FIGURE 2.
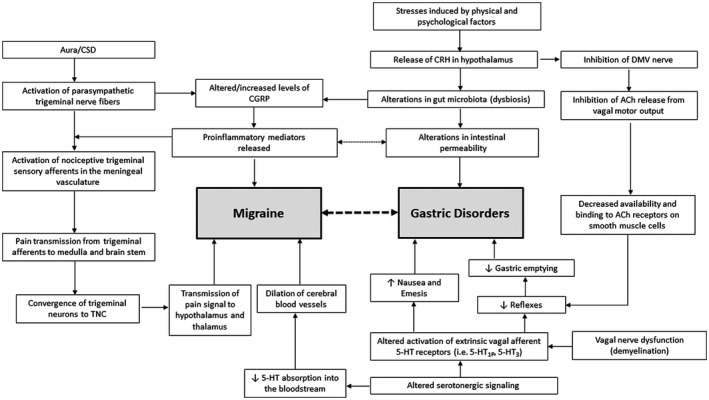
Proposed mechanisms explaining the relationship between migraine and gastric disorders. 21 , 131 A bidirectional relationship exists between migraine and gastric disorders, which is influenced by autonomic dysfunction; specifically, altered sympathetic and parasympathetic activity and changes in the gut microbiota profile, which are mediated by various cytokines, hormones, and neurotransmitters. 21 In migraine, cortical spreading depression (CSD) activates pain pathways that originate from the parasympathetic trigeminal nerve fibers and results in the release of calcitonin gene‐related peptide (CGRP) and proinflammatory mediators, which are implicated in both migraine and gastrointestinal (GI) disorder pathophysiology. 22 , 124 In gastric disorders, it is suggested that stress induced by physical and psychological factors causes the release of corticotrophin‐releasing hormone (CRH), which leads to alterations in gut microbiota and intestinal permeability, the release of proinflammatory mediators, and the inhibition of acetylcholine release, resulting in GI dysfunction. Another major factor contributing to this relationship is an alteration in serotonergic signaling, which can activate the TGV system involved in the initiation of a migraine attack and lead to the development of symptoms of gastric disorders including nausea, emesis, and delayed gastric emptying by altering GI reflex pathways or activating GI serotonin receptors. 21 , 62 Abbreviations: 5‐HT, 5‐hydroxytryptamine; ACh, acetylcholine; DMV, dorsal motor nucleus of the vagus; TGV, trigeminovascular; TNC, trigeminal nucleus caudalis
