.7%) |
| Exercise /Sport | 4 (7.1%) | 2 (3.6%) | 6 (10.7%) |
| Alleged assault | 0 | 3 (5.4%) | 3 (5.4%) |
| Seizure | 1 (1.8%) | 0 | 1 (1.8%) |
| Eating (orthodontic) | 2 (3.6%) | 0 | 2 (3.6%) |
| Water fight | 1 (1.8%) | 0 | 1 (1.8%) |
| Siblings play fighting | 1 (1.8%) | 0 | 1 (1.8%) |
| Total | 30 (53.6%) | 26 (46.4%) | 56 |
Trauma to the primary dentition accounted for 26.8% (n = 15) of all cases, with the remainder (n = 41, 73.2%) being permanent teeth. The most common type of injury was lateral luxation (n = 15, 26.7%), followed by avulsion (n = 12, 21.4%), of which 11 were in the permanent dentition. Complicated crown fractures (n = 12) made up 21.4% of dentoalveolar trauma, along with enamel/dentine fractures (n = 9, 16%). Four patients (7.1%) had extrusion and 3.5% (n = 2) presented with intrusion.
The majority (48%) of dentoalveolar injuries required local anaesthetic (LA) to manage the injury. The rest were managed without local anaesthetic (dressings placed) or were treated using topical anaesthesia and non‐pharmacological behavioural management techniques. One patient (aged 1‐year) was swaddled in a blanket with consent from the parents to extract a mobile maxillary primary tooth following a fall. Unusually for this patient demographic group, only one patient required an urgent general anaesthetic for extraction of a complicated crown fracture of a primary maxillary central incisor. This was completed on the first day of the ‘lockdown’ period before the peak of the pandemic (Figure 1).
FIGURE 1.
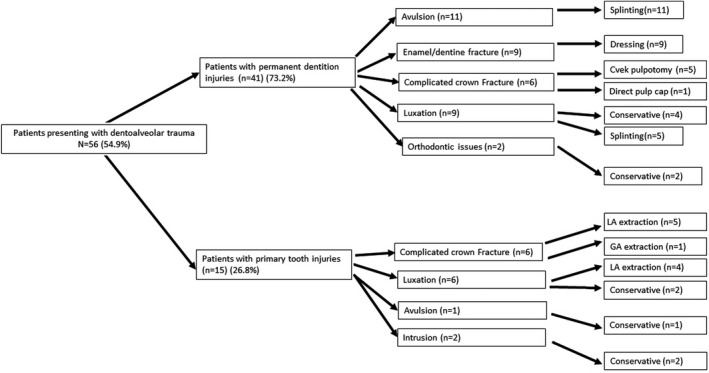
Type of dentoalveolar trauma and the treatment of each injury
In terms of follow‐up, 26 (46.4%) patients were followed up by the paediatric dental/OMFS teams, with the initial follow‐up being ‘virtual’. The remainder were followed up by the patients General Dental Practitioners (GDP).
Thirty‐seven (36.2%) patients suffered lacerations during the ‘lockdown period’. Over double the number of males suffered lacerations (n = 25, 67.6%) compared with their female counterparts (n = 12, 32.4%). The average age of patients with lacerations was five years. The majority of lacerations occurred at home or in the garden at home (n = 26, 70.3%), with the remainder (n = 11, 29.7%) sustained outside of the home, usually at a park. The majority of the lacerations were due to falls (n = 20, 54.1%) with the remainder (n = 12, 32.4%) largely occurring from incidences involving bicycles, scooters and skateboards.
Out of 37 lacerations, 20 (54.1%) were treated conservatively, with simple debridement and dressings (n = 12, 32.4%) or steri‐stripping and/or gluing (n = 8, 21.6%). The remaining 17 (45.9%) underwent debridement and suturing under local anaesthetic with the assistance of pre‐anaesthetic topical lignocaine, adrenaline and tetracaine (LAT) gel. All treatment under local anaesthetic was successful (Figure 2). No patients required a general anaesthetic to manage lacerations.
FIGURE 2.
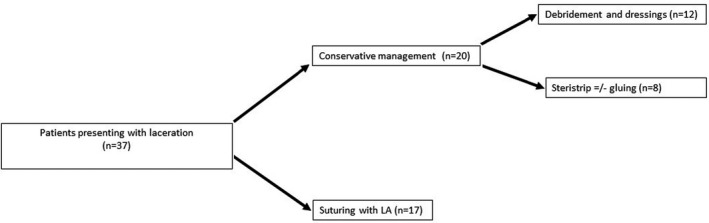
Number of patients presenting with lacerations and their management
Four patients had dog bites. The youngest was five years of age and the eldest was 15 years old. All of these bites were by their own dogs at home. There was an equal gender distribution for males (n = 2, 50%) and females, with average age of nine years. The majority (n = 3, 75%) were treated with wash‐out and debridement under local anaesthetic and they were given a seven day course of antibiotics. One patient with a small bite was managed conservatively. All were followed up remotely by telephone and no patients reported subsequent problems.
There were five patients who had suspected facial fractures of which the majority were male (n = 3), with an average age of 14 years. Two of the cases (one female and one male) were alleged assaults, two were bicycle injuries (one female and one male) and one male was concerned after a fall that he had a facial fracture due to headaches. All of these occurred outside of the home. Four patients had no confirmed fracture on imaging. One of these was followed up virtually and one face to face in the clinic. One patient presented with a condyle fracture which was treated conservatively and followed up in the clinic (face to face). This meant that no patients required operative surgical intervention.
4. DISCUSSION
These data highlight the wide range of presentations of dental‐facial trauma within the paediatric cohort throughout the ‘lockdown’ period. In terms of the causes of the trauma, falling (46.1%), followed by bicycles, scooters and skateboards (28.4%) were the most common. As expected due to ‘lockdown’ and government advice to only leave the home for essential visits, the majority of all injuries (58.8%) occurred within the home environment, with the remainder (41.2%) outside of the home. This occurrence is higher than worldwide prevalence trends, which previously have shown that 47% of traumatic dental injuries occurred within the home. 9 This is likely due to the effect of ‘lockdown’ meaning more people remained at home.
Interestingly in this cohort, a larger number of injuries than may have been expected occurred outside of the home environment. This may be because people in the UK were still allowed outside for daily exercise. If children had been at home for the majority of the ‘lockdown’ period, they may have then been over zealous in their activities once they were allowed to leave the home, leading to a sustained level of dental trauma. Furthermore, this was likely encouraged by parents in order to ensure children were still benefiting from physical activities. At school, children would more likely benefit from a more structured day with less opportunity for traumatic dental‐facial injuries to occur. Anecdotally, the abnormally warm British summer may have contributed to more injuries outside of the home environment, with May 2020 being the sunniest month on record. 10
There was also a large number of injuries from bicycles and scooters, with no injuries from team sports as is usually expected in an adolescent cohort. This is again likely due to the cancellation of all team sports in ‘lockdown’. 11
The overwhelming majority of patients were fit and well (85.2%). This can possibly be attributed to those who were medically compromised ‘shielding’ and not leaving the household, and parents being cautious and seeking appropriate telephone advice before attending face‐to‐face appointments unnecessarily.
The majority of injuries seen were to the permanent dentition (73.2%). Fewer injuries to the primary teeth were seen in face‐to‐face appointments. This may be due to more primary tooth injuries being triaged ‘virtually’ and managed by advice only, as per previously mentioned published guidelines. Ordinarily, the majority of permanent dental injuries would be expected to present due to sports injuries or injuries outside of the home. Given the ‘lockdown’ period and the closure of schools, more injuries to the permanent dentition occurred at home.
Interestingly in this cohort, the majority of dentoalveolar injuries were more severe than what has previously been reported in the literature, with a higher number of avulsions (19.6% of all dentoalveolar injuries in the permanent dentition) and luxation injuries (26.8%). 12 A likely reason for this is the implementation of a video and telephone triage system meaning that the majority of the less complicated dentoalveolar injuries (those not involving tooth displacement or pulp involvement) were managed with self‐help advice, as the public heeded the warnings to not overwhelm the healthcare system. As primary care providers were also forced to close, this also probably led to secondary care providers, such as King's College Hospital who were selected as ‘urgent care hubs’, to be referred more complex dentoalveolar trauma. 13 This also highlights that in the face of staff redeployment to help manage an increased capacity of COVID positive patients, 14 skilled operators are still required to manage complex acute dental trauma, of which the psychosocial impact for children and parents can have lifelong repercussions. 15 This is a key treatment area which should not be neglected in any future ‘lockdowns’ as dental‐facial trauma continues to present as demonstrated in this cohort.
Four children sustained facial dog bites during the ‘lockdown’ period. All of the dogs were known to the children. This is not unusual in that most children are bitten by dogs known to them. 16 It is likely that children were spending extended periods of time at home with their pets, possibly with a lack of space as families worked from home, leading to increased frustration and an increased likelihood of dog bites.
Previous studies have highlighted how small lacerations can be successfully managed with either gluing or suturing. 17 Interestingly, from these results, even the youngest children did not require general anaesthetics to manage their facial lacerations. In contrast, previously published data has highlighted how up to 50% of children have required a GA to manage their facial lacerations. 18 , 19
Due to the lack of GA facilities at KCH during the peak of the pandemic (due to anaesthetist redeployment, increased fallow times and theatres being used for additional bed capacity), it is likely that clinicians, parents and children were more willing to attempt treatment under LA alone. Furthermore, the risk of additional exposure to the hospital environment carried an enhanced risk of infection.
These findings have had an impact upon practice within the oral and maxillofacial surgery department at King's College Hospital with every clinician more willing to attempt treatment under lignocaine, adrenaline and tetracaine gel and local anaesthetic in the future, possibly freeing up access to GA facilities and decreasing waiting times for treatment. The increased understanding from the public about the current health crisis has meant that parents are also more willing to consent to use of LAT gel 20 and a form of restraint to enable treatment to be completed effectively.
Whenever dental‐facial trauma has occurred clinicians should be mindful of safeguarding concerns. The increased time that children have been spending at home has led to an increase in calls to children's protection charities. 21 In this service, none of the patients who presented during ‘lockdown’ gave cause for concern, but clinicians were still mindful of this. The paediatric dental department has a safeguarding protocol whereby letters are sent to both the general dental practitioner and general medical practitioner informing them of the injury. This communication ensures that any dental injuries, which may feed in to a wider pattern of injuries causing concern, are known to all the relevant healthcare professionals.
It is worth considering the impact that trauma prevention can have on this age group. Whilst paediatric dental‐facial emergencies can present in many different ways, they can occasionally be prevented. 22 The use of helmets for children when riding bicycles and scooters should always be encouraged. If triaging paediatric patients with acute dental‐facial trauma, online aids can occasionally be beneficial in helping to improve outcomes particularly for those with avulsed teeth, if recommended appropriately. 23
The use of ‘teledentistry’ has long been reported in the literature. 24 However, its use recently has increased due to the necessity to reduce patient footfall in the peak of the pandemic whilst still providing patients with adequate care. 25 The NHS has adopted ‘attend anywhere’ virtual, video‐calling clinics which have been implemented by King's College Hospital. All reviews were initially conducted via these virtual clinics. This allowed for close monitoring to ensure that dentoalveolar splints had not debonded and soft tissues were healing adequately, whilst saving both the patient and guardian from an unnecessary visit and possible increased risk of COVID‐19 infection, which has been reported as being as high as 20% in some quarters. 26 Those injuries that were able to be followed up in primary care were discharged with communication to the primary care provider, again to decrease the risk of contracting coronavirus when attending secondary care clinics. It is likely that virtual appointments will continue to be commonplace moving forward, in order to help reduce the burden on clinicians in the light of long waiting lists post‐pandemic and keeping patients footfall to a minimum to adhere to social distancing protocols.
5. CONCLUSION
This study has reported the demographics, presenting complaints and treatment needs of patients who presented to KCH during the ‘lockdown’ period with dental‐facial trauma. The overwhelming majority of these patients were treated successfully without access to GA facilities, with clinicians and parents mindful to not overburden the healthcare system. The use of LAT gel was extremely effective. This study has noted how an effective ‘teledentistry’ system reduced patient footfall ensuring only the more complicated cases were seen. This led to an increase in the severity of dentoalveolar trauma being seen despite the national ‘lockdown’. These results may provide information on emergency resource distribution during future pandemics and ‘lockdowns’ to ensure optimal patient outcomes.
CONFLICT OF INTEREST
The authors confirm that they have no conflict of interest.
AUTHORS CONTRIBUTIONS
K Fan conceived the idea with overall charge of the direction and planning. K Fan, K Howson, E Yeung, L Rayne designed the project. K Howson performed data collection and data analysis. K Fan, K Howson E Yeung & L Rayne involved in data interpretation. K Howson wrote the manuscript with input from K Fan, E Yeung & L Rayne.
Nabeel Ilyas and Alexandra Green are joint first authors, both authors contributed equally to this manuscript.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Health Foundation . Visits to A&E departments in England in April 2020 fell by 57% compared to last year. Available from: https://www.health.org.uk/news‐and‐comment/charts‐and‐infographics/visits‐to‐a‐e‐departments‐in‐england‐in‐april‐2020‐fell‐by‐57. [Accessed 26 August 2020].
- 2. Coulthard P, Hutchison I, Bell JA, Coulthard ID, Kennedy H. COVID‐19, domestic violence and abuse, and urgent dental and oral and maxillofacial surgery care. Br Dent J. 2020;228:923–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bastone EB, Freer TJ, McNamara JR. Epidemiology of dental trauma: a review of the literature. Aust Dent J. 2000;45:2–9. [DOI] [PubMed] [Google Scholar]
- 4. Royal College of Paediatrics and Child Health . COVID‐19‐ guidance for paediatric services. Available from: https://www.rcpch.ac.uk/resources/covid‐19‐guidance‐paediatric‐services. [Accessed 26 August 2020].
- 5. Royal College of Surgeons England . Recommendations for Paediatric Dentistry during COVID‐19 pandemic. Available from: https://www.rcseng.ac.uk/dental‐faculties/fds/coronavirus/. [Accessed 26 August 2020].
- 6. Scottish Dental Clinical Effectiveness Programme . Management of acute dental problems during COVID‐19 pandemic. Available from: https://www.sdcep.org.uk/wp‐content/uploads/2020/03/SDCEP‐MADP‐COVID‐19‐guide‐300320.pdf. [Accessed 26 August 2020].
- 7. Dental Trauma UK . Permanent/primary dentition acute management of traumatic injuries and follow‐up care during the COVID‐19 pandemic. Available from: https://www.dentaltrauma.co.uk/Index.aspx. [Accessed 26 August 2020].
- 8. Ilyas N, Agel M, Mitchell J, Sood S. COVID‐19 pandemic: the first wave ‐ an audit and guidance for paediatric dentistry. Br Dent J. 2020;228:927–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Azami‐Aghdash S, Ebadifard Azar F, Pournaghi Azar F, Rezapour A, Moradi‐Joo M, Moosavi A, et al. Prevalence, etiology, and types of dental trauma in children and adolescents: systematic review and meta‐analysis. Med J Islam Repub Iran. 2015;29:234. [PMC free article] [PubMed] [Google Scholar]
- 10. Madge G. May 2020 becomes the sunniest calendar month on record. Available from: https://www.metoffice.gov.uk/about‐us/press‐office/news/weather‐and‐climate/2020/2020‐spring‐and‐may‐stats. Accessed 26 August 2020.
- 11. Kumamoto DP, Maeda Y. A literature review of sports‐related orofacial trauma. Gen Dent. 2004;52:270–80. [PubMed] [Google Scholar]
- 12. Lam R. Epidemiology and outcomes of traumatic dental injuries: a review of the literature. Aust Dent J. 2016;61:4–20. [DOI] [PubMed] [Google Scholar]
- 13. Hurley S, Neligan M. Issue 3: preparedness letter for primary dental care. Available from: https://www.england.nhs.uk/coronavirus/wp‐content/uploads/sites/52/2020/03/issue‐3‐preparedness‐letter‐for‐primary‐dental‐care‐25‐march‐2020.pdf. [Accessed 15 April 2020].
- 14. England NHS. Redeploying the clinical dental workforce to support the NHS clinical delivery plan for COVID‐19. Available from: https://www.england.nhs.uk/coronavirus/wp‐content/uploads/sites/52/2020/04/C0301‐Permissions‐Redeploying‐our‐people‐clinical‐dental‐workforce‐v2.pdf. [Accessed 26 August 2020].
- 15. Lee JY, Divaris K. Hidden consequences of dental trauma: the social and psychological effects. Pediatr Dent. 2009;31:96–101. [PubMed] [Google Scholar]
- 16. Chen HH, Neumeier AT, Davies BW, Durairaj VD. Analysis of pediatric facial dog bites. Craniomaxillofac Trauma Reconstr. 2013;6:225–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Quinn J, Drzewiecki A, Li M, Stiell I, Sutcliffe T, Elmslie T, et al. A randomized, controlled trial comparing a tissue adhesive with suturing in the repair of pediatric facial lacerations. Ann Emerg Med. 1993;22:1130–5. [DOI] [PubMed] [Google Scholar]
- 18. Dua R, Abd el Rahman H, Fan K. Emergency paediatric admissions to a maxillofacial unit in London. Int J Oral Maxillofac Surg. 2017;46:258–9. [Google Scholar]
- 19. Islam S, Ansell M, Mellor T, Hoffman G. A prospective study into the demographics and treatment of paediatric facial lacerations. Pediatr Surg Int. 2006;22:797–802. [DOI] [PubMed] [Google Scholar]
- 20. Dua R, Abd el Rahman H, Fan K. Parental opinion of topical local anaesthetics used for paediatric facial lacerations. Int J Oral Maxillofac Surg. 2017;46:259. [Google Scholar]
- 21. NSPCC . Calls about domestic abuse highest on record following lockdown increase. Available from: https://www.nspcc.org.uk/about‐us/news‐opinion/2020/Calls‐about‐domestic‐abuse‐highest‐on‐record‐following‐lockdown‐increase/. [Accessed 19 June 2020].
- 22. Levin L, Zadik Y. Education on and prevention of dental trauma: it’s time to act!. Dent Traumatol. 2012;28:49–54. [DOI] [PubMed] [Google Scholar]
- 23. Hutchison CM, Cave V, Walshaw EG, Burns B, Park C. YouTube™ as a source for patient education about the management of dental avulsion injuries. Dent Traumatol. 2020;36:207–11. [DOI] [PubMed] [Google Scholar]
- 24. Chen J, Hobdell MH, Dunn K, Johnson KA, Zhang J. Teledentistry and its use in dental education. J Am Dent Assoc. 2003;134:342–6. [DOI] [PubMed] [Google Scholar]
- 25. Virdee J, Sharma R, Ponduri S. Spotlight on teledentistry. Br Dent J. 2020;228:815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Harding L, Campbell D. Up to 20% of hospital patients with Covid‐19 caught it at hospital. Available from: https://www.theguardian.com/world/2020/may/17/hospital‐patients‐england‐coronavirus‐covid‐19. [Accessed 26 August 2020].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


