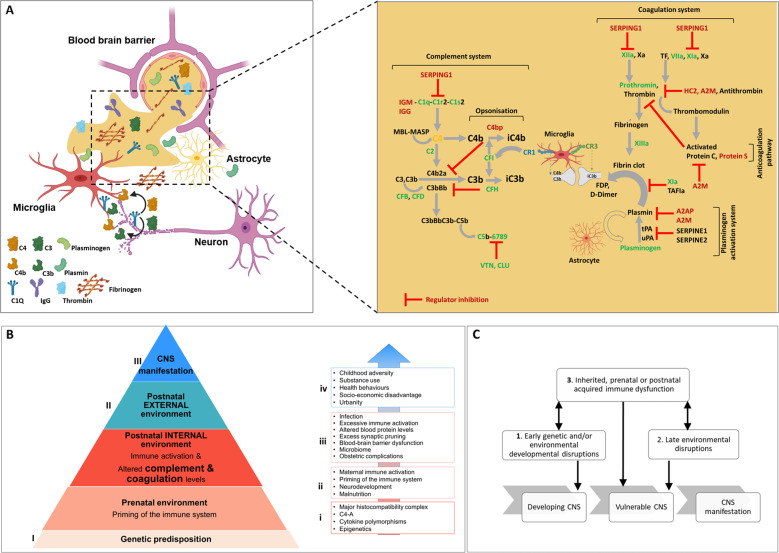
Fig. 2. Mechanism by which infection and inflammation (inherited and acquired risk) influence the progression to psychosis.
A Complement and coagulation proteins and pathways show upregulated components in green (proteomics studies) or blue (transcriptomic studies). Downregulated components are shown in red. Regulatory interactions are highlighted with an inhibition arc colored in red ├. Genetic variant is shown in orange. A blood-brain barrier (BBB) cross-section with complement and coagulation proteins at the neurovascular interface and extravasation into the central nervous system (CNS) following disintegration of the BBB. Activation of the coagulation and plasminogen activation and complement system promoting inflammation and microglia-mediated cellular damage. B The pyramid describes the cumulative risk factors in the progression toward psychosis spectrum disorders illustrating the integrated impact of genetic predisposition and prenatal environment (priming of the immune system), postnatal internal environment (immune activation, altered complement, and coagulation levels), postnatal external environment, leading to central nervous system (CNS) manifestation. Notably, each risk factor is not considered in isolation but as a significant contributing factor and each of the “hits” may have an additive effect on the progression to psychotic disorder. Points of risk assessment and intervention: (I) Risk assessment and stratification, e.g., prenatal environment and genetic risk association, (II) stratification, e.g., clinical high risk (CHR), proposed predicative blood biomarkers and intervention, e.g., cognitive behavioral therapy (CBT), Omega-3 supplementation and proposed anti-inflammatory (complement) and anticoagulant therapeutics. (III) Intervention, e.g., cognitive behavioral therapy (CBT) and antipsychotic drugs. The box and arrow breaks down the individual components as bullet points associated with (i) genetic predisposition, (ii) prenatal environment, (iii) postnatal internal environment, and (iv) postnatal external environment. C The two-hit hypothesis of schizophrenia states that early genetic and/or environmental developmental disruptions (“first-hit”) to the developing central nervous system (CNS) increase the vulnerability of the individual to subsequent, late environmental disruptions (“second-hit”), leading to the development of CNS manifestation. The multiple-hit theory introduces another hit of inherited, prenatal, or postnatal acquired immune dysfunction that sets complement and coagulation pathway activating capacity and regulatory ability integral to development of psychotic disorder (adapted from [12]). A2M alpha-2-macroglobulin, APC activated protein C, AT antithrombin, C1Q complement component 1q, C1r complement C1r subcomponent, C1S complement component 1s, C2 complement C2, C3 complement C3, C3b is the larger of two elements formed by the cleavage of complement component 3, opsonins, C3bBb complement C3 convertase, C4 complement C4, C4b is the larger of two elements formed by the cleavage of complement component 4, opsonin, C4b2a complement C3 convertase, C5b6789 membrane-attack complex, CFB complement factor B, CFD complement factor D, CFH complement factor H, CLU clusterin, D-dimer a fibrin degradation product, FDP fibrin degradation products, FII prothrombin; HC2 heparin cofactor II or SERPIND1, iC3b inactive component 3b, opsonin, IGG immunoglobulin G, IGM immunglobulin M, MASP mannose-associated serine protease, MBL mannose-binding lectin, PAI-1 plasminogen activator inhibitor-1, PROS vitamin K-dependent protein S, SERPING1 plasma protease C1 inhibitor, TF tissue factor, tPA tissue plasminogen activator, VIIa plasma factor VIIa, VTN vitronectin, Xa factor Xa, XIa factor XIa, XIIa factor XIIa, XIIIa factor XIIIa, an enzyme of the blood coagulation system that crosslinks fibrin.