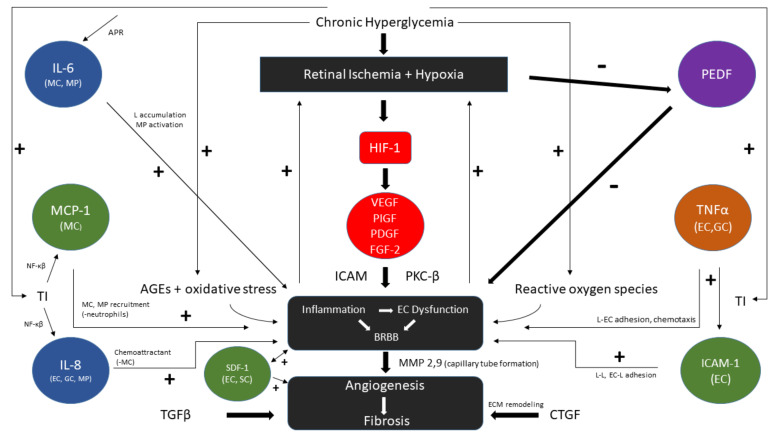
Figure 3.
Flow diagram of VEGF dependent and major independent patho-mechanisms in proliferative diabetic retinopathy. Chronic hyperglycemia leads to tissue injury (TI), hypoxia, advanced glycated end products (AGEs), and reactive oxygen species that cause inflammation and endothelial dysfunction with blood–retinal barrier breakdown (BRBB) in a positive feedback loop. VEGF is produced directly by HIF-1 stimulation in hypoxic conditions and directs its action through PKC-β and stimulates ICAM. PEDF and its inhibitory effects on BRBB are suppressed by hypoxia. VEGF independent pathways include IL-6, by acute phase response (APR) with induction of leukocyte (L) accumulation. TI further stimulates MCP-1 and IL-8 through NF-κβ as chemoattractants. TNFα secreted by endothelial cells (EC) and glial cells (GC) and ICAM-1 promote EC and L adhesion to further cause loss of microvascular integrity. TNF-α stimulates MCP-1 (not shown). SDF-1, derived from EC and stromal cells (SC) (bone marrow), is generated in response to endothelial injury and recruits progenitor cells, weakens tight junctions, and may promote neovascularization. Continued microangiopathy results in angiogenesis and culminates in fibrotic extracellular matrix (ECM) remodeling (through TGFβ, CTGF) whose footprint is largely irreversible. The above concepts have been discussed throughout the ongoing PDR vitreous scientific literature [21,35,40,42,64,81,94,99,112,120,123,134,154,163,164,165].