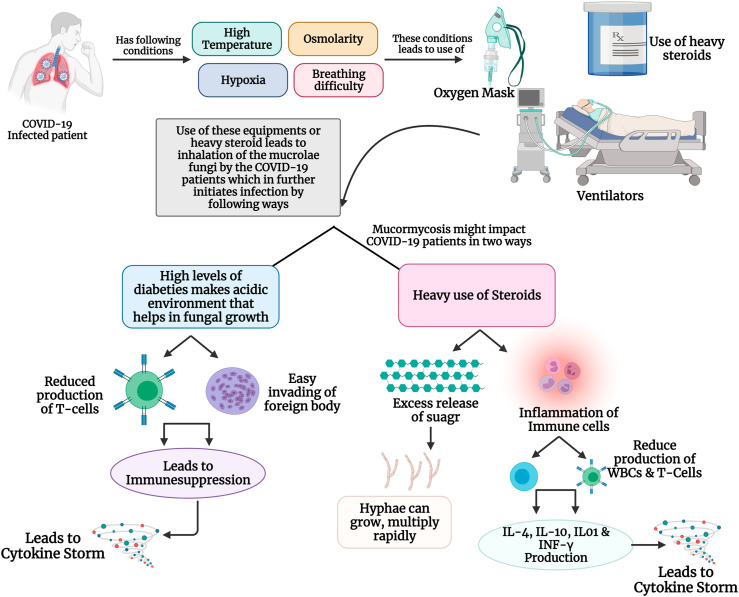
Fig. 3.
(A): Mechanism of mucormycosis in healthy individuals: When the Mucorales enters an immune-compromised patient through inhalation, or through wounds, it is initially gets attached to the epithelial cells receptor using its CotH receptors. Further, the PDGFRB signaling pathways provides essentials for the proper development and growth of the fungal hyphae. Also, if the patients have diabetes, ketoacidosis and hyperglycaemia damage the neutrophils, making it easy for the fungi spread. Once the fungi are developed it starts to produce Mucorales-specific T cells which has various pro-inflammatory cells such as IL-4, IL-10, IL-17, IFN-γ, which triggers the cytokine storm resulting into cellular damages. (B): Possible mechanism of mucormycosis in COVID-19 infected patients: Mucormycosis is becoming common among COVID-19 patients, especially due to physiological stressors such as high body temperature osmolarity, hypoxia which are common conditions when affected with SARS-CoV-2. Also, these patients undergo heavy intake of steroids, use oxygen masks and ventilators to combat SARS-CoV-2 infection, which turns as an entry pass to the body for the Mucorales fungus. Further, this fungal infection could impact the COVID-19 in two-way scenario: 1) when the COVID-19 patients who have diabetes as co-morbidity, create an acidic environment that enables a unique environment for these fungi to grow. Also, due to hyperglycaemia, there is a decrease production of T-cells and immunosuppression, resulting in a cytokine storms. 2) heavy intake of steroids also release a huge amount of sugar which helps in the rapid multiplication and growth of fungal hyphae. Also, steroids tend to inflammation the immune cells leading to cytokine storm and damage to cellular organs.