Abstract
Background
Veterans have higher rates of anxiety, depression, and posttraumatic stress disorder (PTSD), and may be vulnerable to mental health consequences of the Covid‐19 pandemic. More than half of veterans who meet mental illness criteria do not seek help. This study screened for clinical symptoms and evaluated the efficacy of a brief, online social‐contact‐based video intervention in increasing treatment‐seeking intentions among veterans. We hypothesized that the video‐based intervention would increase treatment‐seeking intentions more than written vignette and control conditions.
Methods
One hundred seventy‐two veterans were randomized to either a (a) brief video‐based intervention; (b) written vignette intervention, or (c) nonintervention control group. In the 3‐min video, a veteran previously diagnosed with PTSD described his symptom reactivation by Covid‐19, his barriers to care, and how therapy helped him to cope. Assessments were conducted at baseline, postintervention, and at 14‐ and 30‐day follow‐ups.
Results
A total of 91 (53%) veterans reported high levels of clinical symptoms, especially those self‐reporting Covid‐19 exposure. The brief video‐based intervention yielded greater increase in treatment‐seeking intentions among veterans. Within the video group, women showed an increase in treatment‐seeking intentions from baseline to postintervention only, whereas men showed a more sustained effect, from baseline to Day 14.
Conclusions
Surveyed veterans reported high symptoms levels. A brief video intervention increased treatment‐seeking intention, likely through identification and emotional engagement with the video protagonist. This easily disseminable video‐based intervention has the potential to increase likelihood of seeking care. Future research should examine longer term sustainability and changes in help‐seeking behavior.
Keywords: anxiety, Covid‐19, depression, help‐seeking, intervention, PTSD, veterans
1. INTRODUCTION
The Covid‐19 pandemic has profoundly affected individuals worldwide, exposing them to greater risk of anxiety, depression, and posttraumatic stress disorder (PTSD) (Amsalem et al., 2020). People prone to psychological problems are especially vulnerable. Veterans often have high rates of preexisting trauma and report high prevalence of psychiatric disorders (Blodgett et al., 2015; Breslau et al., 2008; Trivedi et al., 2015; Wild et al., 2016). Pre‐Covid‐19 comparison of US veterans to the general population found that veterans had more anxiety (23% vs. 17%), depression (33% vs. 19%), and PTSD (26% vs. 13%) symptoms (Fortney et al., 2016). Yet, some veterans might be less impacted if they already have PTSD and feeling unsafe is not new to them (Rosen et al., 2005). A recent study showed that veterans may face risk of increased rates of mental problems during the pandemic (Murphy et al., 2020). Thus, addressing COVID‐19 mental health problems among veterans, and effectively enhancing their help‐seeking, is crucial. Encouraging veterans to pursue treatment might reduce long‐term costs, disability, and future psychiatric morbidity (Dell'Osso et al., 2013; Kraus et al., 2019).
Approximately 60% of veterans who meet mental illness criteria do not seek help (Hoge et al., 2004; Lazar, 2014). Across studies, one of the most frequently reported barriers to help‐seeking among veterans is concern about stigma, with many expecting to face prejudice and discrimination (Iversen et al., 2011; Kehle et al., 2010). For example, “My friends and family members might treat me differently” and “I would be seen as weak” are among the main stigma concerns veterans endorse (Sharp et al., 2015). In this pandemic‐related stress, some psychological first aid packages include components that target stigma reduction (Blake et al., 2020). As studies have found a negative association between treatment stigma and intentions to use mental health services (Blais & Renshaw, 2013; Clement et al., 2015; Sharp et al., 2015), interventions to reduce stigma and increase treatment‐seeking intentions among veterans could promote treatment participation.
Research has shown that social contact‐based interventions most effectively reduce mental‐health‐related stigma and attitudes and enhance help‐seeking intentions (Thornicroft et al., 2016). Social contact involves interpersonal contact with members of the stigmatized group. Members of the general population who meet and interact with individuals with lived experience (i.e., individuals who are struggling with mental illness themselves) are likely to lessen their stigma and discrimination. The core element of contact‐based antistigma programs is an empowered presenter from the stigmatized group who describes his or her personal story, preferably tailored to enhance audience identification (Amsalem et al., 2020; Corrigan et al., 2013; 2014), with emphasis on recovery‐oriented themes showing greater efficacy than symptom‐based content (Li et al., 2017). Video‐based social contact interventions have shown similar efficacy to in‐person presentations in improving attitudes toward individuals with lived experience (Janoušková et al., 2017; Koike et al., 2018). Moreover, while in‐person interventions are difficult to replicate and tend to target relatively small exposure groups, video‐based interventions necessitate minimal resource use, cost less, and facilitate dissemination to specific targeted audiences. Previous studies that examined the efficacy of social contact‐based video interventions among veterans used educational content with a series of hundreds of videos (Hamblen et al., 2019) or a 35‐min long video (Hurtado et al., 2019). No study has shown the efficacy of a single ultra‐brief video.
To address this gap, we designed a randomized controlled study to screen veteran psychopathology and test the efficacy of a brief video‐based intervention in increasing treatment‐seeking intentions, with assessments at baseline, postintervention, and at 14‐ and 30‐day follow‐ups. Participants with military experience (US veterans) were randomly assigned to one of three conditions: (1) a brief video‐based intervention (“video”); (2) a written vignette intervention, containing the same material as the video (“vignette”); or (3) a nonintervention control group (“control”). We hypothesized: (1) as with other disasters and epidemics, the Covid‐19 pandemic would produce relatively high levels of anxiety, depression, and PTSD, and (2) the brief video‐based intervention would increase treatment‐seeking intentions more than the vignette and control groups.
2. METHODS
2.1. Participants and recruitment
We recruited participants using Amazon Mechanical Turk (MTurk) (Paolacci et al., 2010), a leading crowdsourcing platform widely used in medical and psychology research (Cunningham et al., 2017). We used several methods to ensure the validity of participants and their responses: First, we scanned all participants to exclude people based on answering the survey more than once, completing the assessment in less than the minimum expected time, locations (coordinates) outside of the United States, or having suspicious IP addresses. Second, we used an open‐ended question format requiring the participant's age as a validity question and allowed only a two‐digit number as a valid answer. We then compared that answer to the age data MTurk provided to disqualify fake participants. Third, we added a question about military trauma with an option of “I did not serve in the military.” All of this resulted in the exclusion of one (0.6%) participant. We required participants to be English‐speaking US residents, 18–80 years old, with self‐reported military experience. Participants were compensated $6 for study participation. The New York State Psychiatric Institute Institutional Review Board approved the project. Before study entry, participants reviewed an informed consent form. Those who agreed to participate were directed to complete the study procedures via Qualtrics.com, a secure, online data‐collection platform.
2.2. Procedure
We conducted baseline demographic questionnaires and assessments before randomizing participants into one of three study groups (Figure 1). We also assessed whether participants had tested positive for Covid‐19 or had a close friend/family member currently or previously diagnosed with Covid‐19. The postintervention assessment was conducted immediately following the intervention. Follow‐up assessments were conducted 14 and 30 days after the postintervention assessment.
Figure 1.
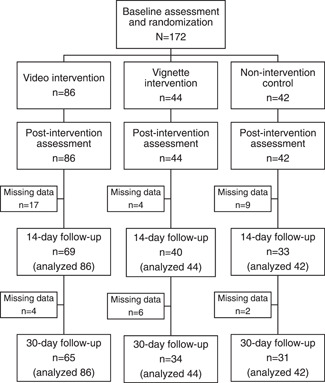
Study profile
2.3. Intervention
This study evaluated the short‐ and longer‐term efficacy of a video‐based intervention in increasing treatment‐seeking intentions. The video‐based intervention was a 3‐min video derived from a 35‐min interview of a 43‐year‐old National Guard veteran who had served in Iraq and had been diagnosed with PTSD. Well‐spoken with self‐deprecating humor, he described his barriers to care and reported avoiding seeking help for 10 years due to perceived stigma (“I thought that [getting treatment] was a sign of weakness, a sign that you can't do your job”). He described overcoming prior false, negative assumptions about treatment, discovering the benefits of social support and psychotherapy, and how they helped him to cope with Covid‐19 stressors that had reactivated his symptoms. He concluded with supportive encouragement: “If I can do this, you can do this!” The video was designed to humanize suffering via social contact. It depicted the veteran as a rounded human being and presented his symptoms in the context of his personal human narrative. The vignette was a written description of the content contained in the video but lacked the direct social contact aspect of the video.
2.4. Instruments
As the primary outcome measure, we used the three items measuring “openness to seeking help” from the Attitude Towards Seeking Professional Psychological Help Scale (ATSPPH‐SF) (Elhai et al., 2008), the most widely used assessment tool of help‐seeking attitudes (Picco et al., 2016). The chosen items specifically tested help‐seeking intentions: “I might want to have psychological counseling in the future,” “I would want to get psychological help if I were worried or upset for a long period of time,” and “A person with an emotional problem is not likely to solve it alone; he or she is more likely to solve it with professional help.” Response options were: 1 = “disagree,” 2 = “partially disagree,” 3 = “partially agree,” and 4 = “agree.” The total score ranged from 4 to 12, with higher scores indicating greater help‐seeking intentions. In this study, Cronbach's alpha coefficient of the ATSPPH items was .79. The ATSPPH‐SF was assessed at all four‐time points (i.e., baseline, postintervention, 14‐ and 30‐day follow‐ups).
Clinical assessments, conducted at baseline and at the 14‐ and 30‐day follow‐ups only, included the Generalized Anxiety Disorder‐7 (GAD‐7), Patient Health Questionnaire‐9 (PHQ‐9), and Primary Care PTSD Screen (PC‐PTSD). The seven GAD‐7 items assess generalized anxiety symptoms during the past 2 weeks (Spitzer et al., 2006). Response options were: 0 = “not at all,” 1 = “several days,” 2 = “more than half the days,” and 3 = “nearly every day.” Total score ranges from 0 to 21, with higher scores indicating greater self‐reported anxiety. Total score ≥5 indicates possible anxiety with high sensitivity (89%) and specificity (82%) (Spitzer et al., 2006). Cronbach's alpha for this study showed good internal consistency (α = .92). The PHQ‐9 is a screening instrument for major depression based on the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM‐5) criteria (Kroenke et al., 2001). The nine‐item instrument assesses depression symptoms during the past 2 weeks. Response options echo those of the GAD‐7. Total score ranges from 0 to 27, with higher scores indicating greater self‐reported depression. Total score ≥10 indicates possible major depression, with sensitivity of 88% and specificity of 85% (Levis et al., 2019). Cronbach's alpha in this sample was .90.
The PC‐PTSD‐5, a screening instrument with five yes/no‐item questions, is designed to identify respondents with probable PTSD. This self‐report reflects DSM‐5 PTSD diagnostic criteria, with three positive items being the screening threshold (Prins et al., 2016). The PC‐PTSD has good reliability and showed good operating characteristics when compared to PTSD diagnosis based on clinician interviews (Ouimette et al., 2008). In addition to assessing previous military trauma, this study focused the PC‐PTSD on Covid‐related events, to understand whether Covid‐19 reactivated pre‐existing PTSD symptoms. Hence, items were adjusted: “In the past month, have you felt guilty or unable to stop blaming yourself or others for the COVID‐19 related events?,” and “Have you felt numb or detached from people, activities, or your surroundings?” Cronbach's alpha was .72.
2.5. Analysis
Data were analyzed using SPSS 26.0. We used Pearson's χ 2 and one‐way analysis of variance to compare demographic variables, baseline psychopathological characteristics, and baseline ATSPPH‐SF scores of the three groups. We used Independent t tests to compare baseline psychopathological characteristics (continuous variables), and χ 2 tests to compare the severity of each psychopathology (ordinal variables) of participants who did and did not report Covid‐19 exposure. All statistical tests were two‐sided, using α < .05.
Intervention effects were tested using the generalized estimating equations (GEE) approach (Zeger & Liang, 1986; Zeger et al., 1988), as recommended for randomized controlled trials (Vens & Ziegler, 2012). The GEE approach accounts for correlated repeated‐measures analysis and accommodates missing data via estimated marginal means relying on the entire sample. Thus, this analytic strategy includes data from all randomized participants who provided at least one data point. To represent within‐subject dependencies in the models, we specified an unstructured correlation matrix. We first applied a full factorial model across the four time points (baseline and postintervention, 14 and 30‐day follow‐ups) for treatment‐seeking intentions, and three time points (baseline, 14‐ and 30‐day follow‐ups) for clinical symptoms. Time‐by‐group interaction terms were used to test the intervention effect hypothesis of greater treatment‐seeking in the video group. For significant differences, post hoc tests were used to compare each group pair. Effect sizes are reported using Cohen's d when appropriate.
3. RESULTS
3.1. Demographic characteristics
All 172 participants completed the baseline and postintervention assessments, 142 (83%) completed the 14‐day follow‐up, and 130 (76%) completed the 30‐day follow‐up (Figure 1). Baseline characteristics did not differ between completers and noncompleters, and rate of dropout did not differ between conditions (range: 23%–26%). This mostly (69%) male sample had a mean age of 47.2 (SD: 14.2; range: 23–78). Most participants identified as White (n = 132, 76%); 23 (14%) as African American, 4 (2%) as Asian, 2 (1%) as Native American, and 8 (5%) self‐identified as other. A total of 15 (9%) reported Hispanic ethnicity. Study groups did not significantly differ by age, gender, or race/ethnicity. Baseline GAD‐7, PHQ‐9, and PC‐PTSD scores did not differ across study groups (Table 1).
Table 1.
Demographics and Psychopathological Characteristics at Baseline, n (%)
| Video | Vignette | Control | ||||
|---|---|---|---|---|---|---|
| Items | n = 86 | n = 44 | n = 42 | Total n = 172 | statistic | p Value |
| Mean age (SD) | 48.2 ± 14.3 | 45.4 ± 13.3 | 47.3 ± 15.6 | 47.2 ± 14.3 | 0.57a | .57 |
| Gender—male (%) | 60 (70) | 30 (68) | 28 (67) | 118 (69) | 1.17b | .88 |
| Hispanic | 7 (8) | 5 (11) | 3 (7) | 15 (9) | 2.38b | .67 |
| Race | ||||||
| White | 64 (74) | 39 (89) | 28 (67) | 132 (76) | 10.1b | .43 |
| African American | 12 (14) | 2 (5) | 9 (21) | 23 (14) | ||
| Asian | 2 (2) | 0 (0) | 2 (5) | 4 (2) | ||
| Native American | 2 (2) | 0 (0) | 0 (0) | 2 (1) | ||
| Other | 4 (5) | 2 (5) | 2 (5) | 8 (5) | ||
| Exposure to Covid‐19 | 26 (31) | 17 (39) | 17 (40) | 60 (35) | 1.97b | .37 |
| Exposure to military trauma | 23 (27) | 16 (36) | 10 (24) | 49 (28) | 1.92b | .38 |
| Clinical symptoms at baseline | ||||||
| GAD‐7 | 4.7±5.0 | 4.2±5.0 | 5.0±5.1 | 4.7±5.0 | 0.25a | .78 |
| PHQ‐9 | 5.2±5.6 | 5.7±5.8 | 5.7±6.0 | 5.4±5.7 | 0.16a | .85 |
| PC‐PTSD | 1.2±1.4 | 1.2±1.5 | 1.1±1.4 | 1.2±1.4 | 0.16a | .85 |
Abbreviations: ANOVA, analysis of variance; DSM‐5, Diagnostic and Statistical Manual of Mental Disorders, 5th Edition; GAD‐7, generalized anxiety disorder; PC‐PTSD, Primary Care PTSD Screen for DSM‐5; PHQ‐9, Patient Health Questionnaire.
One way ANOVA.
Pearson χ 2.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
3.2. Clinical characteristics and exposure to Covid‐19
A total of 67 (39%) participants screened positive for probable generalized anxiety disorder (GAD‐7 ≥5), with 22 (13%) reporting moderate anxiety (GAD‐7 ≥10) and 10 (6%) reporting severe anxiety (GAD‐7 ≥15). A total of 78 (45%) participants screened positive for probable depression (PHQ‐9 ≥5), including 16 (9%) reporting moderate (PHQ‐9 ≥10), 11 (6%) reporting moderately severe (PHQ‐9 ≥15), and 5 (3%) reporting severe depression (PHQ‐9 ≥20). A total of 31 (18%) participants reported symptoms suggesting probable PTSD (PC‐PTSD ≥3; Table 2). Overall, 118 (69%) participants screened positive for either anxiety, depression and/or PTSD across times points.
Table 2.
Exposure to Covid‐19 and Clinical Symptoms at Baseline
| Total | Exposure to Covid‐19a | |||||
|---|---|---|---|---|---|---|
| (n = 172) | Yes (n = 60) | No (n = 112) | statistic | p Value | ||
| Age | 47.2 ± 14.2 | 43.3 ± 12.9 | 49.3 ± 14.6 | 2.7b | .009 | |
| Clinical symptoms | ||||||
| GAD‐7 (range: 0–21) | 4.7 ± 5.0 | 6.2 ± 5.4 | 3.8 ± 4.7 | 3.1b | .003 | |
| PHQ‐9 (range: 0–27) | 5.4 ± 5.7 | 6.9 ± 5.9 | 4.7 ± 5.5 | 2.4b | .020 | |
| PC‐PTSD (range: 0–5) | 1.2 ± 1.4 | 1.7 ± 1.6 | 0.9 ± 1.3 | 3.5b | .001 | |
| Severity level of GAD | ||||||
| Mild (9≥GAD‐7≥5) | 35 (20%) | 12 (20%) | 23 (21%) | 13.8c | .003 | |
| Moderate (14≥GAD‐7≥10) | 22 (13%) | 15 (25%) | 7 (6%) | |||
| Severe (GAD‐7 ≥15) | 10 (6%) | 4 (7%) | 6 (5%) | |||
| Total | 67 (39%) | 31 (53%) | 36 (32%) | |||
| Severity level of depression | ||||||
| Mild (9≥PHQ‐9≥5) | 46 (27%) | 13 (22%) | 33 (29%) | 18.7c | .001 | |
| Moderate (14≥PHQ‐9≥10) | 16 (9%) | 12 (20%) | 4 (4%) | |||
| Moderately severe (19≥PHQ‐9≥15) | 11 (6%) | 7 (12%) | 4 (4%) | |||
| Severe (PHQ‐9 ≥20) | 5 (3%) | 1 (2%) | 4 (4%) | |||
| Total | 78 (45%) | 33 (55%) | 45 (40%) | |||
| PTSD | 31 (18%) | 19 (32%) | 12 (11%) | 12.0c | .001 | |
| Any psychopathology | 118 (69%) | 46 (27%) | 41 (24%) | 3.8c | .051 | |
Note: The bold values are the significance p values for "statistics" column.
Abbreviations: DSM‐5, Diagnostic and Statistical Manual of Mental Disorders, 5th Edition; GAD‐7, generalized anxiety disorder; PC‐PTSD, Primary Care PTSD Screen for DSM‐5; PHQ‐9, Patient Health Questionnaire.
Exposure to Covid‐19 were participants who tested positive to Covid‐19, or had a close friend/family member who tested positive.
Independent t test.
Pearson χ 2.
This article is being made freely available through PubMed Central as part of the COVID-19 public health emergency response. It can be used for unrestricted research re-use and analysis in any form or by any means with acknowledgement of the original source, for the duration of the public health emergency.
A total of 60 (35%) participants reported Covid‐19 exposure (testing positive or having a close friend/family member diagnosed with Covid‐19) at baseline, with distribution not differing across study groups (χ 2 = 1.97; p = .37). Covid‐19‐“exposed” participants had lower mean age (43.3 ± 12.9 vs. 49.3 ± 14.6; p = .009) and reported increased social media use: 20 (34%) participants reported spending more than 4 h a day, compared to 15 (13%) participants in the nonexposed group (χ 2 = 13.4; p = .004). Covid‐19‐“exposed” participants reported higher baseline clinical symptoms: 53% (vs. 32% nonexposed) screened positive for GAD (GAD‐7 ≥5) (χ 2 = 13.8; p = .003), 55% (vs. 40% nonexposed) for depression (PHQ‐9 ≥5) (χ 2 = 18.7; p = .001), and 32% (vs. 11% nonexposed) for PTSD (PC‐PTSD ≥3) (χ 2 = 12.0; p = .001; Table 2).
3.3. Intervention effects
As hypothesized, study groups significantly differed on the primary outcome. The brief video intervention yielded greater increase in treatment‐seeking intentions. Figure 2 presents results of the GEE model for ATSPPH scores. Baseline scores did not differ across study groups (Video mean scores 7.4, confidence interval [CI] [6.9–8.0], vignette 7.9, CI [7.3–8.6], and control 7.3, CI [6.6–8.1]). A main effect of time (Wald χ 2 = 34.5; p < .001) was subsumed under a significant time‐by‐group interaction effect (Wald χ 2 = 13.9; p = .031). Follow‐up analyses of baseline and post‐intervention time points indicated a significant main effect of time (Wald χ 2 = 21.9; p < .001) and a group‐by‐time interaction (Wald χ 2 = 12.3; p = .002), with increased treatment‐seeking intentions in the video group only (CI [0.51–1.13], p < .001, Cohen's d = 0.32; video from 7.4 (CI [6.9–8.0]) to 8.2 (CI [7.7–8.8]); vignette from 8.0 (CI [7.3–8.6]) to 8.1 (CI [7.4–8.7]); control from 7.3 (CI [6.6–8.1]) to 7.6 (CI [6.9–8.3]). Further analysis comparing the postintervention and 14‐day follow‐up means scores yielded only a main effect of time (Wald χ 2 = 8.8; p < .001), with the 14‐ and 30‐day follow‐ups yielding no significant effects.
Figure 2.
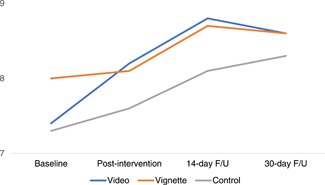
Comparison between Video (n = 86), Vignette (n = 44) and Control (n = 42) Groups on Attitudes Toward Seeking Professional Help Scale (ATTPHS) Over Time. Scores ranged from 3 to 12, with higher scores indicate higher help seeking intentions; F/U. follow‐up
Figure 3 presents the results of a secondary, within‐groups item‐level analysis, among the 118 (69%) participants who reported psychopathology (anxiety, depression and/or PTSD). A main effect of time (Wald χ 2 = 17.2; p = .001) was subsumed under a near significant time‐by‐group interaction effect (Wald χ 2 = 11.7; p = .069). The video group's ATSPPH mean scores increased from 7.6 (CI [6.9–8.3]) at baseline to 8.4 (CI [7.9–9.1]) at postintervention (p < .001, Cohen's d = 0.34), 8.9 (CI [8.3–9.6]) at 14‐day follow‐up (p = .01; Cohen's d = 0.56), and 8.6 (CI [7.9–9.3]) at 30‐day follow‐up (p=.13, Cohen's d = 0.37). The vignette group scores were 8.1 (CI [7.4–8.8]) at baseline, 8.1 (CI [7.3–8.9]) at post‐intervention, 8.5 (CI [8.1–9.0]) at 14‐day follow‐up, and 8.3 (CI [7.9–8.8]) at 30‐day follow‐up. The control group scores were 7.7 (CI [6.9–8.5]) at baseline, 8.0 (CI [7.3–8.8]) at postintervention, 8.2 (CI [7.5–8.9]) at 14‐day follow‐up, and 8.2 (CI [7.7–8.8]) at 30‐day follow‐up.
Figure 3.
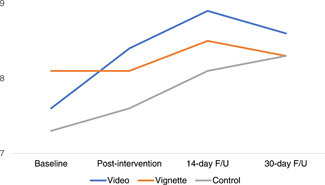
Comparison between Video (n = 54), Vignette (n = 30) and Control (n = 34) Groups on Attitudes Toward Seeking Professional Help Scale (ATTPHS) Over Time among veterans who reported anxiety, depression or PTSD. Scores ranged from 3 to 12, with higher scores indicate higher help seeking intentions; F/U, follow‐up
To better understand the observed intervention effects, and based on our previous study (Amsalem et al., 2020), we conducted a secondary, within‐groups item‐level analysis. As the protagonist in the video was male, we examined whether the video had greater influence on men. For the video‐based group, both men and women reported increased help‐seeking intentions between baseline and postintervention (men: from 7.3 to 7.8, paired t test = 4.0, p < .001; Cohen's d = 0.22, CI [0.3–0.8]; women: from 8.2 to 8.5, paired t test = 3.4, p = .002, Cohen's d = 0.17, CI [0.1–0.7]), but only men showed an additional increase in mean scores between postintervention and the 14‐day follow‐up assessment (for men: from 7.8 to 8.6, t = 2.5, p = .016, Cohen's d = 0.42, CI [0.3–1.2] vs. for women: from 8.5 to 8.6, t = 0.2, p = .88, CI [−0.7–0.8]). No differences emerged at 30‐day follow‐up. No gender differences were found within the vignette and control groups at any time point.
4. DISCUSSION
Our randomized controlled trial assessed self‐reported probable anxiety, depression, and PTSD among veterans during Covid‐19, and tested the utility of a brief intervention in increasing their treatment‐seeking intentions. Self‐reported psychiatric symptoms were high in this veteran, Covid‐era sample. As hypothesized, the brief video‐based intervention yielded greater increase in treatment‐seeking intentions among veterans. In the 3‐min video, a veteran previously diagnosed with PTSD and depression portrayed his personal story, described how Covid‐19 reactivated his symptoms, and how therapy helped him to cope with daily difficulties. Consistent with previous studies (Hurtado et al., 2019; Thornicroft et al., 2016), this RCT showed the greater effectiveness of social contact‐based video interventions. This study is the first to demonstrate effectiveness of a brief social contact‐based video in increasing treatment‐seeking intentions among veterans.
Overall, the video‐based intervention yielded a greater increase in treatment‐seeking intentions compared to written vignette and control groups, mostly short‐term. Furthermore, a secondary analysis among a subgroup of veterans who reported clinical symptoms of anxiety, depression, or PTSD showed a similar pattern of increase in treatment‐seeking intention in the video group only. Other studies (Hamblen et al., 2019; Hurtado et al., 2019) that tested social contact‐based interventions used much longer videos or a significantly greater number of videos. Brevity has advantages: lower cost, use of fewer resources, and offering focused, proactive approach to encourage veterans to seek help if needed. This single, targeted, Covid‐related antimental health stigma video can be sent by email or shared on social media platforms. How can a 3‐min video create such change? The video protagonist, a 43‐year‐old White male, shared several characteristics with most viewers: age (mean = 47), gender (70% male), race (74% identified as White), and, of course, the living experience of a veteran trying to cope with the Covid‐19. In addition to veterans, this brief intervention may benefit other subgroups affected by this pandemic (e.g., healthcare workers), potentially changing their openness to treatment‐seeking as well (Serrano‐Ripoll et al., 2020). However, we found no differences across conditions at Day 30. Future studies should explore whether booster videos enhance the intensity and durability of this effect among veterans and other populations (Corrigan et al., 2015).
A secondary, within groups item‐level analysis showed that although the video had an immediate effect on both men and women, only men showed persisting, longer‐term effects. This gender difference, found only in the video group, strengthens our hypothesis that a tailored intervention enabled identification and enhanced the emotional engagement between video protagonist and viewer. This finding corroborates our previous study: a similar intervention with a 22‐year‐old woman protagonist sharing her living experience with psychosis showed greater efficacy among women viewers in the video group only (Amsalem et al., 2020). Further studies should examine whether characteristics as age, gender, race/ethnicity could create greater change in perception regarding treatments and seeking help.
Almost half of the participants reported probable anxiety and depression, one‐fifth reported PTSD symptoms, and of the 172 participants, 118 (69%) reported probable psychopathology across time points. No other study has screened for clinical symptoms among veterans during the Covid‐19 pandemic, although compared to data of veterans pre‐Covid‐19, or to nonveteran groups during the pandemic, it appears relatively high. For example, using equivalent instruments, a previous study of veterans. Conducted before the Covid‐19 era, showed lower rates for probable anxiety (23%) and depression (33%), and a similar level of PTSD (Fortney et al., 2016). Recent studies among healthcare workers, people diagnosed with Covid‐19, and their relatives show similarly increased rates of symptomatology (Pappa et al., 2020; Pfefferbaum & North, 2020). The Covid‐19 pandemic has profoundly affected individuals and populations, and these findings emphasize the need to intervene for at‐risk groups like veterans (Pfefferbaum & North, 2020).
4.1. Limitations
Our study has several limitations. First, study findings are limited to MTurk participants, who might differ from the veteran population (Paolacci et al., 2010). For example, 76% of participants reported white race, 14% reported African American race, and 9% reported Hispanic ethnicity, percentages slightly divergent from the distribution of the US veteran population of 81% White, 12% African American, and 8% Hispanic (https://www.va.gov/vetdata/veteran_population.as). Second, our survey of veteran symptoms derived from a relatively small sample, used only self‐report instruments, and hence requires cautious interpretation. Third, we only assessed openness to seeking help (treatment‐seeking intentions), the reporting of which is subject to social desirability (Perinelli & Gremigni, 2016) and thus may not reflect actual help‐seeking behaviors. Future studies should measure change in help‐seeking behaviors and inquire if respondents were actually receiving mental health services. Last, our study showed limited longer‐term effects of our brief video intervention. Further studies are needed to examine how to create a sustainable effect.
5. CONCLUSION
The Covid‐19 pandemic has accelerated an already emerging trend towards online platforms, which is changing dissemination of knowledge and consumption of contents. More than half of the surveyed veterans reported symptoms of either generalized anxiety, depression, and/or PTSD, emphasizing the need for an online intervention to increase treatment‐seeking. A 3‐min online social contact‐based video intervention effectively increased self‐reported short‐term help‐seeking intentions among participants. Men showed a greater duration of this effect solely in the video group, supporting our hypothesis that identification with the video protagonist increases treatment‐seeking intentions. This is the first study to assess Covid‐19 related psychopathology in a veteran sample, and to use such a brief intervention. This ultra‐brief video‐based intervention can be easily shared and disseminated by email or social media platform, and has the potential to increase likelihood of seeking care, which is crucial during this Covid‐19 pandemic era. Future studies should examine the effect of a series of videos (booster videos) on treatment‐seeking intentions and behaviors.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
ACKNOWLEDGMENT
The authors thank the video participant, who shared his story and contributed to help‐seeking.
Amsalem, D. , Lazarov, A. , Markowitz, J. C. , Gorman, D. , Dixon, L. B. , & Neria, Y. (2021). Increasing treatment‐seeking intentions of US veterans in the Covid‐19 era: A randomized controlled trial. Depression Anxiety. 38, 639–647. 10.1002/da.23149
Clinicaltrials.gov identifier: NCT04484207.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- Amsalem, D. , Dixon, L. B. , & Neria, Y. (2020). The coronavirus disease 2019 (COVID‐19) outbreak and mental health. JAMA Psychiatry, 78(1), 9–10. 10.1001/jamapsychiatry.2020.1730 [DOI] [PubMed] [Google Scholar]
- Amsalem, D. , Yang, L. H. , Jankowski, S. , Lieff, S. A. , Markowitz, J. C. , & Dixon, L. B. (2020). Reducing stigma toward individuals with schizophrenia using a brief video: A randomized controlled trial of young adults. Schizophrenia Bulletin, 46(5), 7–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blais, R. K. , & Renshaw, K. D. (2013). Stigma and demographic correlates of help‐seeking intentions in returning service members. Journal of Traumatic Stress, 26(1), 77–85. [DOI] [PubMed] [Google Scholar]
- Blake, H. , Bermingham, F. , Johnson, G. , & Tabner, A. (2020). Mitigating the psychological impact of covid‐19 on healthcare workers: A digital learning package. International Journal of Environmental Research and Public Health, 17(9), 2997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blodgett, J. C. , Avoundjian, T. , Finlay, A. K. , Rosenthal, J. , Asch, S. M. , Maisel, N. C. , & Midboe, A. M. (2015). Prevalence of mental health disorders among justice‐involved veterans. Epidemiologic Reviews, 37, 163–176. [DOI] [PubMed] [Google Scholar]
- Breslau, N. , Peterson, E. L. , & Schultz, L. R. (2008). A second look at prior trauma and the posttraumatic stress disorder effects of subsequent trauma. Archives of General Psychiatry, 65(4), 431–437. [DOI] [PubMed] [Google Scholar]
- Clement, S. , Schauman, O. , Graham, T. , Maggioni, F. , Evans‐Lacko, S. , Bezborodovs, N. , Morgan, C. , Rüsch, N. , Brown, J. S. L. , & Thornicroft, G. (2015). What is the impact of mental health‐related stigma on help‐seeking? A systematic review of quantitative and qualitative studies. Psychological Medicine, 45(1), 11–27. [DOI] [PubMed] [Google Scholar]
- Corrigan, P. , Michaels, P. J. , & Morris, S. (2015). Do the effects of antistigma programs persist over time? Findings from a meta‐analysis. Psychiatric Services, 66(5), 543–546. [DOI] [PubMed] [Google Scholar]
- Corrigan, P. W. , Michaels, P. J. , Vega, E. , Gause, M. , Larson, J. , Krzyzanowski, R. , & Botcheva, L. (2014). Key ingredients to contact‐based stigma change: A cross‐validation. Psychiatric Rehabilitation Journal, 37(1), 62–64. [DOI] [PubMed] [Google Scholar]
- Corrigan, P. W. , Vega, E. , Larson, J. , Michaels, P. J. , McClintock, G. , Krzyzanowski, R. , Gause, M. , & Buchholz, B. (2013). The California schedule of key ingredients for contact‐based antistigma programs. Psychiatric Rehabilitation Journal, 36(3), 173–179. [DOI] [PubMed] [Google Scholar]
- Cunningham, J. A. , Godinho, A. , & Kushnir, V. (2017). Can Amazon's Mechanical Turk be used to recruit participants for internet intervention trials? A pilot study involving a randomized controlled trial of a brief online intervention for hazardous alcohol use. Internet Interv, 1(10), 12–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dell'Osso, B. , Glick, I. , Baldwin, D. , & Altamura, A. (2013). Can long‐term outcomes be improved by shortening the duration of untreated illness in psychiatric Disorders? A conceptual framework. Psychopathology, 46(1), 14–21. [DOI] [PubMed] [Google Scholar]
- Elhai, J. D. , Schweinle, W. , & Anderson, S. M. (2008). Reliability and validity of the Attitudes Toward Seeking Professional Psychological Help Scale‐Short Form. Psychiatry Research, 159(3), 320–329. [DOI] [PubMed] [Google Scholar]
- Fortney, J. C. , Curran, G. M. , Hunt, J. B. , Cheney, A. M. , Lu, L. , Valenstein, M. , & Eisenberg, D. (2016). Prevalence of probable mental disorders and help‐seeking behaviors among veteran and non‐veteran community college students. General Hospital Psychiatry, 38, 99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamblen, J. L. , Grubaugh, A. L. , Davidson, T. M. , Borkman, A. L. , Bunnell, B. E. , & Ruggiero, K. J. (2019). An online peer educational campaign to reduce stigma and improve help seeking in veterans with posttraumatic stress disorder. Telemed e‐Health, 25(1), 41–47. [DOI] [PubMed] [Google Scholar]
- Hoge, C. W. , Castro, C. A. , Messer, S. C. , McGurk, D. , Cotting, D. I. , & Koffman, R. L. (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine, 351(1), 13–22. [DOI] [PubMed] [Google Scholar]
- Hurtado, S. L. , Simon‐Arndt, C. M. , Schmied, E. A. , Belding, J. N. , Subala, R. S. , & Richardson, C. M. (2019). Use of an educational video to reduce barriers to military mental health care. Psychiatric Services, 70(10), 915–920. [DOI] [PubMed] [Google Scholar]
- Iversen, A. C. , Van Staden, L. , Hughes, J. H. , Greenberg, N. , Hotopf, M. , Rona, R. J. , Thornicroft, G. , Wessely, S. , & Fear, N. T. (2011). The stigma of mental health problems and other barriers to care in the UK Armed Forces. BMC Health Services Research, 11, 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janoušková, M. , Tušková, E. , Weissová, A. , Trančík, P. , Pasz, J. , Evans‐Lacko, S. , & Winkler, P. (2017). Can video interventions be used to effectively destigmatize mental illness among young people? A systematic review. European Psychiatry, 41, 1–9. [DOI] [PubMed] [Google Scholar]
- Kehle, S. M. , Polusny, M. A. , Murdoch, M. , Erbes, C. R. , Arbisi, P. A. , Thuras, P. , & Meis, L. A. (2010). Early mental health treatment‐seeking among U.S. National Guard soldiers deployed to Iraq. Journal of Traumatic Stress, 23(1), 33–40. [DOI] [PubMed] [Google Scholar]
- Koike, S. , Yamaguchi, S. , Ojio, Y. , Ohta, K. , Shimada, T. , Watanabe, K. , Thornicroft, G. , & Ando, S. (2018). A randomised controlled trial of repeated filmed social contact on reducing mental illness‐related stigma in young adults. Epidemiology and Psychiatric Sciences, 27(2), 199–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraus, C. , Kadriu, B. , Lanzenberger, R. , Zarate, C. A. , & Kasper, S. (2019). Prognosis and improved outcomes in major depression: A review. Translational Psychiatry, 9(1), 127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K. , Spitzer, R. L. , & Williams, J. B. W. (2001). The PHQ‐9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazar, S. G. (2014). The mental health needs of military service members and veterans. Psychodyn Psychiatry, 42(3), 459–478. [DOI] [PubMed] [Google Scholar]
- Levis, B. , Benedetti, A. , & Thombs, B. D. (2019). Accuracy of Patient Health Questionnaire‐9 (PHQ‐9) for screening to detect major depression: Individual participant data meta‐analysis. BMJ, 365, 1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Y. , Sorrentino, R. , Norman, R. , Hampson, E. , & Ye, Y. (2017). Effects of symptom versus recovery video, similarity, and uncertainty orientation on the stigmatization of schizophrenia. Personality and Individual Differences, 106, 117–121. [Google Scholar]
- Murphy, D. , Williamson, C. , Baumann, J. , Busuttil, W. , & Fear, N. T. (2020). Exploring the impact of COVID‐19 and restrictions to daily living as a result of social distancing within veterans with pre‐existing mental health difficulties. BMJ Mil Heal, bmjmilitary‐2020‐001622. online ahead of print. [DOI] [PubMed] [Google Scholar]
- Ouimette, P. , Wade, M. , Prins, A. , & Schohn, M. (2008). Identifying PTSD in primary care: Comparison of the primary care‐PTSD screen (PC‐PTSD) and the General Health Questionnaire‐12 (GHQ). Journal of Anxiety Disorders, 22(2), 337–343. [DOI] [PubMed] [Google Scholar]
- Paolacci, G. , Chandler, J. , & Ipeirotis, P. G. (2010). Running experiments on Amazon mechanical turk. Judgm Decis Mak, 5, 411–419. [Google Scholar]
- Pappa, S. , Ntella, V. , Giannakas, T. , Giannakoulis, V. G. , Papoutsi, E. , & Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID‐19 pandemic: A systematic review and meta‐analysis. Brain, Behavior, and Immunity, 88, 901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perinelli, E. , & Gremigni, P. (2016). Use of social desirability scales in clinical psychology: A systematic review. Journal of Clinical Psychology, 72(6), 534–551. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum, B. , & North, C. S. (2020). Mental health and the Covid‐19 pandemic. New England Journal of Medicine, 383, 510–512. [DOI] [PubMed] [Google Scholar]
- Picco, L. , Abdin, E. , Chong, S. A. , Pang, S. , Shafie, S. , Chua, B. Y. , Vaingankar, J. A. , Ong, L. P. , Tay, J. , & Subramaniam, M. (2016). Attitudes toward seeking professional psychological help: Factor structure and socio‐demographic predictors. Frontiers in Psychology, 7, 547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins, A. , Bovin, M. J. , Smolenski, D. J. , Marx, B. P. , Kimerling, R. , Jenkins‐Guarnieri, M. A. , Kaloupek, D. G. , Schnurr, P. P. , Kaiser, A. P. , Leyva, Y. E. , & Tiet, Q. Q. (2016). The primary care PTSD screen for DSM‐5 (PC‐PTSD‐5): Development and evaluation within a veteran primary care sample. Journal of General Internal Medicine, 31(10), 1206–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen, C. , Tiet, Q. , Cavella, S. , Finney, J. , & Lee, T. (2005). Chronic PTSD patients' functioning before and after the September 11 attacks. Journal of Traumatic Stress, 18(6), 781–784. [DOI] [PubMed] [Google Scholar]
- Serrano‐Ripoll, M. J. , Meneses‐Echavez, J. F. , Ricci‐Cabello, I. , Fraile‐Navarro, D. , Fiol‐deRoque, M. A. , Pastor‐Moreno, G. , Castro, A. , Ruiz‐Pérez, I. , Zamanillo Campos, R. , & Gonçalves‐Bradley, D. C. (2020). Impact of viral epidemic outbreaks on mental health of healthcare workers: A rapid systematic review and meta‐analysis. Journal of Affective Disorders, 277, 347–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp, M. L. , Fear, N. T. , Rona, R. J. , Wessely, S. , Greenberg, N. , Jones, N. , & Goodwin, L. (2015). Stigma as a barrier to seeking health care among military personnel with mental health problems. Epidemiologic Reviews, 37, 144–162. [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L. , Kroenke, K. , Williams, J. B. W. , & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD‐7. Archives of Internal Medicine, 166(10), 1092–1097. [DOI] [PubMed] [Google Scholar]
- Thornicroft, G. , Mehta, N. , Clement, S. , Evans‐Lacko, S. , Doherty, M. , Rose, D. , Koschorke, M. , Shidhaye, R. , O'Reilly, C. , & Henderson, C. (2016). Evidence for effective interventions to reduce mental‐health‐related stigma and discrimination. Lancet, 387(10023), 1123–1132. [DOI] [PubMed] [Google Scholar]
- Trivedi, R. B. , Post, E. P. , Sun, H. , Pomerantz, A. , Saxon, A. J. , Piette, J. D. , Maynard, C. , Arnow, B. , Curtis, I. , Fihn, S. D. , & Nelson, K. (2015). Prevalence, comorbidity, and prognosis of mental health among US veterans. American Journal of Public Health, 105(12), 2564–2569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vens, M. , & Ziegler, A. (2012). Generalized estimating equations and regression diagnostics for longitudinal controlled clinical trials: A case study. Computational statistics & data analysis, 56, 1231–1242. [Google Scholar]
- Wild, J. , Smith, K. V. , Thompson, E. , Béar, F. , Lommen, M. J. J. , & Ehlers, A. (2016). A prospective study of pre‐trauma risk factors for post‐traumatic stress disorder and depression. Psychological Medicine, 46(12), 2571–2582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeger, S. L. , & Liang, K.‐Y. (1986). Longitudinal Data Analysis for Discrete and Continuous Outcomes. Biometrics, 42, 121–130. [PubMed] [Google Scholar]
- Zeger, S. L. , Liang, K.‐Y. , & Albert, P. S. (1988). Models for Longitudinal Data: A Generalized Estimating Equation Approach. Biometrics, 44, 1049–1060. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


