Abstract
The Chicago Classification v4.0 (CCv4.0) is the updated classification scheme for esophageal motility disorders using metrics from high-resolution manometry (HRM). A key feature of CCv.4.0 is the more rigorous and expansive protocol that incorporates single wet swallows acquired in different positions (supine, upright) and provocative testing, including multiple rapid swallows and rapid drink challenge. Additionally, solid bolus swallows, solid test meal, and/or pharmacologic provocation can be used to identify clinically relevant motility disorders and other conditions (eg, rumination) that occur during and after meals. The acquisition and analysis for performing these tests and the evidence supporting their inclusion in the Chicago Classification protocol is detailed in this technical review. Provocative tests are designed to increase the diagnostic sensitivity and specificity of HRM studies for disorders of esophageal motility. These changes attempt to minimize ambiguity in prior iterations of Chicago Classification, decrease the proportion of HRM studies that deliver inconclusive diagnoses and increase the number of patients with a clinically relevant diagnosis that can direct effective therapy. Another aim in establishing a standard manometry protocol for motility laboratories around the world is to facilitate procedural consistency, improve diagnostic reliability, and promote collaborative research.
1 |. INTRODUCTION
Patients who present with esophageal symptoms in whom mucosal and structural disorders have been excluded by endoscopy and who do not respond to empirical treatment are recommended to have esophageal physiology studies such as manometry and ambulatory reflux monitoring.1,2 Over 15 years, technological advances in data acquisition and presentation of physiological measurement have emerged, and these have been accompanied by changes in the classification of esophageal motility disorders.3–5 We are now in a better position now to visualize and understand esophageal function than at any time in the past. High-resolution manometry (HRM) technology and the Chicago Classification of esophageal motility disorders are well established in clinical practice; however, the methodology used to assess esophageal motility and function continues to develop. Novel methods designed to improve the diagnostic performance of HRM investigation have been developed and validated. Surveys suggest that many of these are already applied in neuro-gastroenterology motility laboratories.6 These “adjunctive” or “provocative” tests are now included in the Chicago Classification version 4.0© (CCv4.0) protocol.7
This technical review provides a detailed description of these techniques and the evidence that supports the use of “provocative” tests in clinical practice. The appropriate use of these methods can improve diagnostic accuracy and, in the context of the CCv4.0, help establish a conclusive diagnosis of esophageal motility disorder.8 The aim of this major revision is to provide more personalized medicine that can guide individual therapy decisions based upon patient presentation, investigation findings and preference.
2 |. METHODS
One working group led by two-chairs (MF, NR) and consisting of eight members was dedicated to development of a standard HRM protocol. As detailed in the main CCv4.0 document, each proposed statement underwent two rounds of independent ranking by the entire CCv4.0 development group according to the RAND UCLA Methodology to determine appropriateness of each statement (Table S1). Statements with a median score of 7 or higher and/or ≥80% agreement were adopted as CCv4.0 recommendations. The final protocol reflects this process and also discussions within and between working groups tasked with reviewing published evidence. This technical review reports the final recommendations for the CCv4.0 HRM protocol.
2.1 |. High-resolution manometry
A variety of modern HRM systems are commercially available, all of which incorporate a large number of sensors, ideally 1 per centimeter, on a flexible catheter which is passed from the nares, through the esophagus and into the stomach. Pressure data from these sensors are usefully presented as a compact, color-coded topographic plot of esophageal pressure activity, known as “Clouse plots”, in memory of Ray Clouse who adopted this technique in seminal publications.9,10 Water-perfused and solid-state HRM systems are available. The former is comprised of thin (micro-capillary) plastic tubes with tiny holes that open at various intervals along the length of the catheter. Changes in pressure within the esophagus alter resistance to the flow of water and this is converted into a signal by external transducers located at the perfusing pump. The latter acquires pressure information from miniaturized pressure sensors arranged along a catheter, with most modern solid-state catheters providing circumferential pressure data either from an array of radially arranged sensors around a central core or miniaturized “sleeve sensors”. The CCv4.0 working group recommends using a solid-state HRM catheter with less than 2 cm sensor spacing. However, recognizing that some labs will not have access to this assembly, the protocol and classification can be performed with water-perfused catheters if appropriate normative values are used. Additionally, a correction for hydrostatic effects is required if water-perfused manometry is applied in the upright position. High-resolution impedance manometry is recommended, though not required by CCv4.0, to assess not only pharyngeal function, but also intra-bolus pressure and bolus clearance through the EGJ. This combined technology is the subject of separate articles.11–13
All HRM systems provide a simultaneous and integrated assessment of pharyngeal, esophageal and lower esophageal sphincter function in real time. Although the information presented is similar, there are differences between technologies and systems produced by manufacturers that can influence pressure measurement. It is important that appropriate normative values should be applied that have been acquired using the same technology and methodology as applied in individual clinical studies.
2.2 |. Testing protocol
Prior to the procedure, patients should fast for at least 4 hours (sips of clear fluid allowed) and informed consent should be obtained. Following catheter placement, the patient assumes the supine or lateral position. A minimum of 60 seconds of quiet rest allows for an adaptation period, following which catheter position is confirmed using a minimum of three deep inspirations. Next, a baseline period of at least 30 seconds is captured to enable identification of anatomic landmarks including the upper esophageal sphincter (UES), lower esophageal sphincter (LES), respiratory inversion point (RIP), and basal EGJ pressure. Following any position change and an adaption period, this sequence of measurements can be repeated. The assessment of EGJ motility and function is the topic of a separate technical review. The primary measurements from esophageal HRM are acquired during a series of 5–10 ml single wet swallows. A key change in CCv4.0 is that these are taken in the supine and in the upright, seated position. Additionally, provocative tests are now recommended to increase diagnostic sensitivity and specificity of HRM studies. A summary of the standard protocol is provided for reference (Box 1, see also Graphical Summary).7
Key points.
The Chicago Classification version 4.0 (CCv4.0) of esophageal motility disorders for high-resolution manometry was agreed by an international development group using RAND UCLA Methodology.
The key advance of the CCv4.0 protocol is the inclusion of positional change and provocative testing in HRM studies
Appropriate normative values must be applied because there is variation in findings with position and with bolus consistency.
If no conclusive evidence of a motility disorder is identified in the primary position and/or if findings do not explain patient presentation, then swallows in the secondary position and /or with provocation tests should be performed.
Concordant findings in the secondary position and with provocation increase strength of confidence of the classification and diagnosis.
A solid test meal, post-prandial monitoring, or pharmacologic provocation can be considered if no conclusive diagnosis can be established by the CCv4 protocol, to resolve discordant findings or if the study fails to explain patient symptoms.
If no conclusive diagnosis can be established by the full CCv4 HRM, then additional investigations such as barium esophagogram or Endo-FLIP should be performed.
The assessment of esophageal motility in the supine position originated from the use of water-perfused catheter with 4 to 8 pressure sensors. These studies were performed with the patient lying flat to eliminate the influence of hydrostatic pressure and single wet swallows were acquired because the data was easy to interpret even when presented as multiple line plots. With the introduction of HRM, validation studies against the existing “conventional manometry” systems were performed using the existing protocol.14,15 Normative values from healthy individuals were published using the conventional methodology,16–18 and this became the foundation of the Chicago Classification versions 1.0–3.0.3–5 A HRM protocol based on single wet swallows is simple and quick to perform and analyze. Further, results can be interpreted across all systems, technologies and expertise with a reasonably high level of agreement.19,20 Thus, with publication of the Chicago Classification, physiologists and clinicians started to use the same terminology and methods, with rapid uptake of the technology in clinical and research practice.21 Notwithstanding these advantages, as experience with this technology increased, the limitations of the conventional protocol have become evident. HRM with single water swallows in the supine position lacks sensitivity and specificity for certain motility disorders and, thus, diagnoses based on these findings are often inconclusive. In many cases, this can be addressed by the introduction of “provocative” tests that assess esophageal motility not only in the supine position but also in the physiological, upright position. This is technically possible because developments in hard and software make it possible to acquire pressure measurements in the upright position without having to correct for hydrostatic pressure and the presentation of data in topographic Clouse plots facilitates the analysis of the more complex pressure activity that occurs during normal drinking and eating.22,23 Data acquisition in two positions and inclusion of provocative tests can prolong data acquisition and variation in findings between tests can complicate the interpretation of HRM findings. The CCv4.0 working group recognizes that increased time required for data acquisition and analysis could be a barrier to implementation; however, the full protocol can be completed within 15 minutes and the inclusion of this information increases diagnostic sensitivity and specificity for clinically relevant diagnosis of esophageal motility disorders.24–36 “Inconclusive” findings on wet swallows can often be confirmed by these tests and, conversely, discordant findings in the secondary position and/or with provocation should prompt reconsideration of the diagnosis. However, if a conclusive classification of findings is not possible based on HRM studies alone, then the use of corroborating supportive testing with timed barium esophogram (with tablet, barium-soaked bread or similar solid bolus marker) and/or functional lumen imaging probe may be required.37,38 Ultimately, outcome studies will identify the most informative protocol in different clinical scenarios.
2.3 |. Patient position
The full CCv4.0 HRM protocol is optimal, especially in research studies; however, clinicians can modify this protocol to adapt to available resources and time. Many labs commence the HRM protocol with a series of wet swallows (ie, 5–10 ml water or dilute normal saline if impedance is used) with the patient supine or in a lateral position. Others will commence clinical studies with the patient seated in a chair or on an examination couch. If the alternate position is not applied in all cases, then the limitations of an abbreviated protocol must be recognized, and appropriate normative values applied.
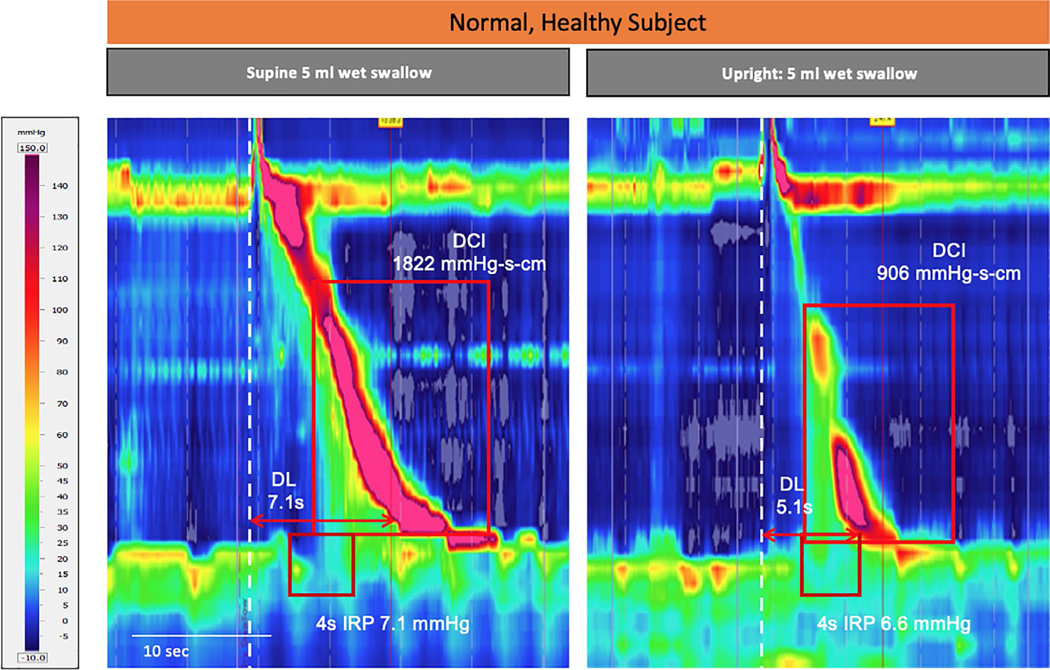
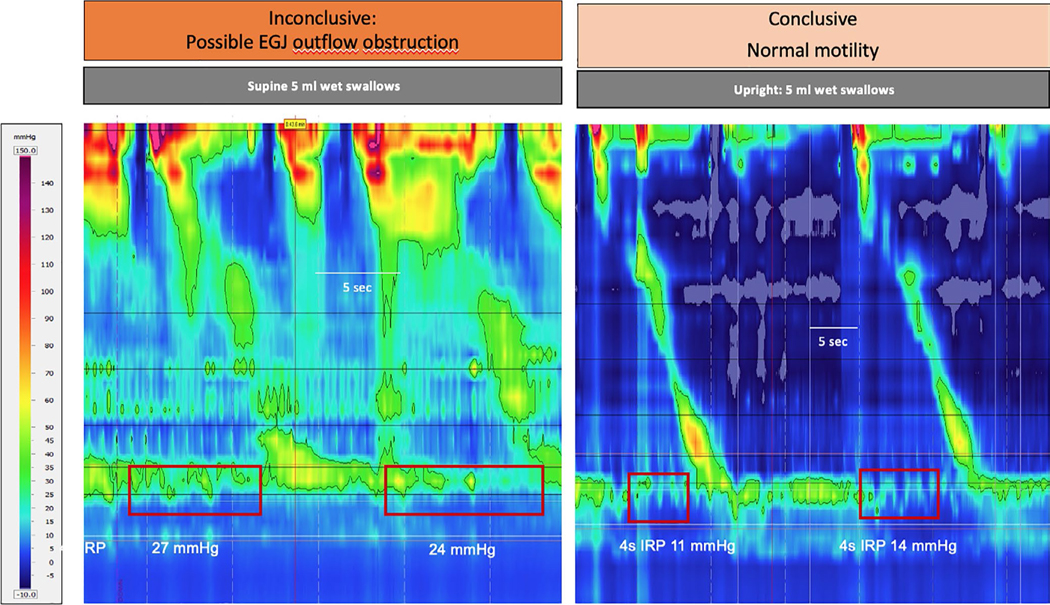
Compared to swallows in the supine position, esophageal contractions in the upright position have increased velocity and decreased vigor (distal contractile interval (DCI)) because gravity reduces the mechanical work required to transport the bolus through the esophagus (Figure 1).22,23 In a large prospective study of healthy subjects and patients with swallowing disorders studied in both positions, diagnostic agreement between positions was 67%, with reduced concordance primarily due to increased prevalence of ineffective esophageal motility (IEM) in the upright position. When IEM was excluded or position specific normal values were applied, concordance between upright and supine analysis improved to 90%.24 The most common reason for the residual lack of diagnostic agreement was esophago-gastric junction outflow obstruction (EGJOO), which is reported more frequently in the supine than the upright position (Figure 2). Recent studies indicate that the majority of EGJOO cases diagnosed in the supine position are false positive and do not persist when the patient moves to the upright position.24,25 Based on this evidence, the CCv4.0 recommends that swallows are acquired in both positions. In particular, abnormalities of esophageal motility seen in either position, especially when unexpected, should be re-evaluated with the patient shifted to the alternative position.
FIGURE 1.
Effect of position on esophageal motility in a healthy subject. The esophageal contraction tends to be slower, better coordinated and more vigorous in the supine (left panels) than the upright, seated (right panels) position. As a consequence, the proportion of ineffective, hypotensive contractions is often higher in the upright position. Appropriate normative values must be applied. Image Courtesy of Digestive Function: Basel at Klinik Arlesheim
FIGURE 2.
EGJ outflow obstruction with IRP >15 mm Hg is more frequently observed with wet swallows in the supine, than the upright position. Many such cases are artefactual, are not associated with increased intra-bolus pressure and are related to pressure on individual sensors as the catheter passes through the EGJ. If discordant findings are present, then provocative tests are helpful to identify individuals with clinically relevant disease. Image courtesy of Oesophageal Laboratory, University College London
2.3.1 |. CC4 recommendation
The CCv4.0 protocol can commence in either position (Table 1).
TABLE 1.
The CCv4© HRM Protocol can be commenced in the supine or the upright position. If the full protocol is not completed, then a shortened version combining selected HRM tests can be applied. The protocol working groups recommendations for required and optional tests for “supine first” and “upright first” studies are presented
| CCv4© HRM Protocol | Supine first study | Upright first study |
|---|---|---|
| Primary position 5–10 ml water ×10a | Required | Required |
| Alternate position 5–10 ml water ×5–10 | Required | Optional |
| Multiple Repeated Swallow ×1–3b | Required | Optional |
| Rapid Drink Challenge ×1 | Required | Required |
| Single Solid Swallow ×5–10c | Optional | Required |
| Solid Test Meal ± Post-prandial Observation | Optional | Optional |
If a conclusive diagnosis of achalasia type 1 or 2 is made from 10 wet swallows in primary position, then further maneuvers are not required.
The purpose of MRS is primarily to document peristaltic reserve. Three MRS are required only if an augmented MRS post-contraction is not present after 1 or 2 attempts.
If the purpose of solid swallows is to document peristaltic reserve (eg, in reflux patients), then the presence of an effective esophageal contraction in >2/10 swallows may be adequate. If it is to assess whether abnormal motility is the cause of patient symptoms then a minimum of 10 swallows is required.
Patients begin with 10 small volume wet swallows in the supine position. If a conclusive diagnosis is not made (eg, type I or II achalasia), then this is followed by at least 5 swallows in the upright position to exclude anomalies that are seen more frequently in the supine position (eg, false-positive diagnosis of EGJOO).
Patients begin with 10 small volume wet swallows in the upright position. If a conclusive diagnosis is not made, then this can be followed by at least 5 swallows in the supine position to exclude anomalies that are seen more frequently in the upright position (eg, false-positive diagnosis of IEM). This may not be required if normal, effective motility is observed in the upright position and during provocative tests (see below); however, this has not yet been confirmed in clinical studies.
The CCv4.0 working group acknowledges that the recommendation to acquire single wet swallows in both the supine and the upright positions plus the inclusion of “provocative” tests increases the time required to perform and analyze HRM studies. It is accepted that acquisition of wet swallows in both positions may not be necessary in routine clinical practice, especially if the findings in the initial position are expected (Table 1). However, if measurements are acquired only in one position, then position appropriate “normative values” are applied. What is essential is that the protocol acquires sufficient information to provide a conclusive diagnosis that explains patient symptoms (if relevant) and guides appropriate management for the individual patient.
2.4 |. Provocative tests
Swallowing small volumes of fluid in the supine or upright position does not represent normal behavior, and very rarely reproduces patients’ symptoms. As such, single wet swallows may lack sensitivity for clinically relevant disorders. To address this issue, “provocative” tests have been introduced, to demonstrate peristaltic reserve, induce abnormal motility and reveal the cause symptoms during the investigation. These include multiple rapid swallows (MRS), rapid drink challenge (RDC), ingestion of more viscous material (yogurt, apple sauce), single solid swallows (eg, bread, marshmallow, dumplings) or asking the patient to consume a test meal (their own food or a standardized pre-prepared meal). Except for MRS, these are normally performed with the patient in the upright position because it is difficult to drink and eat normally when lying flat. Viscous swallows are not discussed further because there is limited evidence that this improves test sensitivity of esophageal studies, especially if solid swallows are included in the protocol. Pharmacological provocation can also be performed during the HRM protocol to help support a diagnosis of a primary disorder of EGJ motility and function.39 This technique is detailed in supplementary information included with the main CCv4.0 publication and is the topic of recent papers.40,41
Inclusion of such techniques increases the time required to perform HRM and requires more expertise in interpreting the results. Provocative tests were referred to, but not included, in the previous iteration of the Chicago Classification because normative values were lacking and there was insufficient evidence supporting the clinical utility of this approach. A recent, international survey of 91 esophageal centers reported that 77% included rapid drink challenge, 63% included solids and 18% included a test meal in their routine clinical practice6; however, these were not applied in a consistent manner, non-standard methods were applied and there was no agreement as to the interpretation or reporting of findings.6 An important feature of the CC4.0 is the integration of provocative tests in the assessment of esophageal motility and function. Recommendations are made as to which tests should be included in routine clinical investigations and which can be reserved for specific patient groups. Standards have been agreed for the acquisition of provocative test and their analysis, interpretation and reporting.
2.5 |. Multiple rapid swallows (MRS)
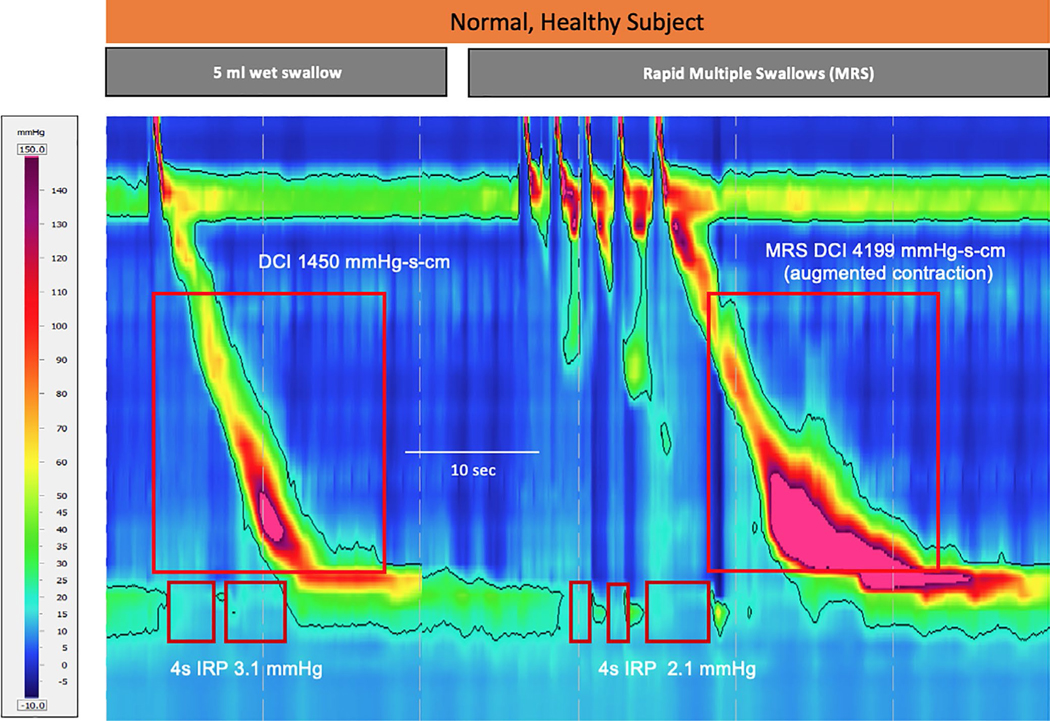
Swallowing normally leads to an almost instantaneous, “deglutitive” inhibition of the esophageal body and relaxation of the LES mediated by the release of nitric oxide from inhibitory neurons. In healthy subjects MRS enhances this phenomenon and, when completed, inhibition is often followed by a relatively high-pressure (augmented) ‘post-contraction’ to clear the esophagus of swallowed material (Figure 3). This sequence of events can provide useful information regarding the esophagus’s intrinsic neuromuscular function.42 MRS is generally performed in the supine position (studies in the upright position are lacking). Normative values have not been established in a large population of healthy subjects and further work is required also to confirm diagnostic thresholds in patients with motility disorders. Notwithstanding these issues, it has been shown that impaired deglutitive inhibition of the EGJ and esophageal body during MRS can help to identify achalasia and peristaltic disorders (eg, esophageal spasm, hypercontractile disorders), respectively.43 Additionally, the presence of an augmented post-contraction following MRS can be used as a marker of peristaltic reserve. This appears to be especially useful when IEM is diagnosed during single wet swallows.44 Augmentation is present if the distal contractile interval (DCI) is higher in the MRS post-contraction than the average DCI from a series of single water swallows performed in the same position (failed swallows not included in this analysis).35 The absence of an augmented contraction following MRS in esophageal studies performed is associated with increased likelihood of post-operative dysphagia in patients referred for consideration of anti-reflux surgery.34–36 The post-MRS contractile response is variable, and the working group recommends that the test is repeated up to three times to assess if peristaltic reserve is present if there is a failed or ineffective post-MRS contraction.35,45
FIGURE 3.
Multiple Rapid Swallows (MRS) is a physiological test that increases deglutitive inhibition of the esophageal contration and EGJ by asking the subject to swallow five times in quick succession. Subsequently, in healthy subjects, the MRS post-contraction is often augmented (more vigorous than normal). MRS highlights failure of deglutitive inhibition in patients with achalasia, esophageal spasm and hypercontractile disorders. Additionally, the lack of augmentation in the post-MRS contraction can indicate a lack of contractile reserve (ie, ability to respond to physiological or iatrogenic challenge). Image courtesy of Digestive Function: Basel at Klinik Arlesheim
2.5.1 |. CC4 recommendation
In CCv4.0, the multiple rapid swallow test has been standardized such that, through a syringe, the operator offers 2 ml aliquots of fluid in sequence, each separated by a few seconds, to produce a cumulative series of five swallows to make up to 10 ml.35,42,46 The CCv4.0 protocol includes this test in the supine position; however, it can be performed also in the upright position. An intact response to MRS is defined as absence of esophageal body contractility (DCI <100 mm Hg•s•cm) with complete deglutitive inhibition of the LES during the repetitive swallows, with an augmented post-MRS contraction. Augmentation is present if the DCI is in the normal range (ie, DCI >450 mm Hg.cm.s) and any of three post-contractions have increased contractile vigor compared to the mean DCI from non-failed single water swallows in the same position (ratio >1). The post-MRS contraction needs to be true peristaltic contractility and not artifact or pressurization.32,35,44,47
2.6 |. Rapid drink challenge (RDC)
The Rapid Drink Challenge (RDC) is designed to replicate normal drinking behavior in the upright position and is the provocative test most commonly used in clinical practice.6 Rapid intake of water by a series of swallows induces deglutitive inhibition of the esophageal body with complete EGJ relaxation and opening (Figure 4A). This is similar to MRS; however, the large volume of water ingested during RDC fills the esophagus and this can highlight resistance to flow, especially at the EGJ (Figure 4B). Clinical studies show that the addition of RDC increases the sensitivity of HRM for functional EGJOO (eg, subtype achalasia) and structural EGJOO (eg, stricture, tight fundoplication), diagnoses that can be missed during single water swallows.27,28,30,31,44 The test is easy to perform and results are highly reproducible. Standard metrics have been validated for the analysis of RDC during HRM studies and normal values for deglutitive inhibition and EGJ relaxation. EGJ function can be assessed using the standard 4 s integrated relaxation pressure (IRP) metric. RDC-IRP >12 mm Hg (with Medtronic equipment) accurately identifies achalasia, even in patients with normal IRP during single water swallows in whom functional obstruction is only evident during esophageal filling.30 RDC-IRP >8 mm Hg (with Medtronic equipment) increases test sensitivity and has good specificity for all causes of EGJOO.27 Inhibition of esophageal body contractility can be assessed qualitatively or quantitatively using the DCI tool during rapid drinking. Lack of deglutitive inhibition with peristaltic or simultaneous contractions (DCI >100 mm Hg•s•cm) during RDC is typical in esophageal spasm and hypercontractile motility. Abnormal post-RDC contractions are also seen in many patients with these diagnoses. Conversely, although the presence of a normal contraction sequence following the RDC is a specific marker of normal contractility; this is not present in all healthy controls.27,28,48
FIGURE 4.
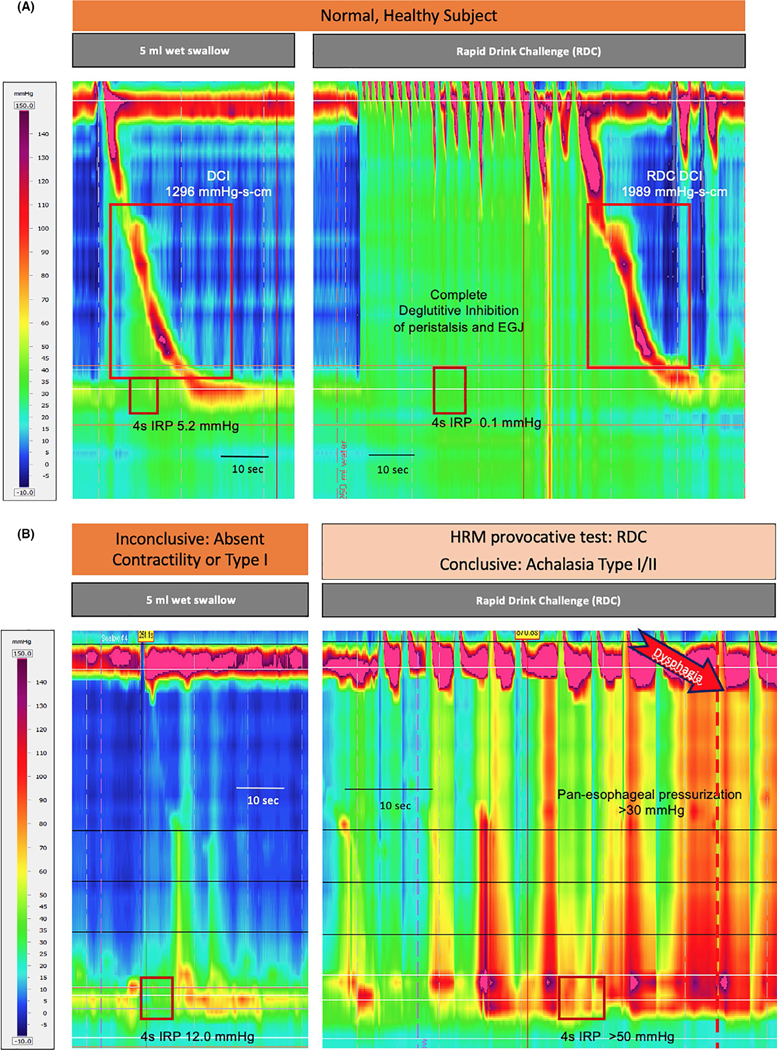
Rapid Drink Challenge (RDC) is performed by asking the subject to drink a large volume of water (100–200 ml) by a series of swallows. The rate can be controlled by drinking through a straw. In healthy subjects, similar to MRS, RDC highlights deglutitive inhibition during repeated swallows (upper panel). Additionally, the presence of a normal contraction sequence following the RDC is a specific marker of normal contractility; however, this is not observed in all healthy controls. Rapid Drink Challenge (RDC) highlights failure of deglutitive inhibition in patients with achalasia (lower panel). In this case the patient had inconclusive findings with normal IRP during wet swallows (left panel). RDC revealed conclusive evidence of achalasia with pan-esophageal pressurization and IRP >50 mm Hg. The patient responded to pneumatic dilatation. Images courtesy of Functional GI Laboratory, Zürich University Hospital.
Characteristic findings during RDC include a normal (“hypopressive”) pattern shared by healthy subjects and patients with IEM, that discriminates patients with non-obstructive hypercontractile motility or achalasia (sensitivity 80% and specificity 93%), (ii) impaired deglutitive inhibition (“brief hyperpressive” pattern) in patients with non-obstructive hypercontractile disorders (eg, distal spasm, hypercontractile esophagus), and (iii) impaired EGJ function (“prolonged hyperpressive” pattern) with increased RDC-IRP that discriminates achalasia and EGJOO from other patients groups (sensitivity 70% and specificity 85%).28 Additionally, the occurrence of typical symptoms during RDC in patients referred for investigation of dysphagia or other esophageal symptoms confirms the clinical relevance of any motility disorder identified during testing.29 Clinical studies have shown that RDC can help to establish a conclusive diagnosis in patients with borderline HRM findings during single water swallows.26–31 Furthermore, up to 17% of patients with esophageal symptoms but normal wet swallows have abnormal RDC findings that require further investigation by addition of solid swallows to the HRM protocol and /or other diagnostic tests.31
2.6.1 |. CC4 recommendation
CCv4.0 recommends that RDC is performed in the upright position to minimize the likelihood of aspiration, to reproduce normal drinking behavior and induce symptoms. The patient should drink a minimum 100 ml (ideally 200 ml) water by a series of rapid water swallows without stopping. The drink is often ingested through a straw to ensure that water is ingested at a steady rate. Deglutitive inhibition of esophageal body contractions (DCI) and EGJ function (IRP) are measured during the series of swallows. An intact response to RDC is defined as absence of esophageal body contractility (DCI <100 mm Hg•s•cm) with complete deglutitive inhibition of the LES during the RDC. When assessing response to RDC, IRP >12 mm Hg especially if accompanied by pan-esophageal pressurization >20–30 mm Hg (both with Medtronic software) are criteria for outflow obstruction.27,28,31,32,48 RDC is especially recommended as a provocative test in patients with suspected EGJ outflow obstruction and achalasia in whom IRP does not reach diagnostic thresholds with single water swallows.
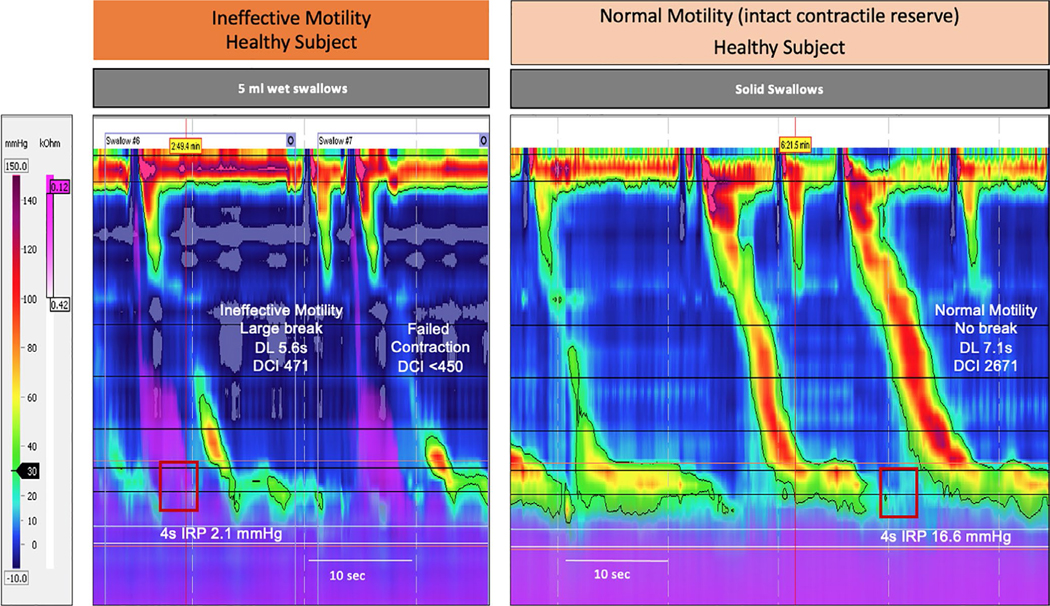
2.7 |. Single solid swallows
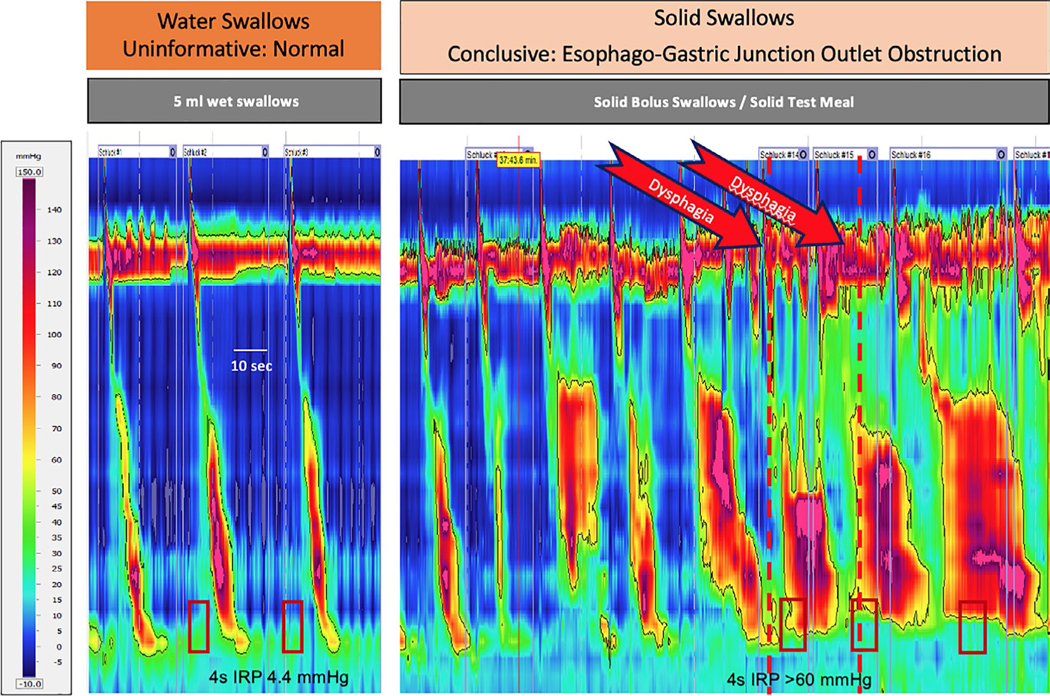
There has been interest for many years in including solid swallows in tests of esophageal function, such as ‘bread-barium’ imaging studies,38,49 to identify the causes of abnormal esophageal function and symptoms. Conventional manometry with line plot presentation of esophageal pressure activity may be more difficult to interpret for solid than liquid swallows.50 This is because more than one pharyngeal swallow are often required to ingest solids and multiple esophageal contractions may be required to transport the bolus through the esophagus and into the stomach. The introduction of HRM with continuous presentation of esophageal pressure data allow rapid acquisition and analysis of solid bolus swallows in clinical practice. Initial studies standardized the methodology and analysis. It was confirmed that healthy subjects and patients often take two pharyngeal contractions to swallow a single solid bolus; however, if taken within 4 seconds, this has no effect on subsequent esophageal contraction.51 Further, the esophageal response to solid bolus swallows is variable. In some healthy subjects only 1 in every 4–5 pharyngeal swallows is followed by an effective esophageal contraction.51 Studies demonstrated that IRP was higher for single solid compared to single wet swallows due to increased viscous resistance (Figure 5). The esophagus responds to this challenge with better coordinated (fewer large breaks in the contractile front), slower (increased DL) and more vigorous contractions (increased DCI).23,50–52 The established principles of the Chicago Classification are applied to establish a diagnosis. Normative values have been published for single solid swallows, and the measurements and diagnosis were found to be reproducible, with good intra-and inter-observer reproducibility.23,53,54
FIGURE 5.
Effect of bolus consistency on esophageal motility in a healthy subject. The esophageal contraction tends to be faster (shorter distal latency), less well coordinated (larger break in contractile front) and less vigorous (lower DCI) in wet swallows (left panel) than solid swallows (right panel). Additionally the IRP is increased for solid swallows due to higher viscous resistance to bolus passage through the EGJ. Appropriate normative values must be applied. Solid swallows can augment peristaltic motility in health and, as in the case presented, demonstrate contractile reserve in patients with ineffective motility during water swallows. Image courtesy of Oesophageal Laboratory, University College London.
Clinical studies indicate that inclusion of solid swallows in the HRM protocol increase the diagnostic yield for motility disorders, especially EGJOO, compared to single water swallows and the occurrence of symptoms during this provocative test supports the clinical relevance of HRM findings.14,24,26,31,33 Additionally, effective contractions after ingestion of solid bolus indicates the presence of peristaltic reserve in patients with IEM with single water swallows. The physiological and clinical relevance of this observation is illustrated by studies in gastro-esophageal reflux disease patients and patients with functional dysphagia. IEM is common in patients with all forms of GERD; however, effective contractions (ie, preserved peristaltic reserve) are present in significantly more patients with non-erosive disease than in those with reflux esophagitis or Barrett’s esophagus.55,56 In the same way, clinical studies have shown that patients with <20% effective contractions during a series of solid swallows have a high likelihood of reporting dysphagia.24,26,33
2.7.1 |. CC4 recommendation
HRM measurements during single solid swallows are acquired in a manner similar to single wet swallows. A series of solid bolus swallows, typically with 1–2 cm cube of buttered bread, soft biscuit, dumpling or cake, are taken into the mouth, chewed, and swallowed once the patient is ready. Single solid swallows may require two pharyngeal swallows; however, otherwise, at least 30 seconds should be allowed between swallows such that there is minimal interference between esophageal contractions. If included in the HRM protocol, then at least 5 solid swallows should be performed (10 swallows preferred). Standard metrics are used to analyze the HRM pressure measurements. Appropriate normative values must be applied. The diagnostic threshold for pathological EGJ function is IRP >25 mm Hg (using Medtronic software) and effective esophageal contractions are defined by the presence of peristalsis (DL >4.5 seconds) with no more than a small break in the contractile front (<3 cm) and vigorous contractility (DCI >1000 mm Hg.cm.s). At least 20% of single solid swallows should produce an effective contraction as defined above. Less than this defines the presence of IEM for solids and is associated with a high likelihood of dysphagia during the test.
2.8 |. Solid test meal
As for single water swallows, the use of single solid swallows to assess esophageal motility can be considered non-physiological. Moreover, this highly regulated and slow manner of eating may not provoke abnormal motility or cause esophageal symptoms. During a test meal pharyngeal swallows occur in rapid succession and are not always followed by effective esophageal contractions (Figure 6). HRM during normal eating produces complex pressure measurements that can be subject to over-interpretation. To address this and ensure that the method can be applied in routine clinical practice, efforts have been made to simplify and standardize the analysis using standard metrics that allow the findings to be classified using established Chicago Classification metrics.57 This method has been validated and shown to be reproducible. Normative values have been published and diagnostic thresholds for patients with motility disorders have been defined.51 Several clinical series have shown that inclusion of a standardized test meal that requires a minimum 20 pharyngeal swallows to ingest significantly increases diagnostic yield for major motility disorders and can increase the diagnostic yield for clinically relevant, major motility disorders and identify the cause of symptoms in the majority patients tested.26,33,58,59 The composition of the meal may not be critical with similar results reported for standardized meals (eg, soft boiled rice, bread) and for personally selected “culprit” foods.60
FIGURE 6.
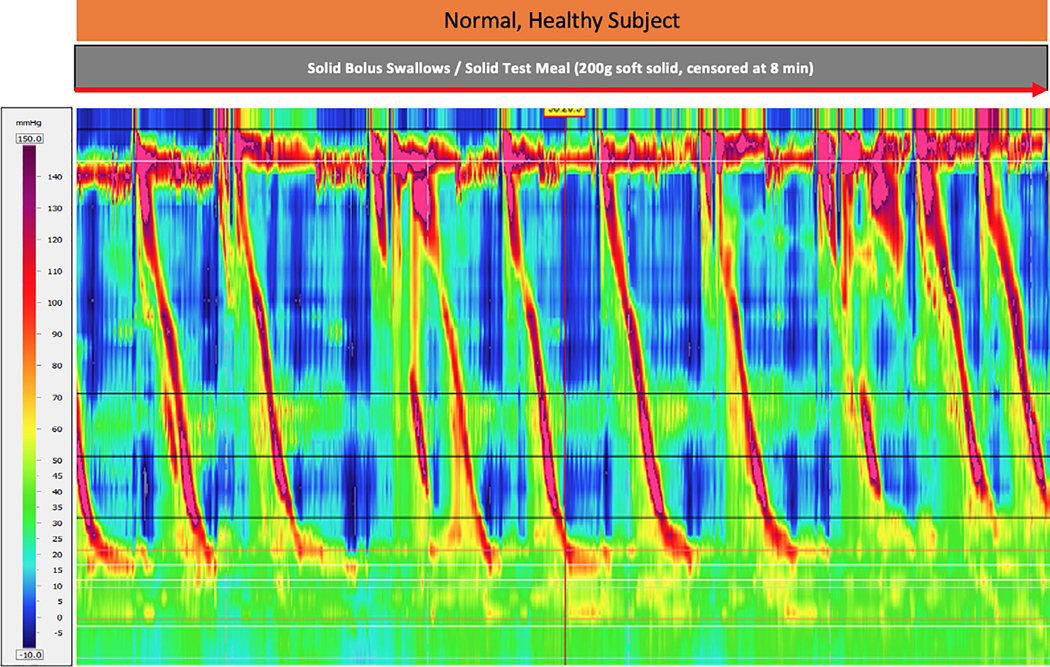
Representative excerpt from HRM recording of a solid test meal ingested by a normal, healthy subject. Image Courtesy of Digestive Function: Basel at Klinik Arlesheim
Case series and an increasing number of outcome studies show that this information produces clinically relevant results that can guide effective therapeutic decisions, especially in the diagnosis and management of EGJOO (Figure 7). Inclusion of a test meal in the HRM protocol identified abnormal motility in 70% of patients with dysphagia after anti-reflux surgery, compared to 30% with single water swallows.26 Approximately half the patients had EGJOO identified only during the solid meal and many of these had good outcomes following pneumatic dilatation of the EGJ/fundoplication wrap.26 In a recent case series, the sensitivity for clinically relevant, symptomatic EGJOO for HRM with a test meal was 85% compared to 54% for single water swallows and 54% for barium esophogram.31 Of 97 patients diagnosed with primary EGJOO, 29 received ‘achalasia-like therapy’ (eg, pneumatic dilatation) of whom 26 had a good clinical outcome, 8 had opioid induced esophageal dysmotility and were treated with opioid reduction or peripheral opioid antagonists, whereas 48 did not require therapy.31
FIGURE 7.
Water swallows (left panel) and start of solid test meal (right panel) in a patient with dysphagia for solids and normal endoscopy. The inclusion of solid swallows increases diagnostic sensitivity for motility disorders especially, as in this case, EGJ outflow obstruction. Additionally, the close temporal association of abnormal motility with symptoms supports the clinical relevance of the finding. Image Courtesy of Digestive Function: Basel at Klinik Arlesheim
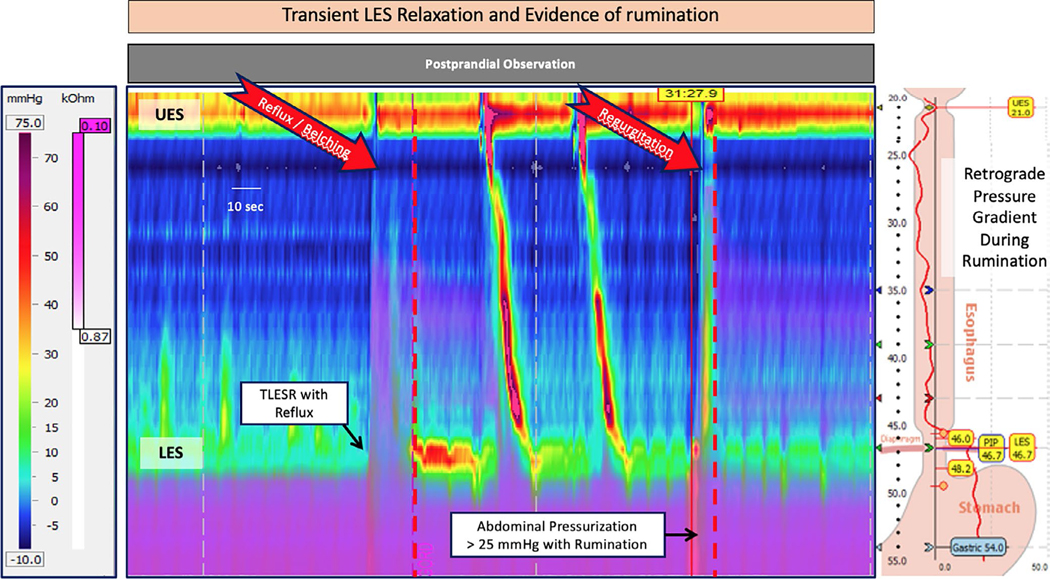
Further, testing can be extended into the post-prandial period to help induce, and classify functional disorders including volume reflux, rumination syndrome and supra-gastric belching (Figure 8).57,61–63 For this purpose combined HRM with impedance is optimal to document retrograde movement of intra-luminal contents (liquid or air); however, rapid increases in gastric pressure >25–30 mm Hg (“R waves” caused by voluntary, albeit unconscious, contraction of the abdominal musculature) associated with typical patient symptoms are characteristic of these behavioral disorders.62,63
FIGURE 8.
Post-prandial observation with combined high-resolution impedance manometry can identify the causes of symptoms that occur after meals. Transient LES relaxations (TLESRs) are often observed, however, a high frequency of these events after meals is consistent with the diagnosis of gastro-oesophageal reflux disease. In this case of a patient with volume regurgitation after meals, reflux and belching were associated with TLESRs; however, repetitive volume regurgitation was caused by rumination. This was confirmed by the presence of rapid increase in gastric pressure (>25 mm Hg) coincident with LES and UES relaxation and immediately followed by typical symptoms. Image courtesy of Digestive Function: Basel at Klinik Arlesheim
2.8.1 |. CC4 recommendation
The CCv4.0 does not require the inclusion of a test meal in routine clinical studies; however, this option should be considered in patients referred for investigation of esophageal symptoms if single water swallows and other provocative tests have either not identified a cause for patient symptoms or if the findings are inconclusive and /or do not guide management. It may also identify peristaltic reserve in patients with IEM on water swallows and confirm whether this finding is clinically relevant (ie, symptomatic or predictive of poor outcome after surgery). The protocol can be undertaken either with a standardized test meal or for the patient to bring in their own “culprit meal”. Ideally, the meal should require 20–30 pharyngeal swallows to complete. Symptoms should be recorded concurrently in the electronic record. The time allowed to complete a 200 g test meal is maximum 8 min. (median 6 min.) with failure to complete the meal within this time considered to be abnormal and “symptomatic”. Regardless of the solid meal used, the same metrics and diagnostic thresholds can be applied, with the findings classified using the CCv4.0 template. The recommended analysis of HRM findings during a test meal is simple. The number of pharyngeal swallows and effective esophageal contractions required to complete the meal is counted (defined as for single solid swallows). In normal, healthy subjects at least 20% of pharyngeal contractions are accompanied by an effective esophageal contraction. Abnormal EGJ function is present when ≥2 swallows have an IRP of >25 mm Hg (using the Medtronic system), spasm where ≥2 swallows have a distal latency of <4.5 seconds and hypercontractile esophagus when ≥2 esophageal contractions have DCI >8000 mm Hg.s.cm. The close temporal association of abnormal motility with typical symptoms supports the clinical relevance of the HRM findings, including IEM as defined by >80% ineffective swallows during the test meal.58
3 |. CONCLUSION
The key advance in this iteration of the CC4.0 protocol is the inclusion of positional change and provocative testing in HRM studies. These tests have been validated and both normative values and pathological thresholds have been established. Further, there is evidence that each can increase diagnostic sensitivity and/or specificity for esophageal motility disorders.
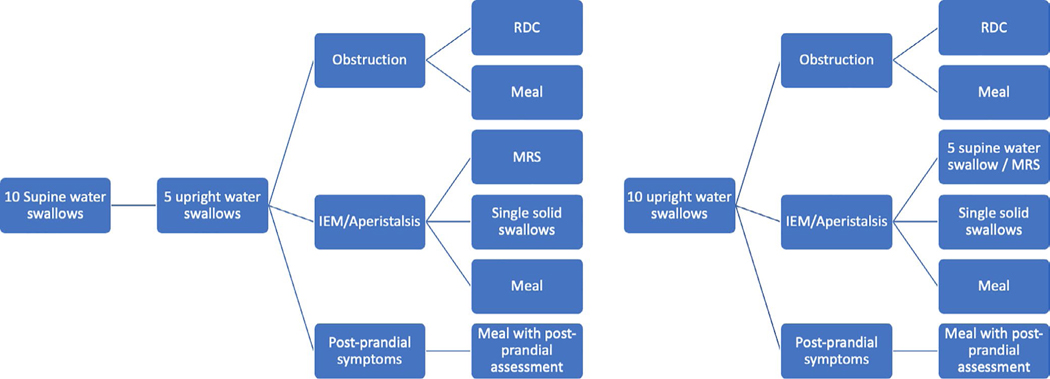
There is consensus that wet swallows still provide the basis for diagnosis by esophageal HRM. The CCv4.0 protocol recommends starting with a series of single wet swallows in either the supine or the upright position. If a conclusive diagnosis has not been established in the initial position (eg, achalasia), then this can be followed by a change in position and a sequence of provocative tests, including MRS, RDC and solid swallows. There was no final consensus regarding which of the provocative tests should be applied in a given clinical scenario; however, two alternate algorithms are provided for guidance (Table 1, Figure 9). Only a few studies have compared performance of different tests or assessed if including multiple tests provides more reliable information than any one test. Thus, decisions concerning when to apply provocative testing remain with the operator.
FIGURE 9.
Two alternate algorithms to guide the use of provocative tests during the CCv4.0 Protocol are provided. Left panel: Protocol commencing with wet swallows in the supine position. Right panel: Protocol commencing with wet swallows in the upright position. In both provocative tests that increase the sensitivity and specificity for detection of clinically relevant esophageal motility disorders are recommended.
It is hoped that this review will provide physiologists and clinicians with the information that they require to decide which individual or combination of tests fits best into their practice. Standard operating procedures for the acquisition and analysis of provocative tests are provided to ensure that clinical investigations and research studies are performed to a high standard and the results can be compared between different centers.
Looking ahead, outcome studies are required to confirm the contribution of each part of the CCv4.0 protocol. It may well be that future iterations reveal redundancy and that certain components (eg, wet swallows in one or other position, MRS) can be removed from the protocol without loss of clinically relevant information. Until then it is hoped that the CCv4.0 protocol and classification will provide patients and doctors with a conclusive diagnosis that identifies the underlying physio-mechanical mechanism of disease and guides specific and effective therapy.
Supplementary Material
BOX 1. High Resolution Esophageal Manometry Standard Protocol: Chicago Classification version 4.0©.
PRE-PROCEDURE
Prior to procedure patients should fast for at least 4 hours and informed consent should be obtained
The CC4.0 Working Group recommends using a solid state high-resolution manometry catheter with <2 cm sensor spacing with combined impedance sensors. However, the protocol and classification can be performed with water perfused catheters if appropriate normative values are used.
STUDY PROCEDURE
Study begins in supine position [use supine normative values]
≥60 seconds adaptation period
Document position with at least 3 deep inspirations
≥30 seconds baseline period
10 supine wet (5 ml) swallows
1 multiple rapid swallow sequence (multiple rapid sequence may be repeated up to 3 sequences if failed attempt or abnormal response)
Change position to upright [use upright normative values]
≥60 seconds adaptation period
Document position with at least 3 deep inspirations
>30 seconds baseline period
≥5 upright wet (5 ml) swallows
1 rapid drink challenge
If no clinically relevant motility disorder is found consider the following manometric tests
In a patient with high probability of a missed diagnosis, especially EGJ outflow obstruction: Solid test swallows, solid test meal, and/or pharmacologic provocation (ie, amyl nitrite, cholecystokinin) in the upright position to assess for obstruction
For suspected rumination/belching disorder: Post-prandial high-resolution impedance observation
If equivocal results are found and/or there is suspicion for an EGJ outflow obstruction that does not fulfill criteria for achalasia, consider the following supportive tests
Timed barium esophagram, preferably with tablet
Endoluminal functional lumen imaging planimetry (FLIP)
Although the protocol designed by the CC4.0 team is considered to be the optimal protocol, clinicians can modify this protocol based on limited resources and time as long as normative values are applied and other positions and provocative tests are used appropriately. Physicians choosing to begin the study in the upright position should perform 10 upright swallows.
REPORTING:
In addition to CC 3.0 metrics, final report should include baseline measures of the esophagogastric junction (EGJ) and symptoms experienced during the study and within 15 seconds of a motility dysfunction.
Acknowledgments
Mark R. Fox: Speaker and support for educational and research activities: Medtronic, Laborie, Diversatek. Research support: Reckitt Benckiser, Nestlé International. Rami Sweis: Speaker: Medtronic, Covidian, Given, Falk Pharma, Ethicon; Advisory Board: Falk Pharma, Ethicon. Rena Yadlapati: Consultant through Institutional Agreement: Medtronic, Ironwood Pharmaceuticals, Diversatek; Research support: Ironwood Pharmaceuticals; Advisory Board: Phathom Pharmaceuticals; Stock Options: RJS Mediagnostix. John E. Pandolfino: Consultant: Medtronic, Ironwood Pharmaceuticals, Diversatek; Research support: Ironwood Pharmaceuticals, Takeda; Advisory Board: Medtronic, Diversatek; Stock Options: Crospon Inc. Jan Tack: Research Grant: Sofar Pharmaceuticals.
Abbreviations:
- CCv4.0
Chicago classification version 4.0©
- DCI
distal contractile interval (DCI)
- DL
distal latency
- EGJ
esophago-gastric junction
- EGJOO
esophago-gastric junction outflow obstruction
- HRM
high-resolution manometry
- IEM
ineffective esophageal motility
- IRP
integrated relaxation pressure
- MRS
multiple rapid swallows
- RDC
rapid drink challenge
- RIP
respiratory inversion point
- STM
solid test meal
- UES
upper esophageal sphincter
Footnotes
CONFLICT OF INTEREST
Other authors have none to report.
SUPPORTING INFORMATION
Additional supporting information may be found online in the Supporting Information section.
REFERENCES
- 1.Fox MR, Kahrilas PJ, Roman S, et al. Clinical measurement of gastrointestinal motility and function: who, when and which test? Nat Rev Gastroenterol Hepatol. 2018;15:568–579. [DOI] [PubMed] [Google Scholar]
- 2.Trudgill NJ, Sifrim D, Sweis R, et al. British society of gastroenterology guidelines for oesophageal manometry and oesophageal reflux monitoring. Gut. 2019;68:1731–1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24(Suppl 1):57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pandolfino JE, Fox MR, Bredenoord AJ, et al. High-resolution manometry in clinical practice: utilizing pressure topography to classify oesophageal motility abnormalities. Neurogastroenterol Motil. 2009;21:796–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sweis R, Heinrich H, Fox M, et al. Variation in esophageal physiology testing in clinical practice: results from an international survey. Neurogastroenterol Motil. 2018;30:e13215. [DOI] [PubMed] [Google Scholar]
- 7.Yadlapati R, Pandolfino JE, Fox MR, et al. What is new in Chicago Classification version 4.0? Neurogastroenterol Motil. 2021;33:e14053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yadlapati R, Kahrilas PJ, Fox MR, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0((c)). Neurogastroenterol Motil. 2021;33:e14058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clouse RE, Staiano A, Alrakawi A. Development of a topographic analysis system for manometric studies in the gastrointestinal tract. Gastrointest Endosc. 1998;48:395–401. [DOI] [PubMed] [Google Scholar]
- 10.Clouse RE, Staiano A, Alrakawi A, et al. Application of topographical methods to clinical esophageal manometry. Am J Gastroenterol. 2000;95:2720–2730. [DOI] [PubMed] [Google Scholar]
- 11.Omari TI, Ciucci M, Gozdzikowska K, et al. High-resolution pharyngeal manometry and impedance: protocols and metrics-recommendations of a high-resolution pharyngeal manometry international working group. Dysphagia. 2020;35:281–295. [DOI] [PubMed] [Google Scholar]
- 12.Singendonk MJ, Lin Z, Scheerens C, et al. High-resolution impedance manometry parameters in the evaluation of esophageal function of non-obstructive dysphagia patients. Neurogastroenterol Motil. 2019;31:e13505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carlson DA, Omari T, Lin Z, et al. High-resolution impedance manometry parameters enhance the esophageal motility evaluation in non-obstructive dysphagia patients without a major Chicago Classification motility disorder. Neurogastroenterol Motil. 2017;29:e12941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fox M, Hebbard G, Janiak P, et al. High-resolution manometry predicts the success of oesophageal bolus transport and identifies clinically important abnormalities not detected by conventional manometry. Neurogastroenterol Motil. 2004;16:533–542. [DOI] [PubMed] [Google Scholar]
- 15.Clouse RE, Parks T, Haroian LR, et al. Development and clinical validation of a solid-state high-resolution pressure measurement system for simplified and consistent esophageal manometry. Am J Gastroenterol. 2003;98:S32–S33. [Google Scholar]
- 16.Pandolfino JE, Ghosh SK, Zhang Q, et al. Quantifying EGJ morphology and relaxation with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol Gastrointest Liver Physiol. 2006;290:G1033–G1040. [DOI] [PubMed] [Google Scholar]
- 17.Ghosh SK, Pandolfino JE, Zhang Q, et al. Deglutitive upper esophageal sphincter relaxation: a study of 75 volunteer subjects using solid-state high-resolution manometry. Am J Physiol Gastrointest Liver Physiol. 2006;291:G525–G531. [DOI] [PubMed] [Google Scholar]
- 18.Ghosh SK, Pandolfino JE, Zhang Q, et al. Quantifying esophageal peristalsis with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol Gastrointest Liver Physiol. 2006;290:G988–G997. [DOI] [PubMed] [Google Scholar]
- 19.Grubel C, Hiscock R, Hebbard G. Value of spatiotemporal representation of manometric data. Clin Gastroenterol Hepatol. 2008;6:525–530. [DOI] [PubMed] [Google Scholar]
- 20.Soudagar AS, Sayuk GS, Gyawali CP. Learners favour high resolution oesophageal manometry with better diagnostic accuracy over conventional line tracings. Gut. 2012;61:798–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fox MR, Bredenoord AJ. Oesophageal high-resolution manometry: moving from research into clinical practice. Gut. 2008;57:405–423. [DOI] [PubMed] [Google Scholar]
- 22.Roman S, Damon H, Pellissier PE, et al. Does body position modify the results of oesophageal high resolution manometry? Neurogastroenterol Motil. 2010;22:271–275. [DOI] [PubMed] [Google Scholar]
- 23.Sweis R, Anggiansah A, Wong T, et al. Normative values and inter-observer agreement for liquid and solid bolus swallows in upright and supine positions as assessed by esophageal high-resolution manometry. Neurogastroenterol Motil. 2011;23:509–e198. [DOI] [PubMed] [Google Scholar]
- 24.Misselwitz B, Hollenstein M, Butikofer S, et al. Prospective serial diagnostic study: the effects of position and provocative tests on the diagnosis of oesophageal motility disorders by high-resolution manometry. Aliment Pharmacol Ther. 2020;51:706–718. [DOI] [PubMed] [Google Scholar]
- 25.Triggs JR, Carlson DA, Beveridge C, et al. Upright integrated relaxation pressure facilitates characterization of esophagogastric junction outflow obstruction. Clin Gastroenterol Hepatol. 2019;17:2218–2226.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang YT, Tai LF, Yazaki E, et al. Investigation of dysphagia after antireflux surgery by high-resolution manometry: impact of multiple water swallows and a solid test meal on diagnosis, management, and clinical outcome. Clin Gastroenterol Hepatol. 2015;13:1575–1583. [DOI] [PubMed] [Google Scholar]
- 27.Ang D, Hollenstein M, Misselwitz B, et al. Rapid drink challenge in high-resolution manometry: an adjunctive test for detection of esophageal motility disorders. Neurogastroenterol Motil. 2017;29:e12902. [DOI] [PubMed] [Google Scholar]
- 28.Marin I, Serra J. Patterns of esophageal pressure responses to a rapid drink challenge test in patients with esophageal motility disorders. Neurogastroenterol Motil. 2016;28:543–553. [DOI] [PubMed] [Google Scholar]
- 29.Zerbib F, Luna D, Marin I, et al. The added value of symptom analysis during a rapid drink challenge in high-resolution esophageal manometry. Neurogastroenterol Motil. 2020;e14008. [DOI] [PubMed] [Google Scholar]
- 30.Sanagapalli S, Roman S, Hastier A, et al. Achalasia diagnosed despite normal integrated relaxation pressure responds favorably to therapy. Neurogastroenterol Motil. 2019;31:e13586. [DOI] [PubMed] [Google Scholar]
- 31.Sanagapalli S, McGuire J, Leong RW, et al. The clinical relevance of manometric esophagogastric junction outflow obstruction can be determined using rapid drink challenge and solid swallows. Am J Gastroenterol. 2020;116(2):280–288. [DOI] [PubMed] [Google Scholar]
- 32.Krause AJ, Su H, Triggs JR, et al. Multiple rapid swallows and rapid drink challenge in patients with esophagogastric junction outflow obstruction on high-resolution manometry. Neurogastroenterol Motil. 2021;33(3):e14000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ang D, Misselwitz B, Hollenstein M, et al. Diagnostic yield of high-resolution manometry with a solid test meal for clinically relevant, symptomatic oesophageal motility disorders: serial diagnostic study. Lancet Gastroenterol Hepatol. 2017;2:654–661. [DOI] [PubMed] [Google Scholar]
- 34.Stoikes N, Drapekin J, Kushnir V, et al. The value of multiple rapid swallows during preoperative esophageal manometry before laparoscopic antireflux surgery. Surg Endosc. 2012;26:3401–3407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shaker A, Stoikes N, Drapekin J, et al. Multiple rapid swallow responses during esophageal high-resolution manometry reflect esophageal body peristaltic reserve. Am J Gastroenterol. 2013;108:1706–1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hasak S, Brunt LM, Wang D, et al. Clinical characteristics and outcomes of patients with postfundoplication dysphagia. Clin Gastroenterol Hepatol. 2019;17:1982–1990. [DOI] [PubMed] [Google Scholar]
- 37.Kahrilas PJ, Bredenoord AJ, Fox M, et al. Expert consensus document: advances in the management of oesophageal motility disorders in the era of high-resolution manometry: a focus on achalasia syndromes. Nat Rev Gastroenterol Hepatol. 2017;14:677–688. [DOI] [PubMed] [Google Scholar]
- 38.Blonski W, Kumar A, Feldman J, et al. Timed barium swallow: diagnostic role and predictive value in untreated achalasia, esophago-gastric junction outflow obstruction, and non-achalasia dysphagia. Am J Gastroenterol. 2018;113:196–203. [DOI] [PubMed] [Google Scholar]
- 39.Babaei A, Shad S, Szabo A, et al. Pharmacologic interrogation of patients with esophagogastric junction outflow obstruction using amyl nitrite. Neurogastroenterol Motil. 2019;31:e13668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Babaei A, Shad S, Massey BT. Diagnostic differences in the pharmacologic response to cholecystokinin and amyl nitrite in patients with absent contractility vs type I achalasia. Neurogastroenterol Motil. 2020;32:e13857. [DOI] [PubMed] [Google Scholar]
- 41.Babaei A, Shad S, Massey BT. Motility patterns following esophageal pharmacologic provocation with amyl nitrite or cholecystokinin during high-resolution manometry distinguish idiopathic vs opioid-induced type 3 achalasia. Clin Gastroenterol Hepatol. 2020;18:813–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fornari F, Bravi I, Penagini R, et al. Multiple rapid swallowing: a complementary test during standard oesophageal manometry. Neurogastroenterol Motil. 2009;21:718–e41. [DOI] [PubMed] [Google Scholar]
- 43.Kushnir V, Sayuk GS, Gyawali CP. Multiple rapid swallow responses segregate achalasia subtypes on high-resolution manometry. Neurogastroenterol Motil. 2012;24:1069–e561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Elvevi A, Mauro A, Pugliese D, et al. Usefulness of low- and high-volume multiple rapid swallowing during high-resolution manometry. Dig Liver Dis. 2015;47:103–107. [DOI] [PubMed] [Google Scholar]
- 45.Mauro A, Savarino E, De Bortoli N, et al. Optimal number of multiple rapid swallows needed during high-resolution esophageal manometry for accurate prediction of contraction reserve. Neurogastroenterol Motil. 2018;30:e13253. [DOI] [PubMed] [Google Scholar]
- 46.Price LH, Li Y, Patel A, et al. Reproducibility patterns of multiple rapid swallows during high resolution esophageal manometry provide insights into esophageal pathophysiology. Neurogastroenterol Motil. 2014;26:646–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Martinucci I, Savarino EV, Pandolfino JE, et al. Vigor of peristalsis during multiple rapid swallows is inversely correlated with acid exposure time in patients with NERD. Neurogastroenterol Motil. 2016;28:243–250. [DOI] [PubMed] [Google Scholar]
- 48.Woodland P, Gabieta-Sonmez S, Arguero J, et al. 200 ml rapid drink challenge during high-resolution manometry best predicts objective esophagogastric junction obstruction and correlates with symptom severity. J Neurogastroenterol Motil. 2018;24:410–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Davies HA, Evans KT, Butler F, et al. Diagnostic value of “bread-barium” swallow in patients with esophageal symptoms. Dig Dis Sci. 1983;28:1094–1100. [DOI] [PubMed] [Google Scholar]
- 50.Johnston BT, Collins JS, McFarland RJ, et al. A comparison of esophageal motility in response to bread swallows and water swallows. Am J Gastroenterol. 1993;88:351–355. [PubMed] [Google Scholar]
- 51.Hollenstein M, Thwaites DT, Buetikofer S, et al. Pharyngeal swallowing and oesophageal motility during a solid meal test: a prospective study in healthy volunteers and patients with major motility disorders. Lancet Gastroenterol Hepatol. 2017;2:644–653. [DOI] [PubMed] [Google Scholar]
- 52.Hasan Y, Go J, Hashmi SM, et al. Influence of everyday bolus consistencies in different body positions on high-resolution esophageal pressure topography (HREPT) parameters. Dis Esophagus. 2015;28:246–252. [DOI] [PubMed] [Google Scholar]
- 53.Xiao Y, Kahrilas PJ, Nicodeme F, et al. Lack of correlation between HRM metrics and symptoms during the manometric protocol. Am J Gastroenterol. 2014;109:521–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xiao Y, Nicodeme F, Kahrilas PJ, et al. Optimizing the swallow protocol of clinical high-resolution esophageal manometry studies. Neurogastroenterol Motil. 2012;24:e489–e496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Daum C, Sweis R, Kaufman E, et al. Failure to respond to physiologic challenge characterizes esophageal motility in erosive gastro-esophageal reflux disease. Neurogastroenterol Motil. 2011;23:517–e200. [DOI] [PubMed] [Google Scholar]
- 56.Sanagapalli S, Emmanuel A, Leong R, et al. Impaired motility in Barrett’s esophagus: a study using high-resolution manometry with physiologic challenge. Neurogastroenterol Motil. 2018;30(8):e13330. [DOI] [PubMed] [Google Scholar]
- 57.Sweis R, Anggiansah A, Wong T, et al. Assessment of esophageal dysfunction and symptoms during and after a standardized test meal: development and clinical validation of a new methodology utilizing high-resolution manometry. Neurogastroenterol Motil. 2014;26:215–228. [DOI] [PubMed] [Google Scholar]
- 58.Hollenstein M, Thwaites P, Butikofer S, et al. Pharyngeal swallowing and oesophageal motility during a solid meal test: a prospective study in healthy volunteers and patients with major motility disorders. Lancet Gastroenterol Hepatol. 2017;2:644–653. [DOI] [PubMed] [Google Scholar]
- 59.Araujo IK, Roman S, Napoleon M, et al. Diagnostic yield of adding solid food swallows during high-resolution manometry in esophageal motility disorders. Neurogastroenterol Motil. 2020:e14060. [DOI] [PubMed] [Google Scholar]
- 60.Sykes C, Davidson A, Blake JA, et al. Dysphagia: has standardising our test meal increased our diagnostic yield during high resolution oesophageal manometry? United European Gastroenterol J. 2020;8:144–887. [Google Scholar]
- 61.Pauwels A, Broers C, Van Houtte B, et al. A randomized double-blind, placebo-controlled, cross-over study using baclofen in the treatment of rumination syndrome. Am J Gastroenterol. 2018;113:97–104. [DOI] [PubMed] [Google Scholar]
- 62.Tucker E, Knowles K, Wright J, et al. Rumination variations: aetiology and classification of abnormal behavioural responses to digestive symptoms based on high-resolution manometry studies. Aliment Pharmacol Ther. 2013;37:263–274. [DOI] [PubMed] [Google Scholar]
- 63.Kessing BF, Bredenoord AJ, Smout AJ. Objective manometric criteria for the rumination syndrome. Am J Gastroenterol. 2014;109:52–59. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.