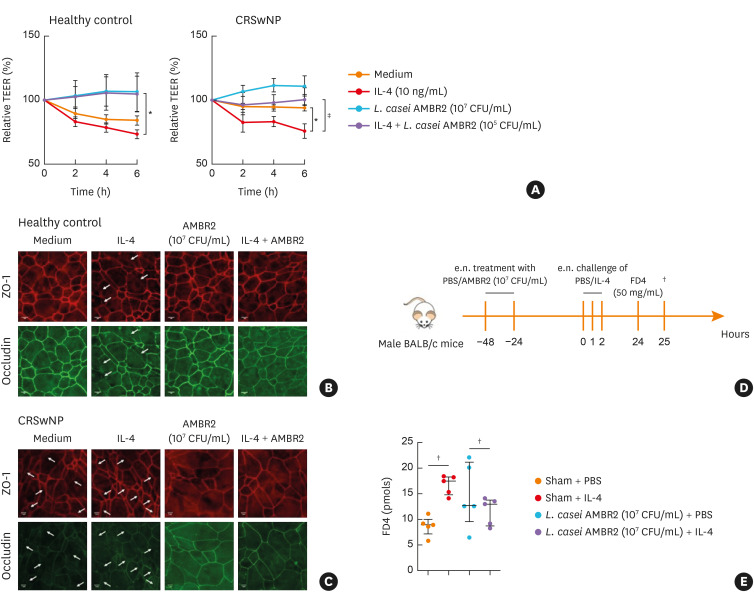
Fig. 4. The effect of L. casei AMBR2 on IL-4 induced barrier dysfunction in vitro and in vivo. (A) Effect of L. casei AMBR2 with/without IL-4 on TEER of epithelial cell cultures of healthy controls (n = 5) and patients with CRSwNP patients (n = 6). (B, C) Representative immunostainings for occludin and ZO-1 from stimulated ALI cultures of healthy controls and patients with CRSwNP. White arrows indicate the opening of the tight junctions (scale bar = 1 μm). (D) Mice were endonasally pre-treated two times with L. casei AMBR2 (107 CFU/mL). Twenty-four hours later, IL-4 was applied three times with one hour interval. Twenty-four hours after the last IL-4 application, FD4 was applied endonasally to evaluate mucosal permeability in the serum of the treated mice. (E) Mucosal permeability for FD4. Data are presented as mean ± SEM. Two-way ANOVA with post hoc analysis for (A). Mann-Whitney test for (D).
CRSwNP, chronic rhinosinusitis with nasal polyps; TEER, trans-epithelial electrical resistance; IL, interleukin; FD4, fluorescein isothiocyanate-dextran 4 kDa; SEM, standard error of mean; ANOVA, analysis of variance; CFU, colony-forming unit; PBS, phosphate-buffered saline; ZO-1, zonula occludens-1.
*P < 0.05; †P < 0.01; ‡P < 0.001.