Abstract
Background and Aims:
Arthroscopic orthopaedic surgery may lead to significant postoperative pain. Interscalene block (ISB) is associated with undesirable effects like phrenic nerve palsy. Shoulder block (ShB) is a relatively recent diaphragm sparing alternative for analgesia in these cases.
Methods:
This prospective randomised trial was conducted in 70 adult patients posted for arthroscopic Bankart repair surgery. Patients were randomly assigned into two groups: interscalene block [Group ISB (n = 35): 0.5% bupivacaine 10 ml] or shoulder block [Group ShB (n = 35): 0.5% bupivacaine (suprascapular block 10 ml and axillary block 10 ml)] using ultrasound and nerve stimulator. The primary aim of our study was to compare the ISB with ShB for visual analogue score (VAS) in recovery area (zero hour). Time for block performance, VAS, time to first rescue analgesia, total analgesic requirement, patient satisfaction and complications were recorded.
Results:
VAS was significantly higher in ShB group at 2 and 4 h (P = 0.001 and 0.000) while it was significantly higher in ISB group at 12 h (P = 0.013). The time to first analgesic request was significantly prolonged in ISB group as compared to ShB group (8.22 h vs. 4.69 h; P = 0.002) but total analgesic requirement and patient satisfaction at 24 h were similar. Complications like dyspnoea, ptosis and motor weakness were seen only with ISB group.
Conclusion:
Both ShB and ISB blocks have similar efficacy in terms of postoperative pain scores, cumulative analgesic requirements and patient satisfaction. However, considering the various undesirable effects associated with ISB, like phrenic nerve blockade, prolonged upper limb weakness and the occurrence of rebound pain, shoulder block may be preferred for arthroscopic shoulder surgeries.
Keywords: Arthroscopy, brachial plexus block, pain, phrenic nerve, postoperative, shoulder
INTRODUCTION
Arthroscopic shoulder surgery, albeit minimally invasive, is associated with considerable intraoperative and postoperative pain.[1] Regional anaesthesia reduces anaesthetic requirements and postoperative pain, thereby expediting recovery.[2] Interscalene brachial plexus block (ISB) is considered the gold standard technique for pain management in shoulder surgery as it provides the most reliable analgesia.[3] But ISB is associated with many undesirable effects like phrenic nerve palsy with diaphragmatic impairment which can potentially lead to respiratory compromise.[3,4,5]
A recent (2020) meta-analysis investigated the analgesic outcomes of suprascapular nerve (SSN) block after shoulder arthroscopy and found it to be inferior to ISB. The authors concluded that the landmark-guided posterior SSN block does not provide clinically meaningful analgesic benefits following shoulder surgery and that exploration of other alternatives to ISB is warranted.[6] The axillary nerve (AN) is another major contributor which complements the SSN for shoulder joint innervations.[7] An alternative approach of shoulder block (ShB) consisting of combined blockade of the SSN and AN was suggested by Price et al.[8] in the year 2007 to control postoperative shoulder pain.
Ultrasound-guided (USG) approach to SSN block (Harmon and Hearty; 2007)[9] and AN block (Roth et al.; 2011)[10] have been described as an option for analgesia for shoulder surgeries. The two blocks were later combined as USG ShB by Dhir et al.[11] in 2016 with excellent success rates. The high success rate afforded by USG procedure may increase the popularity of ShB over ISB due to its advantage of being a more distal phrenic sparing block.
We conducted this randomised trial with the primary objective of comparing the postoperative pain scores provided by both the techniques in the recovery room. The secondary objectives included time to first analgesic request, total analgesic requirement, pain scores, patient satisfaction, and complications.
METHODS
After the institutional ethics committee approval and registration in the clinical trial registry, this prospective randomised interventional trial was conducted in 70 American Society of Anesthesiologists (ASA) grades 1 and 2, adult (18–60 years) patients of either sex, undergoing elective unilateral arthroscopic shoulder surgery (Bankart repair) under general anaesthesia. Any patient with a history of local anaesthetic (LA) allergy, coagulopathy, anticoagulant therapy, local-site infection, body mass index (BMI) >30 kg/m2, inability to understand visual analogue scale (VAS), cardiopulmonary disorder and previous neurological deficit in the upper limbs were excluded from the study.
After written informed consent, patients were randomly allocated into 2 groups of 35 each using block-computerised randomisation technique (blocks of 10) and allocation concealment was achieved using sealed envelope technique.
Group ShB (n = 35): ShB using 10 ml of 0.5% bupivacaine each for SSN and AN block.
Group ISB (n = 35): ISB using 10 ml of 0.5% bupivacaine.
All patients underwent a detailed pre-anaesthetic check-up and kept fasting after midnight. An intravenous (IV) access was secured using 20-G cannula on the opposite hand.
Both the blocks were performed with dual assistance of high-frequency (10–12 Hz) 38-mm linear ultrasound transducer (Imagic Agile, Peachtree, Georgia) and peripheral nerve stimulator (Multistim-i3640, Pujunk) by an independent experienced anaesthetist (who had performed at least 20 ShB and ISB) in a block room 30 min before the anaesthesia induction. Preoperative measurements (baseline vital parameters, procedural duration, pain on injection, sensory and motor block) were noted by this person and handed over to the investigators. The procedural duration of the blocks was defined as the time that block needle was under the skin.
The investigator assessing the intraoperative and postoperative outcomes was blinded to the group allocation. For ensuring blinding, opaque adhesive tape was applied following the block to all the three proposed needle entry points.
For performing ISB, the roots of brachial plexus were visualised in supine position. A 22-G 50-mm nerve block needle was inserted in-plane and LA was injected in aliquots after eliciting response distal to deltoid muscle at 0.4 mA. SSN block was performed using Harmon and Hearty's technique, while AN block was performed using Rothe et al.[10] technique in sitting position using linear ultrasound probe and 22-G 100-mm nerve block needle in plane.[9] Evoked motor response (supraspinatus/infraspinatus for SSN and deltoid for AN) was elicited at 0.5 mA and LA was injected.
Success of sensory block (0 = no block; normal sensation; 1 = partial; a touch of pinprick but no pain; and 2 = complete; absence of sensation to pinprick) and motor block (0 = no block; normal movements of the shoulder, arm, and forearm, 1 = partial block; inability to perform movements against resistance and 2 = complete loss of motor power) was assessed after 30 min, on a 3-point scale.
The sensory block was assessed over C5–C7 dermatomes for ISB (C5 – skin over deltoid, C6 – thumb tip, C7 – middle fingertip) and for ShB, lateral aspect shoulder (regimental badge area, supplied by the AN). Motor block was assessed as restriction of shoulder abduction and elbow flexion for ISB and as restriction of shoulder abduction and external rotation for ShB. Patients with complete block failure at 30 min were excluded. Immediate complications, such as paraesthesia, Horner's syndrome, respiratory distress etc., were assessed.
After 30 min, anaesthesia was induced with IV fentanyl (2 μg/kg) and propofol (2–2.5 mg/kg) and intubation performed using vecuronium (0.1 mg/kg). Anaesthesia was maintained by nitrous-oxide and isoflurane to achieve a minimum alveolar concentration (MAC) of 1. If haemodynamic parameters increased >20% above baseline, inj. fentanyl (1 μg/kg) was administered.
Primary outcome was postoperative pain at time '0' (after the patient was shifted to recovery) which was assessed using VAS [0 (no pain) to 10 (worst pain)]. Secondary outcomes were pain scores at times 2, 4, 6, 12 and 24 h using VAS, block performance time, sensory and motor blockade, haemodynamic parameters, intraoperative fentanyl requirement and any adverse effects.
Rescue analgesia in the form of Inj. paracetamol 1 g IV was administered on demand or if VAS was ≥ 4 (maximum 4 doses, 6 h apart). Inj. tramadol 50 mg was administered to patients having inadequate pain relief within 6 h of paracetamol as secondary rescue analgesic. Time of first rescue analgesia (the time from operating room discharge until the first dose of rescue analgesia) and total analgesia required (number of times analgesic rescue doses) were noted. Satisfaction in terms of overall quality of pain relief was rated by the patient at the end of 24 h as excellent, good, fair, and poor.
In a previous study by Lee et al.,[12] the mean VAS at 0 h (in the post-anaesthesia care unit) in ISB group was found to be 1.4 ± 1.2 and in shoulder block group was 3.6 ± 1.9. Considering these values as reference, with minimal clinically important difference of 1.5 in mean VAS at 0 h and SD of 1.9, we needed 35 patients/group with 90% power and 5% two-sided level of significance. So, we decided to take the total sample size as 70.
The analysis was done with the use of Statistical Package for the Social Sciences (SPSS) version 21.0 (Armonk, NY: IBM). The categorical data were expressed as numbers (percentages) while continuous data were presented as mean ± standard deviation (SD) and median values. The data normality was checked by using the Kolmogorov–Smirnov test. The comparison of the variables, which were quantitative and normally distributed, was analysed using independent t-test [e.g., weight, BMI, heart rate, mean arterial pressure (MAP)]. Mann–Whitney test was used to analyse non-parametric data (age, height, duration of block, surgery and analgesia, VAS). The comparison of qualitative variables (gender, ASA, sensory block, motor block, complications, patient satisfaction, number of times analgesics received) was analysed using Chi-square test/Fisher's exact test. The statistically significant difference was considered as a P value <0.05.
RESULTS
Eighty patients between 18 and 60 years of age, posted for arthroscopic Bankart repair surgery, were assessed for eligibility and after screening for exclusion criteria, remaining 70 patients were included [Figure 1].
Figure 1.
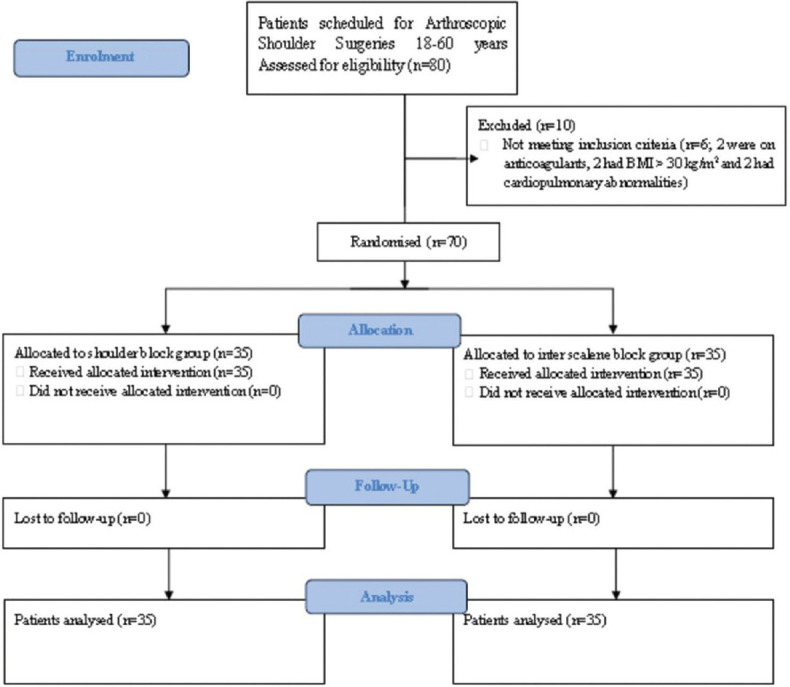
CONSORT flow diagram
The demographic profile was comparable in the two groups [Table 1]. The mean time for block performance was significantly more in group ShB (9.8 min vs. 3.8 min) (P < 0.0001).
Table 1.
Demographic characteristics of the patients
| Group | SHB (n=35) | ISB (n=35) | P |
|---|---|---|---|
| Age (years) | 26.97 (7.67) | 27.29 (6.41) | 0.638 |
| Gender (male/female) | 31/4 | 30/5 | 1.000 |
| Weight (kg) | 71.77 (13.39) | 70.11 (13.06) | 0.602 |
| Height (cm) | 169.74 (8.7) | 170.03 (7.71) | 0.911 |
| BMI (kg/m2) | 24.99 (3.66) | 24.03 (3.64) | 0.274 |
| ASA PS* (1/2) | 32/3 | 33/2 | 1.000 |
| Duration of surgery (min) | 55.34 (10.99) | 53.6 (10.98) | 0.485 |
The data are presented as number or mean (Standard deviation). *ASA PS: American Society of Anesthesiologists physical status, BMI: Body mass index
The sensory blockade score was comparable (P = 1.0). The motor blockade was partial in all patients in group ShB, whereas complete motor blockade was seen in 88.57% of ISB patients (P < 0.0001). Intraoperative fentanyl was required in 1 (2.86%) patient in ShB and 2 (5.71%) patients in ISB (P = 0.602). The perioperative variation in heart rate [Figure 2], MAP and SPO2 between the groups was similar.
Figure 2.
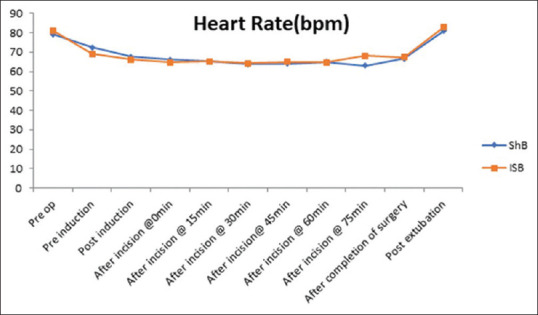
Heart rate in the two groups
The VAS was similar in the two groups at 0, 6 and 24 h [Figure 3]. VAS at 2 h (P = 0.001) and 4 h (P = 0.000) was higher in ShB group, whereas VAS was higher in ISB (P = 0.013) at 12 h. Mean analgesic duration was significantly longer with ISB (8.22 h vs. 4.69 h; P = 0.002) [Table 2]. Analgesia was required only once in 30 (85.7%) in ShB and 24 (68.6%) in ISB, whereas repeat dose was needed in 2 (5.7%) and 3 (8.6%) patients. Analgesia was not required in three (8.6%) patients in ShB and eight (22.9%) in ISB. The cumulative analgesic requirement was similar over 24 h in both the groups (P = 0.208). None of the patients required secondary rescue analgesics.
Figure 3.
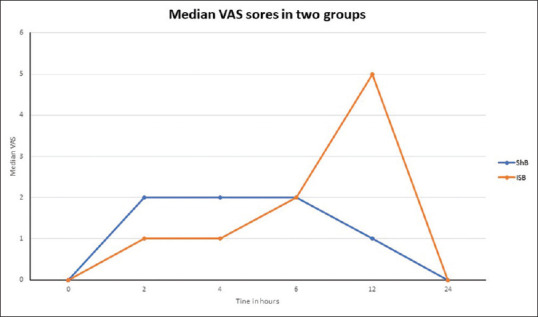
Median VAS in the two groups
Table 2.
Block characteristics in the two groups
| Group | SHB (n=35) | ISB (n=35) | P |
|---|---|---|---|
| Duration of block procedure (min) | 9.8 (1.39) | 3.83 (0.79) | <0.0001 |
| Sensory block (partial/complete) | 0/35 | 2/33 | 1.000 |
| Motor block (partial/complete) | 35/0 | 2/33 | <0.0001 |
| Complications (none/pain on injection/dyspnoea/ptosis) | 32/3/0/0 | 31/1/1/2 | 0.260 |
| Duration of analgesia (h) | 4.69 (2.01) | 8.22 (4.2) | 0.002 |
| Median (IQR) VAS | |||
| 0 | 0 [1-2] | 0 [0-0] | 0.320 |
| 2 | 2 [1-2] | 1 [0-2] | 0.001 |
| 4 | 2 [2-6] | 1 [0-2] | 0.000 |
| 6 | 2 [0-6] | 2 [0-2] | 0.170 |
| 12 | 1 [0-2] | 5 [0-7] | 0.013 |
| 24 | 0 [0-1] | 0 [0-1] | 0.909 |
| Number of times paracetamol was given in 24 h (none/once/twice) | 3/30/2 | 8/24/3 | 0.208 |
| Number of patients who required intraoperative fentanyl supplement (Y/N) | 1/34 | 2/33 | 0.602 |
| Patient satisfaction at 24 h (excellent/good/fair/poor) | 15/15/5/0 | 17/14/4/0 | 0.873 |
| Motor weakness/paraesthesia at 6 h | 0 | 23 | <0.001 |
| Motor weakness/paraesthesia at 12 h | 0 | 5 | 0.008 |
The data are presented as number; mean (Standard deviation) or median (Interquartile Range). VAS-Visual analogue scale;IQR-Interquartile range
Incidence of motor weakness was comparable between the groups at 0, 2, 4 and 24 h but it was significantly higher in ISB group at 6 (P < 0.001) and 12 h (P = 0.008) [Table 2]. The block complications like dyspnoea, ptosis and extensive motor blockade were observed only in the ISB group [Figure 4]. The patient satisfaction score was comparable between the groups [P = 0.873; Table 2].
Figure 4.
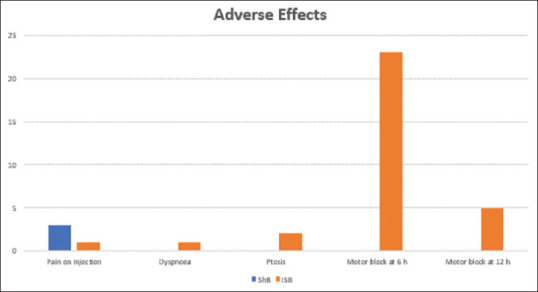
Adverse effects in the two groups
DISCUSSION
The findings of the present study indicate that a single-shot dual guidance ShB is a safe and effective technique for arthroscopic Bankart repair. As compared to ISB, ShB resulted in similar analgesic consumption and patient satisfaction with reduced motor block and less adverse events.
Pain following shoulder surgery is very intense and interferes with initial recovery and rehabilitation which necessitates opiate therapy.[13] The analgesic efficacy of ISB for analgesia following shoulder surgeries has been attested in literature.[1,3] Nevertheless, the occurrence of several potentially serious complications has necessitated the search for more selective safer blocks.[2,5] SSN block alone may be effective but the quality of analgesia provided is inferior to ISB,[6] because it provides innervation to 60–70% of the shoulder joint only and the rest 25–30% innervation of the shoulder joint is by AN.[10,14] Hence, combined blockade of the two should result in almost complete phrenic nerve-sparing analgesia of the joint. However, the time required for the block is significantly increased due to the need to block two different nerves.[11,12,15]
Motor blockade was partial in 100% in ShB patients, whereas ISB resulted in a complete motor block in 88.6% of patients because ISB paralyses muscles of the entire upper limb. In contrast, motor blockade with ShB is confined to posterior rotator cuff muscles and deltoid only. Correspondingly, the incidence of postoperative motor weakness and paraesthesia was significantly higher in ISB group (66% vs. 0% at 6 h). Despite the excellent quality of analgesia with ISB, extensive upper limb paralysis remains a significant cause of discomfort. Dhir et al.[11] also reported significantly higher motor weakness with ISB. Pani et al.[16] reported residual muscle weakness in all ISB cases in their study as they used a high concentration of LA (0.75% ropivacaine). This also resulted in lower satisfaction scores with ISB in their study.
The first analgesic requirement in the ISB group was significantly delayed in the ISB group (8.2 h vs. 4.6 h) and 4 h VAS was significantly higher in ShB which could be because of pain due to overdistension of the joint capsule caused by irrigation fluid used intra-operatively, as it takes up to 12 h to get absorbed.[11] In ShB group, this resulted in some extent of pain because of sparing of contributions from lateral pectoral, subscapularis and musculocutaneous nerves (innervating anterior joint capsule).[8,13] The superior articular branch of the SSN may leave the nerve before it enters suprascapular fossa.[14] This also resulted in an early time to first analgesic request with ShB. Proximal blockade by ISB provides more complete coverage of shoulder joint and provides excellent early postoperative analgesia. Previous researchers have also reported superior pain control in the early postoperative period with ISB.[11,12,15]
VAS at 12 h was significantly higher in ISB (P = 0.008). This can be explained because of rebound pain phenomenon due to wearing off of the ISB and this has been reported by various authors previously.[11,12,17] A meta-analysis conducted by Abdallah et al.[18] had concluded that ISB can provide efficient analgesia up to 8 h and there were no discernible advantages afterwards. Lee et al.[12] had documented a consistent pain relief with minimal variation in pain scores with ShB while there was a wide variation with ISB. Demarco et al.[17] reported rebound pain after 20 h; early rebound pain in our study may be due to lesser drug volume used for ISB. VAS scores at 24 h were comparable as reported in previous studies also.[11,15,16,19] Delayed pain relief is said to be better with ShB as LA blocks a distal smaller peripheral nerve in a less vascular area for a prolonged period as compared to large central nerve roots.[11,15]
In the current study, both the blocks provided equivalent postoperative analgesia, cumulative analgesic requirement which is in agreement with the results of previous researchers.[15,16,19] Waleed found similar analgesic requirements and patient satisfaction with both blocks in concordance with our study.[20] However, VAS scores in their study were comparable at all time points, probably because they did not specify the type of procedures while we had uniformly included Bankart repair procedures, a major arthroscopic surgery. Another reason could be the different type and concentration of LA used (0.25% levobupivacaine). They noted a higher incidence of complications with ISB, presumably due to twice the volume of LA.[20]
Dyspnoea was seen in one patient (2.9%) and ptosis was seen in two patients (5.7%) in the ISB group while no complications were recorded in the ShB group. Both groups demonstrated stable haemodynamics which is of key importance in arthroscopic surgery as they relate to pump pressures and intra-articular bleed.[21] Dyspnoea and ptosis are common complications of ISB and result from the diffusion of LA anteriorly to block ipsilateral phrenic nerve and paravertebrally to block the cervical sympathetic chain. Previous trials have also reported higher complications with ISB as compared to ShB.[16,19,22] However, the incidence of complications reported in their study was much higher as compared to our study probably due to a higher volume or concentration of LA used.
Satisfaction level at 24 h was comparable in the two groups and none reported poor level of satisfaction. Pitombo et al.[15] also established that both techniques were safe, effective and had similar satisfaction scores. Various other researchers have also reported a high level of patient satisfaction with ShB.[7,11,15,22]
Our study has a few limitations. First, the blocks were done by a skilled operator, so the results may not be the same in hands of inexperienced operators. Second, patient blinding was not feasible because of the different sites of injection. However, the investigators assessed the outcome variables without being involved in the block procedure, thereby minimising any possibility of bias. Third, diaphragmatic palsy was assessed only by subjective complaints of dyspnoea and not objectively demonstrated using ultrasonography and spirometry. However, phrenic nerve blockade is expected to occur in most patients with the LA volume used in the current study while ShB is a diaphragm sparing block.[23] Lastly, VAS scores were assessed only at rest and dynamic scores could not be assessed because of the application of shoulder brace by the surgeons.
CONCLUSION
ShB and ISB have similar efficacy in terms of VAS in recovery, cumulative analgesic requirement, and patient satisfaction. ISB prolonged the time to first analgesic request but resulted in significantly higher delayed rebound pain. Considering the undesirable effects associated with ISB like phrenic nerve blockade, prolonged upper limb weakness and the occurrence of rebound pain, ShB may be preferred for arthroscopic shoulder surgeries.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors would like to thank Dr. Saveena G. Raheja (Medical officer, Anaesthesiology, VMMC and Safdarjung hospital), Dr. Bhawna Garg (Statistician) and Dr. Deepak Joshi (Professor and specialist Orthopaedic, VMMC and Safdarjung Hospital) for their incessant support and valuable inputs in this manuscript.
REFERENCES
- 1.Beecroft CL, Coventry DM. Anaesthesia for shoulder surgery. Br J Anaesth. 2008;8:193–8. [Google Scholar]
- 2.Wahal C, Kumar A, Pyati S. Advances in regional anaesthesia: A review of current practice, newer techniques and outcomes. Indian J Anaesth. 2018;62:94–102. doi: 10.4103/ija.IJA_433_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fredickson MJ, Krishnan S, Chen CY. Postoperative analgesia for shoulder surgery: A critical appraisal and review of current techniques. Anaesthesia. 2010;65:608–24. doi: 10.1111/j.1365-2044.2009.06231.x. [DOI] [PubMed] [Google Scholar]
- 4.Park HS, Kim HJ, Ro YJ, Yang HS, Koh WU. Delayed bilateral vocal cord paresis after a continuous interscalene brachial plexus block and endotracheal intubation: A lesson why we should use low concentrated local anesthetics for continuous blocks. Medicine (Baltimore) 2017;96:e6598. doi: 10.1097/MD.0000000000006598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jadon A, Nage S, Swarupa CP, Motaka M. Weakness of contralateral upper limb after interscalene block – A case report. Indian J Anaesth. 2019;63:55–7. doi: 10.4103/ija.IJA_554_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cho N, Kang RS, McCartney CJL, Pawa A, Costache I, Rose P, et al. Analgesic benefits and clinical role of the posterior suprascapular nerve block in shoulder surgery: A systematic review, meta-analysis and trial sequential analysis. Anaesthesia. 2020;75:386–94. doi: 10.1111/anae.14858. [DOI] [PubMed] [Google Scholar]
- 7.Checcucci G, Allegra A, Bigazzi P, Gianesello L, Ceruso M, Gritti G. A new technique for regional anaesthesia for arthroscopic shoulder surgery based on a suprascapular nerve block and an axillary nerve block: An evaluation of the first results. Arthroscopy. 2008;24:689–96. doi: 10.1016/j.arthro.2008.01.019. [DOI] [PubMed] [Google Scholar]
- 8.Price DJ. The shoulder block: A new alternative to interscalene brachial plexus blockade for the control of postoperative shoulder pain. Anaesth Intensive Care. 2007;35:575–81. doi: 10.1177/0310057X0703500418. [DOI] [PubMed] [Google Scholar]
- 9.Harmon D, Hearty C. Ultrasound guided suprascapular nerve block technique. Pain Physician. 2007;10:743–6. [PubMed] [Google Scholar]
- 10.Rothe C, Asghar S, Andersen HL, Christensen JK, Lange KH. Ultrasound guided block of the axillary nerve: A volunteer study of new method. Acta Anesthesiol Scand. 2011;55:565–70. doi: 10.1111/j.1399-6576.2011.02420.x. [DOI] [PubMed] [Google Scholar]
- 11.Dhir S, Sondekoppam RV, Sharma R, Ganapathy S, Athwal SG. A comparison of combined suprascapular and axillary nerve blocks to interscalene nerve block for analgesia in arthroscopic shoulder surgery: An equivalence study. Reg Anesth Pain Med. 2016;41:564–71. doi: 10.1097/AAP.0000000000000436. [DOI] [PubMed] [Google Scholar]
- 12.Lee SM, Park SE, Nam YS, Han SH, Lee KJ, Kwon MJ, et al. Analgesic effectiveness of nerve block in shoulder arthroscopy: Comparison between interscalene, suprascapular and axillary nerve blocks. Knee Surg Sports Traumatol Arthrosc. 2012;20:2573–8. doi: 10.1007/s00167-012-1950-5. [DOI] [PubMed] [Google Scholar]
- 13.Basat HC, Uçar DH, Armangil M, Güçlü B, Demirtaş M. Post operative pain management in shoulder surgery: Suprascapular and axillary nerve block by arthroscope assisted catheter placement. Indian J Orthop. 2016;50:584–9. doi: 10.4103/0019-5413.193474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang KV, Wu WT, Hung CY, Han DS, Yang RS, Chang CH, et al. Comparative effectiveness of suprascapular nerve block in the relief of acute post-operative shoulder pain: A systematic review and meta-analysis. Pain Physician. 2016;19:445–56. [PubMed] [Google Scholar]
- 15.Pitombo PF, Barros RM, Matos MA, Modolo NSP. Selective supra-scapular and axillary nerve block provides adequate analgesia and minimal motor block; comparison with interscalene block. Rev Bras Anesthesiol. 2013;63:45–58. doi: 10.1016/S0034-7094(13)70197-1. [DOI] [PubMed] [Google Scholar]
- 16.Pani N, Routray SS, Pani S, Mallik S, Pattnaik S, Pradhan A. Post-operative analgesia for shoulder arthroscopic surgeries: A comparison between inter-scalene block and shoulder block. Indian J Anaesth. 2019;63:382–7. doi: 10.4103/ija.IJA_65_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DeMarco JR, Componovo R, Barfield WR, Liles L, Nietert P. Efficacy of augmenting a subacromial continuous-infusion pump with a preoperative interscalene block in outpatient arthroscopic shoulder surgery: A prospective, randomized, blinded, and placebo-controlled study. Arthroscopy. 2011;27:603–10. doi: 10.1016/j.arthro.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 18.Abdallah FW, Halpern SH, Aoyama K, Brull R. Will the real benefits of single-shot interscalene block please stand up.A systematic review and meta-analysis? Anesth Analg. 2015;120:1114–29. doi: 10.1213/ANE.0000000000000688. [DOI] [PubMed] [Google Scholar]
- 19.Zanfaly HE, Aly AA. Shoulder block versus interscalene block for postoperative pain relief after shoulder arthroscopy. Ain-Shams J Anesthesiol. 2016;9:296–303. [Google Scholar]
- 20.Waleed A. Postoperative analgesia for arthroscopic shoulder surgery: Comparison between ultrasound-guided interscalene block and combined suprascapular and axillary nerve blocks. Ain-Shams J Anaesthesiol. 2016;9:536–41. [Google Scholar]
- 21.Tantry TP, Karanth H, Shenoy SP, Shetty PK, Bhandary S, Adappa KK. Sevoflurane versus isoflurane in shoulder arthroscopy in beach chair position in patients with prior interscalene brachial plexus block: A prospective randomised equivalency-based haemodynamic evaluation trial. Indian J Anaesth. 2018;62:793–801. doi: 10.4103/ija.IJA_376_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Neuts A, Stessel B, Wouters PF, Dierickx C, Cools W, Ory JP, et al. Selective suprascapular and axillary nerve block versus interscalene plexus block for pain control after arthroscopic shoulder surgery: A noninferiority randomised parallel controlled clinical trial. Reg Anesth Pain Med. 2018;43:1091–108. doi: 10.1097/AAP.0000000000000777. [DOI] [PubMed] [Google Scholar]
- 23.Sinha SK, Abrams JH, Barnett JT, Muller JG, Lahiri B, Bernstein BA, et al. Decreasing the local anesthetic volume from 20 to 10 ml for ultrasound-guided interscalene block at the cricoid level does not reduce the incidence of hemi diaphragmatic paresis. Reg Anesth Pain Med. 2011;36:17–20. doi: 10.1097/aap.0b013e3182030648. [DOI] [PubMed] [Google Scholar]


