Abstract
Purpose of Review
The orthotopic neobladder and ileal conduit are the two most commonly utilized urinary diversions among patients undergoing radical cystectomy. Although orthotopic diversion offers several advantages, only 20% of patients nationally receive this diversion, with decreasing utilization over time. The purpose of this articles is to review advantages of each diversion type and considerations in patient selection, review trends in diversion utilization and perioperative and functional outcomes, and examine recent studies evaluating methods of optimizing diversion selection and patient satisfaction and outcomes.
Recent findings:
Decreasing utilization of orthotopic diversion has coincided with the increasing utilization of minimally-invasive surgical techniques. A multicenter robotic series demonstrated a higher incidence of high-grade complications with intracorporeal diversion, reflecting the learning-curve associated with this technique. Patient satisfaction with urinary diversion is associated with informed decision-making and goal alignment. Ongoing quality of life studies are aiming to identify predictors of patient satisfaction with the selected urinary diversion and may help guide patient counseling.
Summary:
Given the potential advantages of orthotopic diversion, its decreasing use is a concerning trend. Elucidating patient goals and informed decision-making are critical to patient satisfaction. A patient-centered approach should be used when selecting the type of urinary diversion for a given patient.
Keywords: Orthotopic neobladder, Ileal conduit, Outcomes, Quality of Life
Introduction
Radical cystectomy with urinary diversion remains the gold standard for management of muscle-invasive bladder cancer and select patients with high risk non-muscle invasive bladder cancer. While several options for urinary tract reconstruction are available, the most commonly utilized urinary diversions are the incontinent ileal conduit and the continent orthotopic neobladder.1,2 Each diversion offers specific advantages with respect to perioperative and functional outcomes that must be considered in selecting the best diversion for a given patient. Although there are a few well-defined absolute contraindications, most patients undergoing radical cystectomy are candidates for orthotopic urinary diversion, including elderly patients (>70 years old). Providing an excellent long term quality of life, orthotopically reconstructed patients appear to be at no higher risk of perioperative complication with this diversion type.3 However, multiple large series4–6 and population-based studies1,2 have demonstrated decreasing utilization of continent urinary diversions over time. This trend has coincided with the increasing adoption of robotic-assisted surgical approaches to radical cystectomy. In fact, multiple robotic radical cystectomy series5,6 and a multicenter randomized trial of open versus robotic cystectomy7 have reported low utilization of continent urinary diversions. Furthermore, studies examining functional outcomes among patients undergoing a minimally-invasive surgical approach, including use of intracorporeal urinary diversion, are limited to small series.8,9
In this review, we review the advantages and disadvantages to orthotopic neobladder and ileal conduit urinary diversion, examine trends in the use of urinary diversion types with the increasing utilization of robotic-assisted surgical approaches, and review recent literature and areas of ongoing study in methods of optimizing patient goal alignment and postoperative satisfaction with urinary diversion.
Patient Selection
Selection of urinary diversion depends on several important considerations, including extent of disease, medical comorbidity, prior pelvic therapy (surgery and radiation), and patient preferences. Although most patients undergoing radical cystectomy are candidates for orthotopic diversion, there are a few absolute contraindications including overt urethral involvement, a positive urethral margin at the time of cystectomy, severe renal or hepatic impairment, extensive inflammatory bowel disease, or physical or mental impairment precluding performance of intermittent catheterization. In all other patients, the advantages of each diversion type must be considered within the context of a given patient and his or her preferences with respect to safety and health-related quality of life.
Considerations of the ileal conduit urinary diversion
The ileal conduit is a technically simple diversion to construct and is often selected in older or comorbid patients due to the shorter operative time, limited bowel needed for reconstruction and lower risk of complication associated with this diversion type.10 Despite these advantages, early and late complications remain common, with gastrointestinal, infectious, and wound complications being most commonly observed in the early post-operative period.10,11 Importantly, late complications of ileal conduit diversion are also common in these patients. In a study of 131 patients who underwent ileal conduit diversion with at least five years of follow-up, Madersbacher and colleagues observed late (> 3 months from surgery) conduit-related complications in 66% of patients, with an increasing incidence of complications over time.12 Commonly observed late complications included renal functional or morphological changes (27%), stomal complications (24%), ureteral anastomotic complications (14%), and urolithiasis (9%). These observations highlight the need for continued long-term surveillance of these patients.
Stomal complications are a unique consideration of ileal conduit diversions. While stomal stenosis remains a rare complication in most series,11 parastomal hernias are common occurring in 30–50% of patients with intermediate follow-up.13–15 A series from Memorial Sloan Kettering demonstrated a 48% 2-year risk of radiographically confirmed parastomal hernia among 386 patient undergoing radical cystectomy with ileal conduit diversion. Sixty-eight percent of parastomal hernias were clinically evident and 27% symptomatic.13 Similar parastomal hernia rates have been reported in robotic cystectomy series.16 Higher body mass index and female gender have been shown to be associated with a greater risk of parastomal hernia. The high incidence of parastomal hernia, including a reoperation rate for parastomal hernia as high as 45% in one series,14 has led several investigators to examine surgical techniques to reduce parastomal hernia risk.
Multiple randomized controlled trials of the use of prophylactic parastomal mesh placement at the time of stoma creation in patients undergoing colostomy have demonstrated statistically and clinically significant reduction in the risk of parastomal hernia, without complication of fistula, stricture, or mesh infection.17 Early experience with prophylactic mesh placement among patients undergoing radical cystectomy with ileal conduit diversion in non-randomized studies suggest a lower incidence of parastomal hernia with use of mesh. A single-center study of 114 patients undergoing prophylactic mesh placement at the time of ileal conduit diversion demonstrated a 14% incidence of parastomal hernia with a 32-month median follow-up.18 No mesh-related complications have been reported in this series, or in our early experience.17 Two ongoing prospective randomized trials at Memorial Sloan Kettering and the University of Southern California will evaluate the impact of prophylactic mesh placement on risk of parastomal hernia.
Considerations of the orthotopic neobladder
Orthotopic neobladder represents an excellent option for urinary diversion for the appropriate candidate. As a continent diversion, most series report daytime continence approaching 90% with nighttime continence of approximately 70%,11 although studies applying objective definitions of incontinence by pad weight report lower continence rates.19 Some studies suggest improved body image, higher quality of life scores, and greater physical function among patients undergoing orthotopic neobladder,20–22 while others suggest similar quality of life outcomes between patients undergoing neobladder and ileal conduit diversions. These observations are associated, in part, with patient selection for the different diversion types. The risk of metabolic complication such as chronic metabolic acidosis or vitamin B12 deficiency is greater with orthotopic neobladder when compared to ileal conduit11 however both diversions require life-long monitoring. Severe renal insufficiency is a contraindication to orthotopic neobladder, due to an inability to handle the increased resorption of metabolic waste products in the urine and subsequent systemic acid load and electrolyte abnormalities. Since a small subset of men and a larger group of women that receive an orthotopic reconstruction have an inability to adequately empty to completeness, the physical inability or unwillingness to perform self-catheterization if needed remains a barrier for some patients to orthotopic diversion.23
Health related quality of life and decisional alignment after urinary diversion
Validated instruments, including bladder cancer-specific tools, have been developed to assess health related quality of life among patients undergoing radical cystectomy with urinary diversion. Multiple series have compared quality of life between patients undergoing ileal conduit and orthotopic neobladder urinary diversion. Prospective studies have demonstrated better quality of life scores among patients undergoing orthotopic neobladder diversion,20,21 including better patient-reported physical function and a more active lifestyle in one study.22 Other studies show similar patient-reported outcomes between the two diversion types, possibly due to differences in patient selection.24,25
Trends in use of orthotopic neobladder
Despite trends towards increased centralization of radical cystectomy at high volume centers in the United States,26 contemporary population-based studies have demonstrated decreasing utilization of orthotopic urinary diversion among patients undergoing radical cystectomy. A study of 4790 patients captured in the American College of Surgeons National Surgical Quality Improvement Program from 2011 to 2015 found that 81% of all patients undergoing radical cystectomy underwent an incontinent diversion.2 Use of orthotopic neobladder decreased over time, with year of surgery independently associated with receipt of an incontinent diversion. Population-based studies have demonstrated similar trends in Europe, with a nationwide German sample demonstrating significant decline in utilization of orthotopic neobladder from 33% in 2006 to 27% by 2014.1
Data from the National Cancer Database demonstrate increasing utilization of minimally-invasive surgical approaches for radical cystectomy over time.27 Multiple multicenter robotic cystectomy series have reported low utilization of continent diversion with robotic-assisted radical cystectomy. The phase 3 noninferiority trial of robotic and open radical cystectomy (RAZOR trial) included 302 patients in the per-protocol analysis, of whom 66 (22%) received orthotopic neobladder, with similar rates of utilization in the open and robotic arms.4 In a recently-published analysis of 2125 patients undergoing robotic cystectomy since 2005 from the International Robotic Cystectomy Consortium, 22% of patients received an orthotopic neobladder. This group observed a significant increase in use of intracorporeal urinary diversion over time, largely driven by the increase in intracorporeal ileal conduit urinary diversion.5 Importantly, a higher incidence of high-grade complications was observed among patients undergoing intracorporeal urinary diversion with decreasing incidence of major complication over time, highlighting the learning curve associated with intracorporeal surgical techniques.5
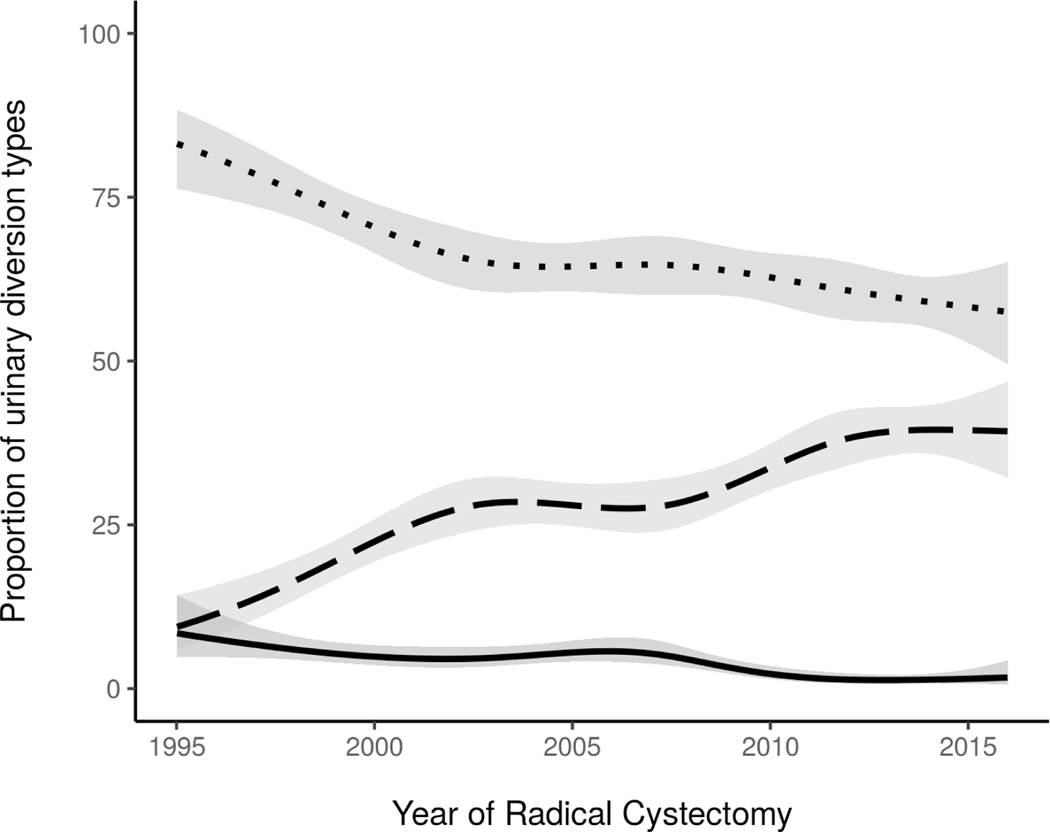
In contrast to these reports, a randomized controlled trial of open versus robotic radical cystectomy conducted at Memorial Sloan Kettering reported use of orthotopic neobladder urinary diversion in 55% of patients in each arm of the trial.28 Furthermore, in an analysis of 2911 patients with urothelial carcinoma undergoing radical cystectomy at Memorial Sloan Kettering from 1995 to 2015, we observed a rise in use of orthotopic neobladder from approximately 21% of all patients undergoing radical cystectomy in 1995 to 38% by 2015 (Figure 1). Given the potential advantages associated with orthotopic neobladder urinary diversion, it is imperative that the availability of this urinary diversion not be limited by the increasing utilization of minimally-invasive surgical approaches. While randomized trials have not shown significant differences in perioperative and oncologic outcomes between open and robotic radical cystectomy,4,29 functional outcomes in patients undergoing robotic radical cystectomy with orthotopic urinary diversions are not as well characterized, with mixed data from limited single-center studies. In one observational study of 70 patients undergoing robotic radical cystectomy with intracorporeal orthotopic neobladder, 88% of men and 67% of women reported daytime continence and 74–81% of men and 67% of women reported nighttime continence at 12 months, leading the authors to conclude that functional outcomes with intracorporeal orthotopic neobladder are comparable with open cystectomy series.30 Another observational study comparing 28 patients undergoing robotic cystectomy with intracorporeal orthotopic neobladder with 79 patients undergoing open radical cystectomy with orthotopic neobladder reported larger pad size and greater pad wetness among patients in the robotic group, suggesting possibly worse functional outcomes although this study was limited by small sample size.31 Further studies are needed to examine functional outcomes among patients undergoing robotic cystectomy with continent urinary diversion.
Figure 1 –
Adjusted rates of continent cutaneous urinary diversion (solid line, p<0.0001), ileal conduit urinary diversion (dotted line, p<0.0001) and orthotopic neobladder (dashed line, p<0.0001), by year of radical cystectomy, among 2911 patients with urothelial carcinoma undergoing radical cystectomy at Memorial Sloan Kettering Cancer Center from 1995 to 2015. Rates are adjusted for age.
Optimizing patient goal alignment in urinary diversion selection
Adequate counseling and patient education are critical to informed decision making and patient-centered goal alignment in selection of urinary diversion. In a longitudinal cohort study of 192 patients undergoing radical cystectomy, Check and colleagues found no difference in decisional regret among patients undergoing ileal conduit or orthotopic neobladder diversion. However, informed decision making was associated with diminished decisional regret and improved quality of life at 18 months after surgery.32 Using formative focus groups and individual interviews of patients who had undergone radical cystectomy, Leo and colleagues defined patient-identified goals specific to ileal conduit urinary diversion, such as having the shortest possible operation and avoiding having to relearn how to void, and to orthotopic neobladder, such as avoiding a urostomy bag and maintaining natural bodily function. Presence of goals specific to a urinary diversion type were associated with goal alignment in patients who received that diversion, and goal dissonance in patients who did not receive this diversion type.33 Importantly, these measures to elicit preoperative patient preference were identified on interview of patients 6 months after cystectomy. Other studies have demonstrated that before surgery patients primary concerns relate to cancer treatment and surgical recovery, whereas 6 months after surgery their priorities focus primarily on quality of life, return to work, regaining sense of normalcy, and quality of life.34 An ongoing prospective study evaluating baseline and postoperative quality of life will provide further insight into predictors of quality of life with each diversion type and may allow development of a clinical decision making tool to guide urinary diversion selection when counseling patients.
Conclusions
Ileal conduit and orthotopic neobladder are excellent options for urinary diversion that offer distinct advantages. Although similar quality of life outcomes have been observed between these two diversion types in several studies, some studies suggest greater quality of life and body image among patients undergoing orthotopic neobladder urinary diversion. Differences in patient selection for each diversion type however inhibits the ability to draw firm conclusions. Recent studies have identified patient treatment goals associated with post-operative decisional satisfaction with the selected urinary diversion, which may help in patient counseling and identifying the right diversion for a given patient. Ongoing studies will provide further insight into predictors of quality of life outcomes between these two urinary diversion types. The decreasing utilization of orthotopic neobladder coinciding with increased adoption of robotic surgical techniques, particularly intracorporal diversion, is a concerning trend. Ultimately informed decision-making through a patient-centered approach, which has been shown to be associated with diminished decisional regret and greater quality of life, and mastering of the technical challenges associated with minimally invasive reconstructive techniques should guide selection of urinary diversion for an individual patient.
Key Points.
Although most patients undergoing radical cystectomy are candidates for orthotopic urinary diversion, use of orthotopic neobladder is continuing to decrease among patients undergoing radical cystectomy.
Decreasing use of orthotopic neobladder urinary diversion has coincided with increased adoption of robotic radical cystectomy and increased utilization of intracorporeal urinary diversion at some centers.
Patient counseling and informed decision-making is associated with reduced risk of decisional regret in urinary diversion selection and greater quality of life, highlighting the importance of patient counseling in selecting the best urinary diversion for a given patient.
Ongoing and future studies are needed to model predictors of patient satisfaction with urinary diversion choice to optimize patient counseling and optimize clinical decision-making in selecting urinary diversions in a patient-centered model.
Additional studies are needed to evaluate functional outcomes among patients undergoing robotic radical cystectomy with orthotopic neobladder and to optimize utilization of orthotopic diversions with minimally-invasive surgical approaches.
Acknowledgements
1. Acknowledgements – The authors would like to thank Emily Vertosick and Dan Sjoberg of the Department of Epidemiology and Biostatistics at Memorial Sloan Kettering for their analysis of trends in use of urinary diversion types among patients undergoing radical cystectomy at Memorial Sloan Kettering from 1995 to 2015.
2. Financial support and sponsorship - This work was supported by the Sidney Kimmel Center for Prostate and Urologic Cancers and by National Institutes of Health/National Cancer Institute Cancer Center Support Grant P30 CA008748. N.A. was supported by National Institutes of Health T32 Ruth L. Kirschstein Institutional National Research Service Award
Footnotes
3. Conflicts of Interest – Nima Almassi has no conflicts of interest to report. Bernard H. Bochner serves as a consultant for Olympus.
References
- 1.Groeben C, Koch R, Baunacke M, et al. Urinary Diversion After Radical Cystectomy for Bladder Cancer: Comparing Trends in the US and Germany from 2006 to 2014. Ann Surg Oncol 2018;25:3502–3509. [DOI] [PubMed] [Google Scholar]
- 2.Bachour K, Faiena I, Salmasi A, et al. Trends in urinary diversion after radical cystectomy for urothelial carcinoma. World J Urol 2018;36:409–416. [DOI] [PubMed] [Google Scholar]
- 3.Clark PE, Stein JP, Groshen SG, et al. Radical cystectomy in the elderly: comparison of clincal outcomes between younger and older patients. Cancer 2005;104:36–43. [DOI] [PubMed] [Google Scholar]
- 4.Parekh DJ, Reis IM, Castle EP, et al. Robot-assisted radical cystectomy versus open radical cystectomy in patients with bladder cancer (RAZOR): an open-label, randomised, phase 3, non-inferiority trial. Lancet 2018;391:2525–2536. [DOI] [PubMed] [Google Scholar]
- 5.Hussein AA, May PR, Jing Z, et al. Outcomes of Intracorporeal Urinary Diversion after Robot-Assisted Radical Cystectomy: Results from the International Robotic Cystectomy Consortium. J Urol 2018;199:1302–1311.**Multi-institutional robotic cystectomy series demonstrating increasing utilization of intracorporeal technique for urinary diversion with decreasing major complications over time, reflecting the learning curve of intracorporeal techniques.
- 6.Zhang JH, Ericson KJ, Thomas LJ, et al. Large Single Institution Comparison of Perioperative Outcomes and Complications of Open Radical Cystectomy, Intracorporeal Robot-Assisted Radical Cystectomy and Robotic Extracorporeal Approach. J Urol 2019. doi: 10.1097/JU.0000000000000570. [DOI] [PubMed] [Google Scholar]
- 7.Parekh DJ, Reis IM, Castle EP, et al. Robot-assisted radical cystectomy versus open radical cystectomy in patients with bladder cancer (RAZOR): an open-label, randomised, phase 3, non-inferiority trial. Lancet (London, England) 2018;391:2525–2536. [DOI] [PubMed] [Google Scholar]
- 8.Satkunasivam R, Santomauro M, Chopra S, et al. Robotic Intracorporeal Orthotopic Neobladder: Urodynamic Outcomes, Urinary Function, and Health-related Quality of Life. Eur Urol 2016;69:247–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tyritzis SI, Hosseini A, Collins J, et al. Oncologic, functional, and complications outcomes of robot-assisted radical cystectomy with totally intracorporeal neobladder diversion. Eur Urol 2013;64:734–41. [DOI] [PubMed] [Google Scholar]
- 10.Shabsigh A, Korets R, Vora KC, et al. Defining Early Morbidity of Radical Cystectomy for Patients with Bladder Cancer Using a Standardized Reporting Methodology. Eur Urol 2009;55:164–176. [DOI] [PubMed] [Google Scholar]
- 11.Nieuwenhuijzen JA, de Vries RR, Bex A, et al. Urinary Diversions after Cystectomy: The Association of Clinical Factors, Complications and Functional Results of Four Different Diversions. Eur Urol 2008;53:834–844. [DOI] [PubMed] [Google Scholar]
- 12.MADERSBACHER S, SCHMIDT J, EBERLE JM, et al. Long-Term Outcome of Ileal Conduit Diversion. J Urol 2003;169:985–990.**This series defines the incidence and types of late (> 3 months after surgery) diversion-related complications observed in patients with at least 5-year follow-up following radical cystectomy.
- 13.Donahue TF, Bochner BH, Sfakianos JP, et al. Risk factors for the development of parastomal hernia after radical cystectomy. J Urol 2014;191:1708–1713.*Retrospective study describing the incidence and risk factors of radiographic parastomal hernia in patients underoing ileal conduit diversion
- 14.Liu NW, Hackney JT, Gellhaus PT, et al. Incidence and risk factors of parastomal hernia in patients undergoing radical cystectomy and ileal conduit diversion. J Urol 2014;191:1313–8. [DOI] [PubMed] [Google Scholar]
- 15.Movassaghi K, Shah SH, Cai J, et al. Incisional and Parastomal Hernia following Radical Cystectomy and Urinary Diversion: The University of Southern California Experience. J Urol 2016;196:777–81. [DOI] [PubMed] [Google Scholar]
- 16.Hussein AA, Ahmed YE, May P, et al. Natural History and Predictors of Parastomal Hernia after Robot-Assisted Radical Cystectomy and Ileal Conduit Urinary Diversion. J Urol 2018;199:766–773. [DOI] [PubMed] [Google Scholar]
- 17.Donahue TF, Cha EK, Bochner BH. Rationale and Early Experience with Prophylactic Placement of Mesh to Prevent Parastomal Hernia Formation after Ileal Conduit Urinary Diversion and Cystectomy for Bladder Cancer. Curr Urol Rep 2016;17:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Styrke J, Johansson M, Granåsen G, et al. Parastomal hernia after ileal conduit with a prophylactic mesh: a 10 year consecutive case series. Scand J Urol 2015;49:308–12. [DOI] [PubMed] [Google Scholar]
- 19.Kretschmer A, Grimm T, Buchner A, et al. Prognostic Features for Objectively Defined Urinary Continence after Radical Cystectomy and Ileal Orthotopic Neobladder in a Contemporary Cohort. J Urol 2017;197:210–215. [DOI] [PubMed] [Google Scholar]
- 20.Kretschmer A, Grimm T, Buchner A, et al. Midterm Health-related Quality of Life After Radical Cystectomy: A Propensity Score–matched Analysis. Eur Urol Focus 2019. doi: 10.1016/j.euf.2019.02.017. [DOI] [PubMed] [Google Scholar]
- 21.Singh V, Yadav R, Sinha RJ, et al. Prospective comparison of quality-of-life outcomes between ileal conduit urinary diversion and orthotopic neobladder reconstruction after radical cystectomy: a statistical model. BJU Int 2014;113:726–32. [DOI] [PubMed] [Google Scholar]
- 22.Philip J, Manikandan R, Venugopal S, et al. Orthotopic neobladder versus ileal conduit urinary diversion after cystectomy--a quality-of-life based comparison. Ann R Coll Surg Engl 2009;91:565–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anderson CB, Cookson MS, Chang SS, et al. Voiding function in women with orthotopic neobladder urinary diversion. J Urol 2012;188:200–204. [DOI] [PubMed] [Google Scholar]
- 24.Hedgepeth RC, Gilbert SM, He C, et al. Body image and bladder cancer specific quality of life in patients with ileal conduit and neobladder urinary diversions. Urology 2010;76:671–675. [DOI] [PubMed] [Google Scholar]
- 25.Ali AS, Hayes MC, Birch B, et al. Health related quality of life (HRQoL) after cystectomy: Comparison between orthotopic neobladder and ileal conduit diversion. Eur. J. Surg. Oncol. 2015;41:295–299. [DOI] [PubMed] [Google Scholar]
- 26.Anderson CB, Gennarelli R, Herr HW, et al. Regionalization of radical cystectomy in the United States. Urol Oncol Semin Orig Investig 2017;35:528.e7–528.e13. [DOI] [PubMed] [Google Scholar]
- 27.Bachman AG, Parker AA, Shaw MD, et al. Minimally Invasive Versus Open Approach for Cystectomy: Trends in the Utilization and Demographic or Clinical Predictors Using the National Cancer Database. Urology 2017;103:99–105. [DOI] [PubMed] [Google Scholar]
- 28.Bochner BH, Dalbagni G, Sjoberg DD, et al. Comparing open radical cystectomy and robot-assisted laparoscopic radical cystectomy: A randomized clinical trial. Eur Urol 2015;67:1042–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bochner BH, Dalbagni G, Marzouk KH, et al. Randomized Trial Comparing Open Radical Cystectomy and Robot-assisted Laparoscopic Radical Cystectomy: Oncologic Outcomes. Eur Urol 2018;74:465–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tyritzis SI, Hosseini A, Collins J, et al. Oncologic, functional, and complications outcomes of robot-assisted radical cystectomy with totally intracorporeal neobladder diversion. Eur Urol 2013;64:734–741. [DOI] [PubMed] [Google Scholar]
- 31.Satkunasivam R, Santomauro M, Chopra S, et al. Robotic Intracorporeal Orthotopic Neobladder: Urodynamic Outcomes, Urinary Function, and Health-related Quality of Life. Eur Urol 2016;69:247–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Check DK, Leo MC, Banegas MP, et al. Decision Regret Related to Urinary Diversion Choice among Patients with Cystectomy. J Urol 2019. doi: 10.1097/JU.0000000000000512.*Longitudinal cohort study identifying role of informed decision-making and quality of life in reducing risk of decision regret with urinary diversion choice.
- 33.Leo MC, Gilbert SM, Wendel CS, et al. Development of a goal elicitation measure to support choice about urinary diversion by patients with bladder cancer. J Urol 2019;202:83–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li Y, Rapkin B, Atkinson TM, et al. Leveraging Latent Dirichlet Allocation in processing free-text personal goals among patients undergoing bladder cancer surgery. Qual Life Res 2019;28:1441–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]