Abstract
Background:
Despite the benefits of early intervention services for the initial stages of psychosis ongoing impairments in functioning are common.
Aims:
To identify 1-year trajectories of occupational and social functioning in individuals enrolled in OnTrackNY, a statewide program offering early intervention services for recent-onset psychosis in community settings.
Method:
We included 937 persons with recent-onset psychosis enrolled at 19 programs across New York State. Demographic, social and clinical data was collected at program entry and at 3, 6, 9 and 12 months. We used growth mixture models to identify occupational and social functioning trajectories and examined the association between trajectory class, baseline factors and symptoms during 1-year follow-up.
Results:
Four distinct trajectory classes of occupational and social functioning were identified. The converging (58.0%) class had disparate levels of functioning at baseline (low occupational, higher social) which eventually converged. The other classes had high-stable (14.8%), moderate-stable (17.8%) and low-improving (9.4%) trajectories. Female gender, educational attainment and private insurance status were significantly associated with the trajectory characterized by higher functioning, while living alone, homelessness, a longer period from psychosis onset to program enrollment, a schizophrenia diagnosis and cannabis use at enrollment were associated with the poorest trajectory. The differences in severity of symptoms by trajectory class diminished over time.
Conclusions:
Trajectories of occupational and social functioning showed substantial variation, but overall, remained stable or improved during 1-year follow-up. The relationship between symptoms and occupational and social functioning attenuated after the acute treatment phase.
Keywords: Early intervention, Psychosis, Functioning, Outcome, Trajectories
1. Introduction
Most non-affective psychotic disorders first appear between late adolescence and young adulthood (Anderson et al., 2019), a period of life that is characterized by important transitions in occupational and social development. The onset of psychosis is associated with serious short- and long-term negative consequences, including school and work failure, strained relationships, homelessness, social isolation, substance use and suicide (Abdel-Baki et al., 2017; Hakulinen et al., 2019; Schoenbaum et al., 2017). These inflict immense suffering on affected individuals and their families, and great costs to society (Hakulinen et al., 2019). Consequently, occupational and social functioning are main targets for intervention, as well as critical elements for recovery (Slade and Hayward, 2007).
Multicomponent programs for recent-onset psychosis providing specialized early intervention services (EIS) demonstrated superior outcomes compared to standard community care in all analyzable domains including psychiatric hospitalizations, involvement in work or school, and total, positive and negative symptom severity (Correll et al., 2018). However, the response to early psychosis care is heterogeneous and a significant subgroup experiences ongoing impairments in functioning (Nossel et al., 2018). Initially, studies on course and outcome in psychosis focused mostly on psychopathology and symptom remission (Hegarty et al., 1994). Studies that did incorporate levels of functioning were often limited by the use of dichotomized measures of functional remission or compared group means on scales assessed at baseline and follow-up. Such approaches may mask large subgroup differences. Further, although measures of occupational and social functioning often correlate with symptoms, an individual may have high occupational and social functioning, but still be symptomatic or vice versa (Oorschot et al., 2012). Given evidence that early level of functioning is more predictive of long-term disability than remission of positive and negative symptoms (Alvarez-Jimenez et al., 2012), functional impairment in the early phase of the illness should be a primary study focus.
Two studies of first-episode psychosis cohorts receiving EIS used longitudinal data to detect 1-year social and 3-year social-occupational functioning profiles (Chang et al., 2018; Hodgekins et al., 2015). Both found that most individuals had persistently poor trajectories while the proportion of people with improving trajectories ranged from 27% to 45%. Symptom severity at baseline, especially negative symptoms, was associated with class membership (Chang et al., 2018; Hodgekins et al., 2015). However, none of these studies examined the association between trajectories and symptoms over time, nor did they explore occupational and social domains separately.
Here, we report on the evolution of occupational and social functioning among individuals with a recent-onset, non-affective psychotic disorder enrolled at OnTrackNY, a multisite program offering a consistent model of EIS throughout New York State. The program serves diverse geographical areas throughout New York State, ranging from highly urban to rural sites. In addition to offering pharmacological treatment and psychosocial support, the program is specifically designed to help young people achieve life goals associated with school, work and social relationships (Bello et al., 2017).
1.1. Study objectives
First, we aimed to identify 1-year trajectories of occupational and social functioning, simultaneously and separately, in a clinical cohort of persons with recent-onset psychosis enrolled at OnTrackNY. Second, we sought to examine baseline factors associated with each trajectory class defined by the combination of both occupational and social functioning. Finally, we explored the association between these trajectories and symptoms over time.
2. Methods
2.1. Setting and participants
This study was conducted at 19 OnTrackNY programs which provide Coordinated Specialty Care, a type of EIS, in diverse settings across New York State (Bello et al., 2017). Programs are located within licensed outpatient clinics which are embedded in community mental health programs and academic medical centers. Individuals aged 16 to 30 with a recent-onset (<2 years) non-affective psychotic disorder are eligible for OnTrackNY services irrespective of insurance status. The study sample included individuals who enrolled between October 2013 and December 2017. Individuals with a diagnosed intellectual disability (IQ < 70), autism spectrum disorder, serious or chronic medical illness, a primary diagnosis of substance-induced psychosis, mood disorder with psychotic features or psychosis secondary to a general medical condition are not eligible for admission. The program is delivered by a multidisciplinary team that provides evidence-based psychopharmacological care, case management, cognitive behavioral-based therapy, family support and education, peer services, and supported employment and education services (Bello et al., 2017). Individuals receive treatment using a recovery-oriented, culturally competent, person-centered approach and principles of shared decision making to promote collaboration and a focus on the person’s preferences and needs. Case managers provide support for practical needs, stimulate engagement and collaboratively identify life goals, and use cognitive-behavioral principles to treat symptoms of psychosis and related mental health problems. Family support and education is provided to encourage family involvement to a level that is consistent with client and family preferences. Psychotherapy is flexibly offered in groups or individually and adjusted according to a person’s needs. Supported education and employment specialists use the individual placement and support model to integrate young people in the desired work or school setting. Lastly, peer specialists focus on building a relationship with participants, encourage engagement to the program, assist with providing resources in the community, and provide tools to empower young people to advocate for themselves (Bello et al., 2017; Dixon and Lieberman, 2015). The frequency of contact with the treatment team fluctuates based on the needs of the participant and acuity of presentation, but ranges between several times per week to once per month. The program does not have a fixed length, but the expectation is that individuals will be enrolled an average of two years, allowing for individuals who may need more or less time in the program. The interventions and procedures of the OnTrackNY model have been previously described in more detail (Bello et al., 2017; Mascayano et al., 2019; Nossel et al., 2018). Client- and program-level data are collected quarterly and submitted to the NYS Office of Mental Health for assessing treatment fidelity and for quality improvement. All identifiable information was removed from the research dataset. The use of deidentified OnTrackNY data for research purposes was approved by the NYS Psychiatric Institute Institutional Review Board.
2.2. Design
Data is collected by master- and doctoral-level, licensed clinicians (social workers, psychologists, mental health counselors) who act as the main point of contact for specific participants and their families. The primary clinician completes the forms based on all information provided by the participant, their family and other team members. The MIRECC GAF scores, like all other data elements, are collected for the primary purpose of program evaluation and quality improvement.
We used data from baseline and 3, 6, 9 and 12 months of follow-up. The baseline assessment was conducted within 14 days of enrollment in the program. At each site, data are collected using standardized admission, follow-up, and disenrollment forms based on chart review and reports from participants and their families. These data include demographic characteristics, family involvement, living situation and clinical information.
2.3. Measurements
Occupational and social functioning, and level of symptoms were assessed using the Mental Illness Research, Education, and Clinical Centers (MIRECC) Global Assessment of Functioning scale (GAF), a scale that has shown strong psychometric properties (Niv et al., 2007). Unlike the GAF scale, the MIRECC GAF disentangles symptoms from occupational and social functioning by scoring each of these three domains separately. The occupational functioning subscale of the MIRECC GAF includes 10 anchor points with descriptions reflecting the participant’s average level of functioning in their primary role as worker, student or homemaker during the 30 days prior to assessment. The social functioning subscale of the MIRECC GAF has a similar structure to the occupational functioning subscale and takes into account social interaction with friends and family, quality and quantity of relationships, ability to develop new relationships and interpersonal conflicts in the previous 30 days. The symptom subscale of the MIRECC GAF captures the participant’s worst level of functioning during the follow-up period (or the last three months for the baseline assessment) and is rated based on suicidality, mood, anxiety and psychotic symptoms. For all three subscales, scores can range from 0 to 100, and scores below 50 are considered in the impaired range while scores of 70 and above represent good functioning. To assess MIRECC GAF scoring accuracy, 63 clinicians scored three different vetted vignettes, producing a total of 149 scores for each subscale; these scores were then compared to gold standard scores determined by expert raters who mapped vignette details to specific criteria within the chosen decile. Accuracy was high for each subscale: 81.2% of social functioning scores, 88.6% of occupational functioning scores, and 89.3% of symptom scores were within 10 points of the gold standard.
Analyses were restricted to participants with at least one completed MIRECC GAF score. Predictor variables at baseline included information about demographics, living situation, family involvement and clinical variables. Demographic variables at enrollment included age, self-ascribed gender (male, female or other) and race-ethnicity (white, black, Hispanic, Asian or other), highest education (<HS, HS or GED, some college and higher), insurance status (uninsured, public, private) and urbanicity of site (highly urban/other). Sites were classified as either “highly urban” (all New York City sites except Staten Island) or “other” (including Staten Island and Upstate New York) using a cut-off of 10,000 people per square mile. Living situation was categorized as homeless, living alone or living with others, that is, with parents, other family or with (non-kin) others. Frequency of family contact was assessed as daily, weekly, or monthly or less. Additional clinical variables at enrollment included time from psychosis onset to first service use and time to OnTrackNY, substance use (any substances, including tobacco, any marijuana) and primary diagnosis (schizophrenia, schizoaffective, schizophreniform or other).
2.4. Statistical methods
Growth mixture models (GMMs) were used to identify different trajectory patterns of occupational and social functioning from baseline to 1-year follow-up. MIRECC GAF occupational and social functioning subscales (0–100) measured at baseline, 3, 6, 9, and 12 months were fit with GMM jointly in order to capture subgroups of participants with similar trajectory patterns taking both into account. This approach is consistent with the literature on psychosis outcomes using combined occupational and social outcome measures (Burns and Patrick, 2007; Nicholl et al., 2010). Preliminary data also indicated there was a moderate correlation over time between these domains, see Supplement 1. GMMs with random intercept, slope, and quadratic terms for trajectories of both occupational and social measures were fit with varying number of classes from 2 to 5 and goodness-of-fit indices of each model were compared. Missingness due to disengagement prior to 1-year follow-up was taken into account using a pattern-mixture model framework where latent class specific trajectory random effects were associated with a binary subject-level indicator of early disenrollment (prior to 1-year disenrollment versus 1-year completers) (Little, 1994), thus allowing valid estimates in case of non-random missing data (Hedeker and Gibbons, 1997). The optimal number of classes across the GMMs was selected based on low AIC, low BIC, high entropy, as well as on interpretability of the classes (Nylund et al., 2007). Additionally, the Lo-Mendell-Rubin likelihood ratio test (LMR-LRT) was applied to test whether k classes fit the data significantly better than k-1 classes. As a sensitivity analysis, additional GMMs were fit for occupational and social functioning separately to explore whether the number of trajectory classes or the amount of heterogeneity would vary by functional domain.
To examine the association of baseline characteristics with trajectory class from the GMM, we used each individual’s most likely class membership from the best fitting GMM. This so-called standard three-step approach (Van de Schoot et al., 2017) first fits the GMM, then places each individual into one trajectory class based on their most likely class membership from their posterior probabilities (step two), and then associates those classes with external variables (step three). We tested associations between most likely trajectory class membership and each variable using chi-square tests for categorical measures and one-way ANOVAs for continuous measures. In cases where the overall test was significant, pairwise differences were examined between all classes using chi-square tests and t-tests.
Longitudinal MIRECC GAF symptom scores were examined in relation to trajectories of occupational and social functioning using a mixed effects model. The model included fixed effects for time (as categorical), most likely class membership (based on the GMM above), their two-way interaction, a random effect for site and an autoregressive error covariance structure to account for within-subject correlation over time. Pre-specified contrasts were tested from the model for the mean change in MIRECC GAF symptoms by class in sequential follow-up assessments.
The GMMs were run using Mplus version 7 (computer code for the 4-class GMM is provided in Supplement 2), while all remaining analyses were done in SAS version 9.4. All statistical tests were two-sided at a 5% significance level.
3. Results
3.1. Study sample
The sample of this study consisted of 937 individuals with a mean age of 21.0 years (SD = 3.3). Of the 937 subjects with 1-year eligibility, 634 (67.6%) were enrolled for the entire 1-year study period, while 57 (6.1%), 143 (15.3%), 198 (21.1%) and 303 (32.3%) disenrolled by 3, 6, 9 and 12 months of follow-up, respectively. Missing data for MIRECC GAF ranged from 0.4% at baseline to 6.5% at 1-year follow-up. Correlations between all baseline variables are displayed in Supplement 3.
3.2. GMM trajectories of occupational and social functioning
The model fit statistics for the GMMs with varying class sizes are presented in Table 1. The entopy for all models from 2 to 5 classes was N0.90. The BIC was lowest (indicating best) for the 4 class model and the Lo-Mendell LRT indicated that the 5-class model was not significantly different from the 4-class model (p = .351). Therefore, along with interpretability of the classes (described below), the 4-class model was selected as the most parsimonious fit of the data.
Table 1.
Goodness-of-fit statistics for growth mixture models of MIRECC GAF social and occupational functioning with varying number of class.
| Fit statistic | Class size: |
|||
|---|---|---|---|---|
| 2-Classes | 3-Classes | 4-Classes | 5-Classes | |
| AIC | 61,002 | 60,803 | 60,648 | 60,626 |
| BIC | 61,245 | 61,079 | 60,958 | 60,970 |
| Entropy | 0.940 | 0.932 | 0.910 | 0.921 |
| Lo-Mendell LRT test p-value | <0.001 | <0.001 | <0.001 | 0.351 |
Abbreviations: AIC = Akaike’s Information Criterion; BIC=Bayesian Information Criterion; LMR-LRT = Lo-Mendell-Rubin Likelihood-ratio test; MIRECC = Mental Illness Research Education and Clinical Center; GAF = Global Assessment of Functioning.
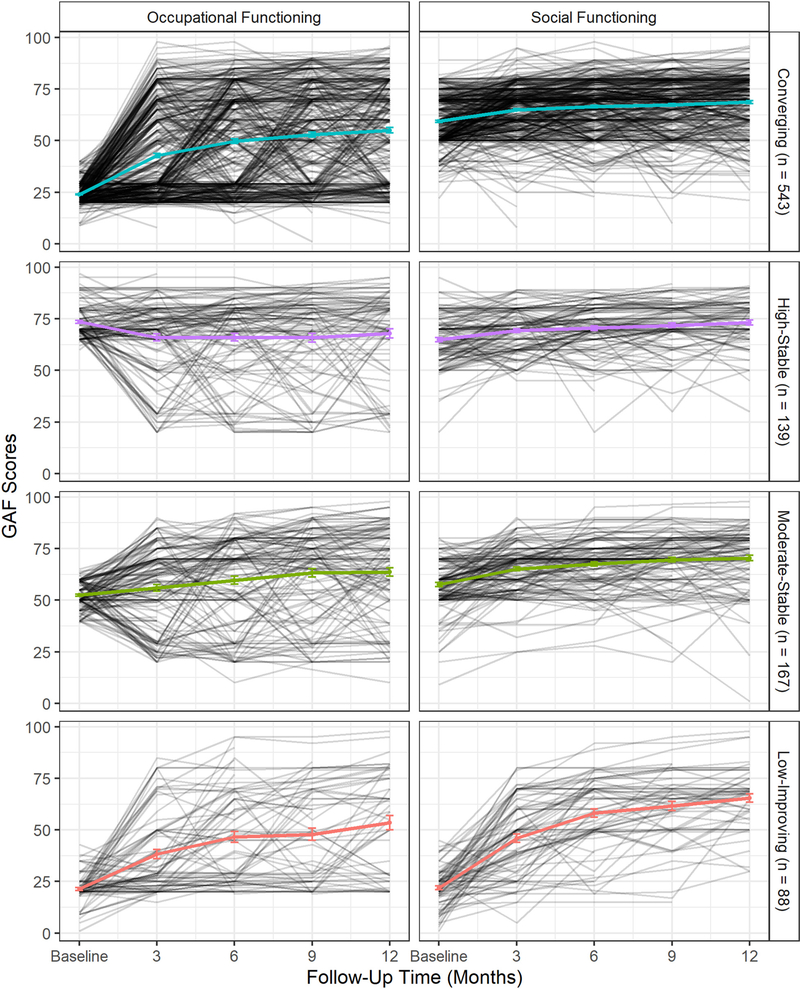
The observed means for the MIRECC GAF occupational and social functioning subscale scores by most likely class membership, along with the individual-level trajectories of each person identified by most likely class membership, are presented in Fig. 1 and in Supplement 4a. Of note, Fig. 1 displays substantial individual-level variability in trajectories within each of the trajectory classes. For example, within the Converging class there is a minority of individuals not exhibiting an increase in their occupational functioning and some individuals having lower social functioning at baseline. This does not mean the GMM classification is incorrect, it only reflects the reality of clinical heterogeneity. Each person is associated with the archetype trajectory pattern that they are most likely to follow based on the GMM, but each person varies in their probability of following the pattern.
Fig. 1.
Observed individual MIRECC GAF occupational functioning (left panel) and MIRECC GAF social functioning (right panel) scores by most likely class membership based on joint growth mixture model with 4 classes with an overlay of observed mean and 1-standard error bars.
3.3. Class 1 (n = 543): converging trajectory
This class includes the majority (58.0%) of participants and is characterized by impaired occupational functioning at baseline (no work or school activities) which improves with a fairly steep slope in the first 3 months reaching moderate level at 1-year follow-up, indicating that this class, on average, managed to become employed or enroll in school over time but still experienced some difficulties. At the same time, this class’ social functioning trajectory starts off higher at baseline and increases slightly to an average of still <70 at 1 year, signifying the presence of some meaningful relationships but ongoing difficulties including interpersonal conflict or avoidance. Compared to the High-stable and Moderate-stable trajectories, this class has relatively low occupational functioning with a gap in MIRECC GAF score of approximately 10 points that persisted throughout follow-up. In contrast, the level of social functioning is substantially higher and comparable to these other trajectories. This class has the largest difference between occupational and social functioning scores at baseline but the trajectories converge over 1-year follow-up.
3.4. Class 2 (n = 139): high-stable trajector
This class includes 14.8% of participants and is characterized by the highest intercept on both outcome domains with a deterioration in occupational functioning from baseline to 3 months, followed by a gradual improvement thereafter and an endpoint close to the fully functional range. The intercept of social functioning is in the moderate range and climbs to the fully functional range as well. This trajectory reflects a high-functioning class of participants engaged in meaningful social relationships and full-time employment or education.
3.5. Class 3 (n = 167): moderate-stable trajectory
This class includes 17.8% of the sample and has intercepts in the moderate range for both domains. Both curves have slightly positive slopes that remain stable in the moderate range for occupational functioning and increase to fully functional for social functioning. This moderate-stable trajectory comprises a class with meaningful relationships and school-work activities, but still experiences difficulties, especially in the occupational domain.
3.6. Class 4 (n = 88): low-improving trajectory
This class includes a minority (9.4%) of participants and has the lowest intercepts on both domains. The slope shows a strong increase in occupational functioning up to month 6 and a gradual increase afterward. Social functioning exhibits a steep slope at the first 3 months of follow-up which climbs to moderate level. This low-improving trajectory reflects a class that was not engaged in any work or school activities at baseline and who still experienced difficulties in school or while doing non-competitive work at follow-up. Their social functioning improved from a predominantly withdrawn life to a situation with some meaningful interpersonal relationships, but with some remaining challenges in the social sphere.
3.7. Occupational and social functioning trajectories and baseline measures
There were no notable differences in proportion of persons disenrolled by trajectory class (Table 2). The high-stable class was more often female, privately insured, living with someone who is not a family member, more highly educated and less often living alone, homeless, diagnosed with schizophrenia or using cannabis at program enrollment. The low-improving class was more often male, less educated, publicly insured, homeless, living alone, diagnosed with schizophrenia, using cannabis, and had the longest period between psychosis onset and program enrollment. In terms of urbanicity of study site, the converging class was more likely to be treated at a highly urban site than the low-improving class. The converging class was most likely to receive public insurance. The moderate-stable class had the lowest number of days between psychosis onset and program enrollment, and was most likely to receive a non-schizophrenia, psychotic disorder (delusional disorder, unspecified schizophrenia spectrum disorder) as primary diagnosis. Most likely class membership was also significantly associated with age, yet the absolute differences were small (maximum of 13 months difference between classes). No other significant between-group differences in race-ethnicity, family contact, or time to first mental health service use emerged.
Table 2.
Observed means and proportions of baseline predictors by most likely class membership and comparison of overall and pair-wise differences between classes.
| Measures | Overall (n = 937) |
Class 1 Converging (n = 543) |
Class 2 High-stable (n = 139) |
Class 3 Moderate-stable (n = 167) |
Class 4 Low-improving (n = 88) |
F or χ2 | pa | Post-hoc comparisonb |
|---|---|---|---|---|---|---|---|---|
| M (SD) or n (%) | M (SD) or n (%) | M (SD) or n (%) | M (SD) or n (%) | M (SD) or n (%) | ||||
| Number of individuals enrolled at 12 month follow-up | 634 (67.7%) | 369 (70.0%) | 92 (66.2%) | 117 (70.1%) | 56 (63.3%) | 1.25 | 0.741 | |
| Demographics at enrollment | ||||||||
| Gender (% female) | 236 (25.3%) | 133 (24.5%) | 51 (37.5%) | 42 (25.3%) | 10 (11.4%) | 19.91 | <0.001 | C1 ≠ C2 C1 ≠ C4 C2 ≠ C3 C2 ≠ C4 C3 ≠ C4 |
| Age at enrollment (SD) | 21.0 (3.3) | 21.4 (3.2) | 20.5 (3.4) | 20.5 (3.3) | 20.5 (3.3) | 6.28 | <0.001 | C1 ≠ C2 C1 ≠ C3 C1 ≠ C4 |
| Ethnicity/race | 7.45 | 0.591 | ||||||
| White (Non-Hispanic) | 252 (26.9%) | 137 (25.2%) | 45 (32.4%) | 46 (27.5%) | 24 (27.3%) | |||
| Black (Non-Hispanic) | 335 (35.8%) | 191 (35.2%) | 46 (33.1%) | 65 (38.9%) | 33 (37.5%) | |||
| Hispanic | 258 (27.5%) | 165 (30.4%) | 33 (23.7%) | 38 (22.8%) | 22 (25.0%) | |||
| Other | 92 (9.8%) | 50 (9.2%) | 15 (10.8%) | 18 (10.8%) | 9 (10.2%) | |||
| Highest education | 17.80 | 0.007 | C1 ≠ C4 C2 ≠ C4 |
|||||
| <HS | 264 (28.2%) | 137 (25.2%) | 36 (25.9%) | 57 (34.1%) | 34 (38.6%) | |||
| HS or GED | 183 (19.5%) | 108 (19.9%) | 22 (15.8%) | 30 (18.0%) | 23 (26.1%) | |||
| Some college | 490 (52.3%) | 298 (54.9%) | 81 (58.3%) | 80 (47.9%) | 31 (35.2%) | |||
| Insurance status | 28.44 | <0.001 | C1 ≠ C2 C2 ≠ C3 C2 ≠ C4 |
|||||
| Uninsured | 48 (5.1%) | 23 (4.2%) | 6 (4.3%) | 14 (8.4%) | 5 (5.7%) | |||
| Public | 430 (45.9%) | 273 (50.3%) | 41 (29.5%) | 74 (44.3%) | 42 (47.7%) | |||
| Private | 382 (40.8%) | 204 (37.6%) | 74 (53.2%) | 71 (42.5%) | 33 (37.5%) | |||
| Other/unknown | 77 (8.2%) | 43 (7.9%) | 18 (12.9%) | 8 (4.8%) | 8 (9.1%) | |||
| Urban/rural site | 9.83 | 0.020 | C1 ≠ C4 | |||||
| Highly urban | 554 (59.1%) | 341 (62.8%) | 78 (56.1%) | 94 (56.3%) | 41 (46.6%) | |||
| Other | 383 (40.9%) | 202 (37.2%) | 61 (43.9%) | 73 (43.7%) | 47 (53.4%) | |||
| Living situation and family contact | ||||||||
| Homelessness (% yes) | 53 (5.7%) | 35 (6.4%) | 0 (0.0%) | 8 (4.8%) | 10 (11.4%) | 14.57 | 0.002 | C1 ≠ C2 C2 ≠ C3 C2 ≠ C4 |
| Living situation | 29.41 | <0.001 | C1 ≠ C2 C2 ≠ C3 C2 ≠ C4 |
|||||
| Parents | 786 (83.9%) | 467 (86.0%) | 114 (82.0%) | 132 (79.0%) | 73 (83.0%) | |||
| Other family (not parents) | 63 (6.7%) | 32 (5.9%) | 6 (4.3%) | 19 (11.4%) | 6 (6.8%) | |||
| Alone | 41 (4.4%) | 25 (4.6%) | 2 (1.4%) | 8 (4.8%) | 6 (6.8%) | |||
| Other | 47 (5.0%) | 19 (3.5%) | 17 (12.2%) | 8 (4.8%) | 3 (3.4%) | |||
| Family contact | 10.27 | 0.114 | ||||||
| Daily | 841 (90.8%) | 494 (92.0%) | 121 (87.7%) | 153 (92.7%) | 73 (84.9%) | |||
| Weekly | 60 (6.5%) | 31 (5.8%) | 13 (9.4%) | 9 (5.5%) | 7 (8.1%) | |||
| Monthly or less | 25 (2.7%) | 12 (2.2%) | 4 (2.9%) | 3 (1.8%) | 6 (7.0%) | |||
| Clinical measures | ||||||||
| Time to first service use, days | 64.8 (139.7) | 60.8 (144.3) | 71.7 (128.2) | 78.5 (112.6) | 52.8 (170.9) | 1.01 | 0.389 | |
| Time to program, days | 230.7 (188.0) | 230.9 (187.9) | 244 (189.4) | 195.4 (174.9) | 275.4 (200.4) | 3.89 | 0.009 | C1 ≠ C3 C1 ≠ C4 C2 ≠ C3 C3 ≠ C4 |
| Primary diagnosis | 38.39 | <0.001 | C1 ≠ C2 C1 ≠ C3 C2 ≠ C4 C3 ≠ C4 |
|||||
| Schizophrenia (295.90) | 291 (31.1%) | 189 (34.8%) | 34 (24.5%) | 32 (19.2%) | 36 (40.9%) | |||
| Schizoaffective disorder (295.70) | 128 (13.7%) | 69 (12.7%) | 18 (12.9%) | 25 (15.0%) | 16 (18.2%) | |||
| Schizophreniform disorder (295.40) | 219 (23.4%) | 139 (25.6%) | 34 (24.5%) | 34 (20.4%) | 12 (13.6%) | |||
| Otherc | 299 (31.9%) | 146 (26.9%) | 53 (38.1%) | 76 (45.5%) | 24 (27.3%) | |||
| Any Substance use (including tobacco) (% yes) | 476 (50.8%) | 278 (51.2%) | 58 (41.7%) | 91 (54.5%) | 49 (55.7%) | 6.36 | 0.095 | |
| Any cannabis use (% yes) | 364 (38.8%) | 211 (38.9%) | 40 (28.8%) | 73 (43.7%) | 40 (45.5%) | 9.21 | 0.027 | C1 ≠ C2 C2 ≠ C3 C2 ≠ C4 |
Baseline differences are assessed using one-way ANOVAs for continuous measures and chi-square test for categorical measures.
Notation C1 ≠ C2 indicates the proportion or mean of the Measure in Class 1 is significantly different (p b 0.05) from Class 2, with other comparisons notated similarly.
Includes delusional disorder, other specified schizophrenia spectrum and other psychotic disorder, and unspecified schizophrenia spectrum disorder.
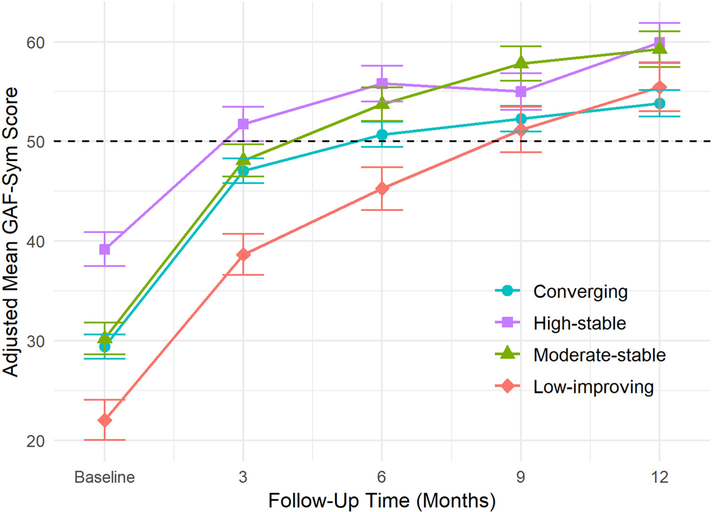
3.8. Occupational and social functioning trajectories and symptomatic functioning
The model estimated means for symptoms by most likely occupational and social functioning trajectory class membership are presented in Fig. 2. There was a significant class by time interaction indicating that the longitudinal changes in symptoms over the 1-year follow-up were different for the four classes (F(12,3759) = 3.36; p < .001). Starting from intercepts in the impaired range, the slopes are relatively steep in the first 3 months, showing large improvements in symptoms among all classes (all p < .001) (Table 3). After 3 months, all classes exhibit a significant positive trend up to month 6; however, after 6 months of follow-up, the slopes flatten out or have an erratic course, except for the low-improving class that shows a continuing positive trend. Across the four classes, the greatest improvements in symptoms are established within the first 3 months of program enrollment and the patterns converge after 6-month follow-up.
Fig. 2.
Model estimated means and 1-standard errors of MIRECC GAF symptoms score predicted by most likely class membership and follow-up time. The dashed reference line at MIRECC GAF score of 50 represents the lower threshold for moderate functioning.
Table 3.
Estimated change in MIRECC GAF symptoms across sequential follow-up visits by trajectory class.
| Time point | Class 1 converging (N = 543) |
Class 2 high-stable (N = 139) |
Class 3 moderate-stable (N = 167) |
Class 4 low-improving (N = 88) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Est | SE | p | Est | SE | p | Est | SE | p | Est | SE | p | |
| Mean at Admission | 29.40 | 1.22 | 39.17 | 1.70 | 30.21 | 1.59 | 22.02 | 2.01 | ||||
| 0–3 month change | 17.64 | 0.70 | <0.001 | 12.57 | 1.39 | <0.001 | 17.88 | 1.27 | <0.001 | 16.63 | 1.74 | <0.001 |
| 3–6 month change | 3.65 | 0.74 | <0.001 | 4.05 | 1.45 | 0.005 | 5.65 | 1.37 | <0.001 | 6.62 | 1.83 | <0.001 |
| 6–9 month change | 1.56 | 0.79 | 0.047 | −0.80 | 1.52 | 0.600 | 4.08 | 1.42 | 0.004 | 5.91 | 1.98 | 0.003 |
| 9–12 month change | 1.55 | 0.84 | 0.064 | 4.91 | 1.68 | 0.003 | 1.45 | 1.47 | 0.323 | 4.27 | 2.14 | 0.046 |
Abbreviations: MIRECC = Mental Illness Research Education and Clinical Center; GAF = Global Assessment of Functioning.
3.9. Sensitivity analyses
When modelled separately, the MIRECC GAF occupational functioning resulted in a 3-class model having good fit, and the MIRECC GAF social functioning resulted in a 2-class model having good fit without over-extracting classes (all class proportions are at least 5%), see Supplement 4b and Supplement 5 (Van de Schoot et al., 2017). Comparing the most likely class memberships of the joint GMM presented above with the classes from the models fit separately, finds the low-improving and converging classes merged into one class if only occupational functioning is considered (Supplement 6). Similarly, if only social functioning is considered, the high-stable, moderate-stable and converging are collapsed into one moderate-stable trajectory that includes almost 90% of the participants in the program.
4. Discussion
In this large clinical cohort of persons with recent-onset psychosis, we found four distinct trajectories of occupational and social functioning during one year of specialized EIS indicating substantial levels of heterogeneity in these functional domains. The majority, nearly two-thirds of the participants, had a converging trajectory with initial low occupational and moderate social functioning that converged over time. Only about one-tenth had the poorest low-improving trajectory. Importantly, when we modelled occupational and social functioning separately, we found fewer trajectories for both domains and less heterogeneity for social than occupational functioning in the early course of non-affective psychosis.
Our findings reflect a somewhat different picture than observed in previous studies conducted in other EIS settings. In a Hong Kong-based program, Chang et al. (Chang et al., 2018) detected four 3-year trajectories of combined social-occupational functioning using the Social and Occupational Functioning Assessment Scale (SOFAS) and found that 48% of participants had a persistently poor trajectory. In the UK, researchers found that up to 66% of participants in EIS had a low-stable, 1-year social functioning trajectory (Hodgekins et al., 2015). In contrast, the majority of participants in the current cohort exhibited early treatment gains, especially in the occupational domain. Of note, OnTrackNY programs offer intensive follow-up by an employment and education specialist, which has been shown to have a positive effect on vocational outcomes (Killackey et al., 2008). However, there may be other reasons for these discrepant findings, including the possibility that differential selection mechanisms and program inclusion criteria influence the demographic and clinical characteristics of participants enrolled in these programs. Nonetheless, the observed differences between programs in trajectories and outcomes are substantial and warrant further investigation.
Except for the high-stable class, treatment gains in both domains peaked within the first three months of follow-up, especially among those with low social or occupational functioning at baseline. Improvements generally flattened out after 6 months of follow-up. This is consistent with other studies suggesting that most gains in EIS are attained in the early course of treatment (Abdin et al., 2017; Austin et al., 2015; Chang et al., 2018).
Only one out of four trajectories exceeded the threshold towards the highest functional level, indicating that the vast majority of participants were enrolled in work or school and had meaningful interpersonal relationships, yet, after 1 year of EIS still experienced at least moderate impairments in these areas. Overall, our results imply that advancing initial occupational and social improvements towards a fully functional level remains a significant challenge and a key target for treatment in the majority of individuals enrolled in specialized EIS.
In terms of predictors, we found that female gender, higher educational attainment, having private insurance and being enrolled at a highly urban program site were significantly associated with trajectories characterized by higher functioning, while living alone, homelessness, cannabis use and a longer period between psychosis onset and program enrollment were predictive of the poorest trajectory. Our findings are consistent with previous studies showing that gender, living circumstances and cannabis use at program entry are associated with the prognosis of psychosis (Chang et al., 2018; Hall et al., 2019; Hodgekins et al., 2015). The relationship with insurance status and homelessness indicates that socioeconomic disparities may influence subsequent functional trajectories in psychosis, suggesting that disadvantaged groups may need additional interventions to fully benefit from EIS.
Symptom levels of the trajectories showed large improvements in the first months of treatment, but these attenuated over time. Overall, the symptom patterns showed less variation compared to the heterogeneous social, and especially occupational, trajectories. The general understanding is that while most persons with a first psychotic episode reach remission of positive symptoms, improvements in functioning lag behind (Santesteban-Echarri et al., 2017). We did not find evidence for a more favorable course of symptomatic than occupational or social functioning. In accordance with earlier work, our data suggests that relief of psychotic symptoms is not a necessary factor for good functioning in these domains (Shepherd et al., 1989; Strauss and Carpenter, 1977).
4.1. Limitations
In the interpretation of these findings several limitations need to be addressed. First, the findings are not based on a population-based cohort and we have no information on whether participants enrolled at OnTrackNY are a representative sample of all individuals with recent-onset psychosis in the inclusion area. However, the program accepts all individuals irrespective of insurance status which lowers financial barriers to enter services. Second, 303 (32.3%) individuals disenrolled before 1-year follow-up. This could potentially be a group with non-random missing data; however, we accounted for missingness by utilizing a pattern-mixture model framework and there was no evidence that the proportion of people that disenrolled before 1-year follow-up was significantly associated with assigned trajectory. Third, data was collected by clinicians, which may have introduced clinician bias. Several predictor variables, including substance use and diagnosis, were not assessed using a structured interview. We relied on clinician-rated MIRECC GAF occupational and social functioning subscales to assess functional trajectories, which is not the same as personal measures. Future research should incorporate self-report measures that cover the most meaningful aspects of outcomes for young people with psychosis. Furthermore, the MIRECC GAF symptom score covers a diverse mix of psychopathology including suicidality, anxiety, mood and psychotic symptoms. The lack of differentiation precludes conclusions about the relationship between specific symptoms and the different functional domains. Fourth, we only captured trajectories during the first year of EIS. Although some studies have shown that most changes occur in the early stages of treatment (Chang et al., 2018; Velthorst et al., 2016), it is possible that these trajectories change substantially beyond the 1-year treatment period. Fifth, the descriptions of the trajectories do no fully capture the course of occupational and social functioning over time nor their relative position in comparison to the other trajectories. Sixth, due to the lack of a control group we cannot separate the effect of EIS on occupational and social functioning from the natural course of functioning after the recent onset of psychotic disorder. Lastly, the current program includes individuals with non-affective psychotic disorder while other EIS programs include all psychotic disorders. Variations in diagnostic inclusion criteria across programs may affect the selection of individuals enrolled in such programs and, as a result, their outcome trajectories over time.
5. Conclusions
In this clinical cohort study of individuals with recent-onset psychosis enrolled in EIS, we found distinct and heterogeneous trajectories of occupational and social functioning during the first year of treatment. Most individuals had improving or stable occupational and social functioning patterns, which challenges previous findings showing that most people developing a psychotic disorder have a deteriorating course of functioning. However, the fact that the majority still experienced at least moderate impairments in these domains after 1-year follow-up indicates that they remain key targets for early intervention. Finally, variation in symptom severity decreased over time, suggesting that beyond a certain level of symptom relief improvements in functional domains are still attainable.
Supplementary Material
Acknowledgement
Els van der Ven is funded by a Rubicon grant from the Netherlands Organisation for Scientific Research (NWO).
Role of the funding source
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Declaration of competing interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.schres.2020.05.051.
References
- Abdel-Baki A, Ouellet-Plamondon C, Salvat É, Grar K, Potvin S, 2017. Symptomatic and functional outcomes of substance use disorder persistence 2 years after admission to a first-episode psychosis program. Psychiatry Res. 247, 113–119. [DOI] [PubMed] [Google Scholar]
- Abdin E, Chong SA, Vaingankar JA, Peh CX, Poon LY, Rao S, Verma S, Subramaniam M, 2017. Trajectories of positive, negative and general psychopathology symptoms in first episode psychosis and their relationship with functioning over a 2-year follow-up period. PLoS One 12 (11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez-Jimenez M, Gleeson J, Henry L, Harrigan S, Harris M, Killackey E, Bendall S, Amminger G, Yung A, Herrman H, 2012. Road to full recovery: longitudinal relationship between symptomatic remission and psychosocial recovery in first-episode psychosis over 7.5 years. Psychol. Med. 42 (3), 595–606. [DOI] [PubMed] [Google Scholar]
- Anderson KK, Norman R, MacDougall AG, Edwards J, Palaniyappan L, Lau C, Kurdyak P, 2019. Estimating the incidence of first-episode psychosis using population-based health administrative data to inform early psychosis intervention services. Psychol. Med. 49 (12), 2091–2099. [DOI] [PubMed] [Google Scholar]
- Austin SF, Mors O, Budtz-Jørgensen E, Secher RG, Hjorthøj CR, Bertelsen M, Jeppesen P, Petersen L, Thorup A, Nordentoft M, 2015. Long-term trajectories of positive and negative symptoms in first episode psychosis: a 10 year follow-up study in the OPUS cohort. Schizophr. Res. 168 (1–2), 84–91. [DOI] [PubMed] [Google Scholar]
- Bello I, Lee R, Malinovsky I, Watkins L, Nossel I, Smith T, Ngo H, Birnbaum M, Marino L, Sederer LI, 2017. OnTrackNY: the development of a coordinated specialty care program for individuals experiencing early psychosis. Psychiatr. Serv. 68 (4), 318–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns T, Patrick D, 2007. Social functioning as an outcome measure in schizophrenia studies. Acta Psychiatr. Scand. 116 (6), 403–418. [DOI] [PubMed] [Google Scholar]
- Chang WC, Chu AOK, Kwong VWY, Wong CSM, Hui CLM, Chan SKW, Lee EHM, Chen EYH, 2018. Patterns and predictors of trajectories for social and occupational functioning in patients presenting with first-episode non-affective psychosis: a three-year follow-up study. Schizophr. Res. 197, 131–137. [DOI] [PubMed] [Google Scholar]
- Correll CU, Galling B, Pawar A, Krivko A, Bonetto C, Ruggeri M, Craig TJ, Nordentoft M, Srihari VH, Guloksuz S, 2018. Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, meta-analysis, and meta-regression. JAMA Psychiatry 75 (6), 555–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon L, Lieberman J, 2015. Early psychosis intervention services: a work in progress. Schizophr. Bull. 41 (1), 23–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakulinen C, McGrath JJ, Timmerman A, Skipper N, Mortensen PB, Pedersen CB, Agerbo E, 2019. The association between early-onset schizophrenia with employment, income, education, and cohabitation status: nationwide study with 35 years of follow-up. Soc. Psychiatry Psychiatr. Epidemiol. 54 (11), 1343–1351. [DOI] [PubMed] [Google Scholar]
- Hall M-H, Holton KM, Öngür D, Montrose D, Keshavan MS, 2019. Longitudinal trajectory of early functional recovery in patients with first episode psychosis. Schizophr. Res. 209, 234–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedeker D, Gibbons RD, 1997. Application of random-effects pattern-mixture models for missing data in longitudinal studies. Psychol. Methods 2 (1), 64. [Google Scholar]
- Hegarty JD, Baldessarini RJ, Tohen M, Waternaux C, Oepen G, 1994. One hundred years of schizophrenia: a meta-analysis of the outcome literature. Am. J. Psychiatr. 151 (10), 1409–1416. [DOI] [PubMed] [Google Scholar]
- Hodgekins J, Birchwood M, Christopher R, Marshall M, Coker S, Everard L, Lester H, Jones P, Amos T, Singh S, 2015. Investigating trajectories of social recovery in individuals with first-episode psychosis: a latent class growth analysis. Br. J. Psychiatry 207 (6), 536–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killackey E, Jackson HJ, McGorry PD, 2008. Vocational intervention in first-episode psychosis: individual placement and support v. treatment as usual. Br. J. Psychiatry 193 (2), 114–120. [DOI] [PubMed] [Google Scholar]
- Little RJ, 1994. A class of pattern-mixture models for normal incomplete data. Biometrika 81 (3), 471–483. [Google Scholar]
- Mascayano F, Nossel I, Bello I, Smith T, Ngo H, Piscitelli S, Malinovsky I, Susser E, Dixon LB, 2019. Understanding the implementation of coordinated specialty care for early psychosis in New York state: a guide using the RE-AIM framework. Early Intervention Psychiatry, 1–5 10.1111/eip.12782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholl D, Nasrallah H, Nuamah I, Akhras K, Gagnon DD, Gopal S, 2010. Personal and social functioning in schizophrenia: defining a clinically meaningful measure of maintenance in relapse prevention. Curr. Med. Res. Opin. 26 (6), 1471–1484. [DOI] [PubMed] [Google Scholar]
- Niv N, Cohen AN, Sullivan G, Young AS, 2007. The MIRECC version of the global assessment of functioning scale: reliability and validity. Psychiatr. Serv. 58 (4), 529–535. [DOI] [PubMed] [Google Scholar]
- Nossel I, Wall MM, Scodes J, Marino LA, Zilkha S, Bello I, Malinovsky I, Lee R, Radigan M, Smith TE, 2018. Results of a coordinated specialty care program for early psychosis and predictors of outcomes. Psychiatr. Serv. 69 (8), 863–870. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO, 2007. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct. Equ. Model. 14 (4), 535–569. [Google Scholar]
- Oorschot M, Lataster T, Thewissen V, Lardinois M, Van Os J, Delespaul P, Myin-Germeys I, 2012. Symptomatic remission in psychosis and real-life functioning. Br. J. Psychiatry 201 (3), 215–220. [DOI] [PubMed] [Google Scholar]
- Santesteban-Echarri O, Paino M, Rice S, González-Blanch C, McGorry P, Gleeson J, Alvarez-Jimenez M, 2017. Predictors of functional recovery in first-episode psychosis: a systematic review and meta-analysis of longitudinal studies. Clin. Psychol. Rev. 58, 59–75. [DOI] [PubMed] [Google Scholar]
- Schoenbaum M, Sutherland JM, Chappel A, Azrin S, Goldstein AB, Rupp A, Heinssen RK, 2017. Twelve-month health care use and mortality in commercially insured young people with incident psychosis in the United States. Schizophr. Bull. 43 (6), 1262–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepherd M, Watt D, Falloon I, Smeeton N, 1989. The natural history of schizophrenia: a five-year follow-up study of outcome and prediction in a representative sample of schizophrenics. Psychol. Med. Monogr. Suppl. 15, 1–46. [DOI] [PubMed] [Google Scholar]
- Slade M, Hayward M, 2007. Recovery, Psychosis and Psychiatry: Research Is Better than Rhetoric. [DOI] [PubMed]
- Strauss JS, Carpenter WT, 1977. Prediction of outcome in Schizophrenia: III. Five-yearn outcome and its predictors. Arch. Gen. Psychiatry 34 (2), 159–163. [DOI] [PubMed] [Google Scholar]
- Van de Schoot R, Sijbrandij M, Winter SD, Depaoli S, Vermunt JK, 2017. The GRoLTS-checklist: guidelines for reporting on latent trajectory studies. Struct. Equ. Model. Multidiscip. J. 24 (3), 451–467. [Google Scholar]
- Velthorst E, Fett A-KJ, Reichenberg A, Perlman G, van Os J, Bromet EJ, Kotov R, 2016. The 20-year longitudinal trajectories of social functioning in individuals with psychotic disorders. Am. J. Psychiatr. 174 (11), 1075–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.