Fig. 3.
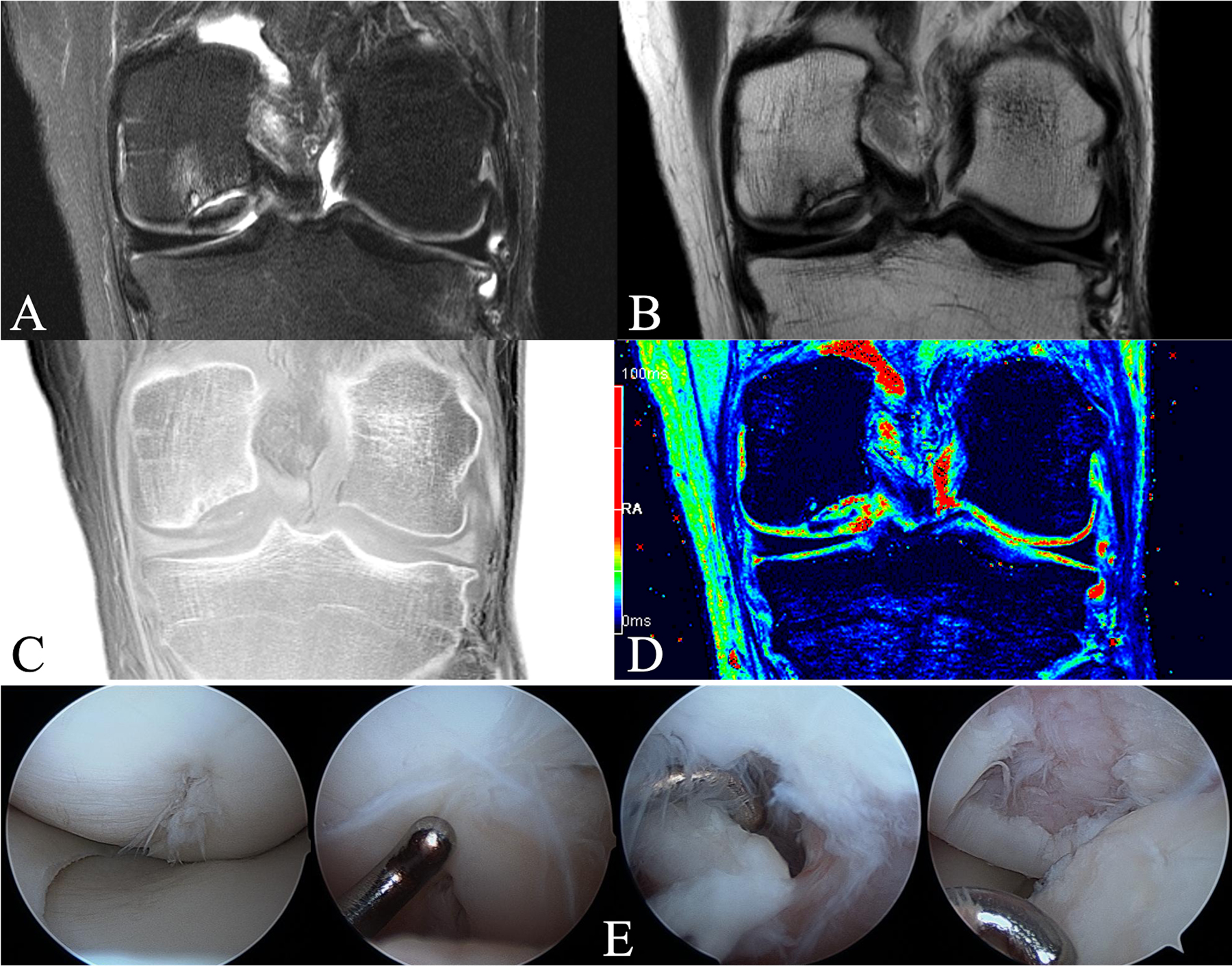
Figs. 3-A through 3-E A 23-year-old man with an OCD lesion on the central aspect of the medial femoral condyle evaluated with an advanced clinical 3-T MRI protocol and arthroscopy. Fig. 3-A T2-weighted fat-saturated coronal TSE (turbo-spin-echo) image (TR [repetition time] = 3,600 ms, and TE [echo time] = 59 ms) demonstrating cystic changes and marrow edema of the parent bone. Substantial fluid at the parent-progeny interface is indicative of an unstable lesion. Overlying articular cartilage appears grossly intact. Fig. 3-B Proton density-weighted coronal TSE image (TR = 3,400 ms, and TE = 27 ms), demonstrating a dark progeny fragment suggesting osseous tissue. Fig. 3-C CT-like GRE (gradient-recalled echo) image (TR = 1,000 ms, and TE = 3.15 ms) with inverted contrast (“bone window”), demonstrating parent bone with cystic changes, sclerosis, and marginal mineralization and/or ossification surrounding the cartilaginous progeny lesion. Fig. 3-D T2* map (TR = 1,000 ms and TE = 3.15, 7.5, 11.9, 22.2, and 34.5 ms). Color-coding signal intensities: blue to black = bone and mineralization, green to red = epiphyseal and articular cartilage, and red = fluid at the parent-progeny lesion interface. T2* mapping affirms a cartilaginous OCD lesion (green centrally) with marginal ossification (blue), deemed unstable because of fluid (red) at the interface. Of note is mild overlying articular cartilage edema (red). Fig. 3-E Arthroscopic photographs confirming an unstable lesion. Arthroscopy was unable to determine the presence of bone on the fragment; thus, the advanced clinical 3-T MRI protocol helped to guide intraoperative decision-making. The patient underwent screw fixation, went on to heal, and returned to all activities.
