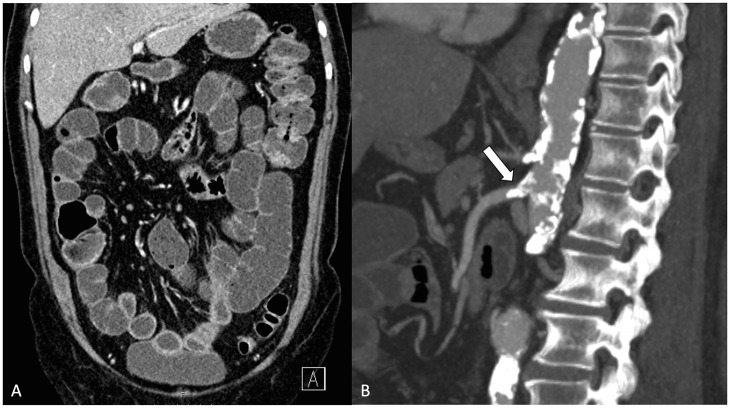
Fig. 5.
This 70-year-old patient had suffered from postprandial pain and diarrhea for 2 months prior to the final admission. The symptoms worsened and became persistent, and the patient was admitted to the emergency room. C-reactive protein was 400 mg/L. A) Computed tomography showed dilated small bowel loops, bowel wall thickening, mesenteric fat stranding, and abnormal increased enhancement of the intestine. B) All mesenteric arteries were severely obstructed by atherosclerotic disease. Based on the vascular and intestinal findings in the imaging, appropriate clinical presentation, and absence of a competing cause, the diagnosis of acute-on-chronic mesenteric ischemia was made. An exploratory laparotomy was performed mainly due to the high inflammatory markers and clinical suspicion of bowel necrosis. The small bowel appeared pale and cyanotic. However, there was no irreversible bowel damage, and subsequent endovascular stenting of the proximal superior mesenteric artery stenosis (arrow) was performed. The patient recovered without need for bowel resection.