Abstract
Background:
Housing First (HF)-based interventions have been implemented in North America and beyond to help people exit homelessness. The effect of these interventions on access to primary and specialist care services is not well-defined. This study assesses the long-term effects of an HF intervention for homeless adults with mental illness on primary care physician (PCP) and non-primary care physician (non-PCP) visits.
Methods:
This is a secondary analysis of the At Home/Chez Soi study, a randomized trial of HF for homeless adults with mental illness in Toronto, Canada. High-need (HN) participants were randomized to HF with assertive community treatment (HF-ACT) or treatment as usual (TAU). Moderate needs (MN) participants were randomized to HF with intensive case management (HF-ICM) or TAU. The primary outcomes were the incidence and the number of visits to a PCP and non-PCP over 7-years post-randomization, compared to the 1-year pre-randomization.
Results:
Of 575 enrolled participants, 527 (80 HN and 347 MN) participants were included in the analyses. HN participants who received HF-ACT had a significant reduction in the number of visits to a PCP compared to TAU participants (ratio of rate ratios (RRR): 0.66, 95% CI: 0.48-0.93) and a significant reduction in the number of non-PCP visits compared with TAU participants (RRR: 0.64, 95% CI: 0.42-0.97) in the 7-years post-randomization compared to the 1-year pre-randomization. MN participants who received HF-ICM had a significant increase in incident visits to a PCP compared to TAU participants (RRR: 1.66, 95% CI: 1.10-2.50). No effect of HF-ICM was observed on the incidence or number of non-PCP visits.
Conclusion:
HF has differing effects on visits to PCPs and non-PCPs among homeless people with high and moderate needs for mental health supports. HF does not result in a consistent increase in PCP and non-PCP visits over a 7-year follow-up period. The At Home/Chez Soi study is registered with ISRCTN (ISRCTN, ISRCTN42520374).
Keywords: housing first, homelessness, mental illness, primary care, specialist physician care
Introduction
Primary care (PC) services play a critical role in achieving more equitable health outcomes.1-3 People who are socioeconomically excluded, such as those experiencing homelessness, face several barriers to accessing these services. Even in settings with universal health insurance (UHI), studies have found that homeless people have lower rates of PC use and preventive and outpatient services than the general population,4,5 despite higher rates of chronic health conditions, 6 infectious diseases, 7 traumatic brain injury, 8 and mental illness.
Further, the access and usage of other non-PC services provided in out-of-hospital care settings, such as visits to specialist physicians, may be even less frequent in homeless people. In a publicly funded UHI system, access to specialist care outside the hospital setting usually requires a referral from a primary care provider (PCP), who acts as the central coordinating point for the care of their patients.9,10 Thus, having no PCP can contribute to health disparities in accessing and receiving specialized care for disadvantaged populations. 11
Housing First (HF) interventions have been widely implemented in North America12,13 and Europe 14 to better address the complex social and health needs of people experiencing homelessness and mental illness. The HF approach is grounded in immediate access to housing without treatment preconditions, coupled with client-centered support services, as a critical starting point for recovery and social and health well-being.12,15 In theory, HF interventions have the potential to improve access to PC by increasing housing stability, reducing barriers to seeking care, and providing support that foster connections with PC providers.
The few studies that have assessed the effects of HF-based programs on PC utilization have been mainly non-randomized studies completed over periods less than 2 years.16,17 There is scant evidence on the long-term impacts of HF support on PC utilization. The objective of this study was to assess the long-term effects of an HF intervention for homeless people with mental illness on PCP and non-PCP visits over a 7-year follow-up period. We hypothesized that the HF intervention would increase both the incidence and number of PCP and non-PCP visits compared to treatment as usual (TAU).
Methods
Study Design and Participants
This study is a secondary analysis of health outcomes over a total of up to 7 years of follow-up among participants of the Toronto site of the At Home/Chez Soi (AH/CS) study, a randomized controlled trial (RCT).18,19 From October 1, 2009, to March 31, 2013, the Toronto site was part of the multi-site Canadian AH/CS study conducted in 5 cities (Vancouver, Winnipeg, Montreal, Moncton, and Toronto). 20 At the end of this period, participants at the Toronto site were asked to consent to be followed-up for an additional 4 years (January 1, 2014 to March 31, 2017).
A detailed description of the Toronto AH/CS study participants, recruitment and randomization, instruments, and primary outcomes, has been previously published.18,19 Briefly, study participants were recruited between October 2009 and July 31, 2011, through referrals from shelters, drop-in centers, hospitals, outreach and homeless services in Toronto, or by self-referrals. The study inclusion criteria were: (1) 18 years of age or older, (2) absolutely homeless or precariously housed, and (3) have a serious mental disorder. 21 Potential participants who did not have legal status in Canada or were already receiving intensive case management (ICM) or assertive community treatment (ACT) were excluded.18,19 The description and comparison of the main characteristics of participants have been published elsewhere. 18
Randomization and Intervention
Toronto AH/CS study participants were stratified based on their level of need for mental health support services into high-need (HN) and moderate-need (MN). HN participants were randomized to receive ACT plus rent supplements (HF-ACT) or TAU. MN participants were randomized to receive ICM plus rent supplements (HF-ICM) or TAU. All TAU participants had access to the local social, health, and housing support services. 19 The randomization was performed using computer-based adaptive randomization procedures at the study center. 20 A sample of 100 participants in each of the HF and TAU groups was considered adequate to detect significances for a 2-sided, .05 statistical level for the AH/CS outcomes. 18 Due to the nature of the intervention, it was not possible to blind the participants or the research team to the treatment allocation.
Data Sources
Study participants were linked to administrative health (AH) databases at ICES, an independent, non-profit research institute whose legal status under Ontario’s health information privacy law allows it to collect and analyze health care and demographic data, without consent, for health system evaluation and improvement. Linkage was performed using unique encoded identifiers, such as participant’s name, date of birth, and personal Ontario health insurance number. PCP and non-PCP visits were ascertained using the Ontario Health Insurance Plan (OHIP) database, which captures information on essentially all physician visits in the province. This dataset was analyzed at ICES.
Outcomes
The 2 main outcomes of this study were PCP visits and non-PCP visits, measured as (1) the incidence of a first visit per person-years of observation and (2) the total number of visits per person-years of observation. The PCP and non-PCP outcomes were ascertained during 2 periods: the 1 year prior to randomization and the 7 years after randomization to the HF intervention. When calculating the incidence of a first PCP and non-PCP visit, the period of observation (time-at-risk) for each participant was truncated on the date that their first PCP or non-PCP visit occurred. The period of observation was also truncated if the participant died or was de-enrolled from the Ontario health care system or if the participant’s consent for data linkage ended.
Statistical Analysis
An intention-to-treat analysis was used. The analyses included an offset for time-at-risk (log of person-years) for each participant. The person-years accounted for time that the participant was alive, eligible for and consenting to data linkage. The Poisson model was used to compare the number of PCP and non-PCP visits between the HF and TAU groups over the study periods (1-year pre-randomization and 0-7 years post-randomization). Generalized estimating equation models that included the intervention (HF vs TAU), period (1-year pre-randomization vs 0-7 years post-randomization), and an intervention × time interaction were used to assess differences in rate changes in outcomes between HF and TAU groups and to compare differences in the 0- to 7-year follow up period versus the 0 to 1 year pre-randomization period. Rates, rate ratios(RR), and the ratio of rate ratios(RRR) with 95% confidence intervals (95% CI) were estimated using SAS 9.4 statistical software.
Results
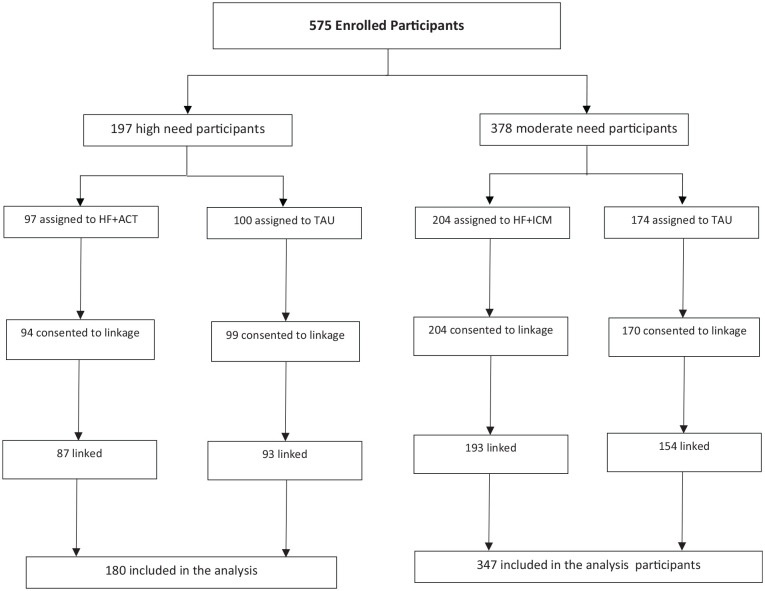
Of the 575 participants recruited at the Toronto site of the AH/CS study, 567 (98.6%) provided consent to have their AH databases linked, and 527 (92.9%) were successfully linked. Of the linked 527 participants, 180 (34.2%) were in the HN level, and 347 (65.8%) were in the MN level (Figure 1). Of these 527 participants, 414 (78.6%) participated over the 4-year extended follow-up period.
Figure 1.
Study flow chart.
The participants’ characteristics are presented in Table 1. Among those with HN, participants in the HF-ACT group were slightly younger than the TAU group. The HF-ACT group also had a higher percentage of women (34.5%) than the TAU group (20.4%). No other significant differences were observed.
Table 1.
Baseline Characteristic of Study Participants, by the Level of Needs for Mental Health Services and HF Intervention Groups, AH/CS Study, Toronto Site.
| High needs (N = 180) |
Moderate needs (N = 347) |
|||||||
|---|---|---|---|---|---|---|---|---|
| n | HF-ACT (n = 87) |
TAU (n = 93) |
P-value | n | HF-ICM (n = 193) |
TAU (n = 154) |
P-value | |
| % or mean ± SD | % or mean ± SD | % or mean ± SD | % or mean ± SD | |||||
| Demographics | ||||||||
| Age (years) | 180 | 37.67 ± 11.06 | 41.45 ± 12.03 | .030 | 347 | 39.56 ± 11.60 | 40.79 ± 12.51 | .345 |
| Gender (self-reported) | ||||||||
| Men | 129 | 57 (65.5%) | 72 (77.4%) | .042 | 234 | 131 (67.9%) | 103 (66.9%) | .931 |
| Women a | 49 | 30 (34.5%) | 19 (20.4%) | 108 | 61 (31.6%) | 47 (30.5%) | ||
| Ethno-racial identity (self-reported) | ||||||||
| Black | 55 | 30 (34.5%) | 25 (26.9%) | .451 | 115 | 73 (37.8%) | 42 (27.3%) | .068 |
| White | 82 | 39 (44.8%) | 43 (46.2%) | 112 | 54 (28.0%) | 58 (37.7%) | ||
| Other | 43 | 18 (20.7%) | 25 (26.9%) | 120 | 66 (34.2%) | 54 (35.1%) | ||
| Marital status | ||||||||
| Single | 127 | 65 (74.7%) | 62 (66.7%) | .428 | 231 | 128 (66.3%) | 103 (66.9%) | .883 |
| Other | 43 | 19 (21.8%) | 24 (25.9%) | 112 | 63 (32.6%) | 49 (31.8%) | ||
| Education | ||||||||
| Less than high school | 82 | 41 (47.1%) | 41 (44.1%) | .566 | 164 | 98 (50.8%) | 66 (42.9%) | .328 |
| Completed high school | 33 | 15 (17.2%) | 18 (19.4%) | 63 | 31 (16.1%) | 32 (20.8%) | ||
| Some post-secondary school | 51 | 29 (33.3%) | 22 (23.7%) | 112 | 61 (31.6%) | 51 (33.1%) | ||
| Homelessness during lifetime (years) | ||||||||
| <3 years | 65 | 35 (40.2%) | 30 (32.3%) | .543 | 171 | 97 (50.3%) | 74 (48.1%) | .663 |
| ≥3 years | 104 | 51 (58.6%) | 53 (57.0%) | 171 | 93 (48.2%) | 78 (50.6%) | ||
| Mental disorders b | ||||||||
| Major depressive episode | ||||||||
| No | 148 | 72 (82.8%) | 76 (81.7%) | .856 | 192 | 106 (54.9%) | 86 (55.8%) | .864 |
| Yes | 32 | 15 (17.2%) | 17 (18.3%) | 155 | 87 (45.1%) | 68 (44.2%) | ||
| Manic or hypomanic episode | ||||||||
| No | 163 | 76 (87.4%) | 87 (93.5%) | .156 | 309 | 171 (88.6%) | 138 (89.6%) | .765 |
| Yes | 17 | 11 (12.6%) | 6 (6.5%) | 38 | 22 (11.4%) | 16 (10.4%) | ||
| Post-traumatic stress disorder | ||||||||
| No | 157 | 74 (85.1%) | 83 (89.2%) | .400 | 250 | 137 (71.0%) | 113 (73.4%) | .622 |
| Yes | 23 | 13 (14.9%) | 10 (10.8%) | 97 | 56 (29.0%) | 41 (26.6%) | ||
| Panic disorder | ||||||||
| No | 172 | 82 (94.3%) | 90 (96.8%) | .412 | 281 | 157 (81.3%) | 124 (80.5%) | .845 |
| Yes | 8 | 1 to 5 (0.6 to 5.7%) c | 1 to 5 (1.1% to 5.5%) c | 66 | 36 (18.7%) | 30 (19.5%) | ||
| Mood disorder with psychotic features | ||||||||
| No | 134 | 65 (74.7%) | 69 (74.2%) | .936 | 282 | 158 (81.9%) | 124 (80.5%) | .750 |
| Yes | 46 | 22 (25.3%) | 24 (25.8%) | 65 | 35 (18.1%) | 30 (19.5%) | ||
| Psychotic disorder | ||||||||
| No | 74 | 37 (42.5%) | 37 (39.8%) | .709 | 260 | 145 (75.1%) | 115 (74.7%) | .923 |
| Yes | 106 | 50 (57.5%) | 56 (60.2%) | 87 | 48 (24.9%) | 39 (25.3%) | ||
| Substance abuse | ||||||||
| No | 161 | 75 (86.2%) | 86 (92.5%) | .172 | 318 | 175 (90.7%) | 143 (92.9%) | .465 |
| Yes | 19 | 12 (13.8%) | 7 (7.5%) | 29 | 18 (9.3%) | 11 (7.1%) | ||
| Substance dependence | ||||||||
| No | 111 | 48 (55.2%) | 63 (67.7%) | .083 | 217 | 124 (64.2%) | 93 (60.4%) | .461 |
| Yes | 69 | 39 (44.8%) | 30 (32.3%) | 130 | 69 (35.8%) | 61 (39.6%) | ||
| Alcohol abuse | ||||||||
| No | 148 | 70 (80.5%) | 78 (83.9%) | .550 | 304 | 165 (85.5%) | 139 (90.3%) | .181 |
| Yes | 32 | 17 (19.5%) | 15 (16.1%) | 43 | 28 (14.5%) | 15 (9.7%) | ||
| Alcohol dependence | ||||||||
| No | 124 | 60 (69.0%) | 64 (68.8%) | .983 | 247 | 145 (75.1%) | 102 (66.2%) | .069 |
| Yes | 56 | 27 (31.0%) | 29 (31.2%) | 100 | 48 (24.9%) | 33.8%) | ||
Includes seven transsexual or transgender participants.
Based on the DSM-IV criteria using the Mini International Neuropsychiatric Interview (MINI) version 6.0.
Absolute numbers less than six have been suppressed to reduce the risk of identification.
The number of outcome events and person-years of observation used to calculate the incidence and number of PCP and non-PCP visits are shown in Table 2.
Table 2.
The Number of Events and Person-Years of Observation for Incidence of Primary Care Physician (PCP) and Non-Primary Care Physician (Non-PCP) Visits and Number of PCP and Non-PCP Visits, According to the Need Level for Mental Health Services and HF Intervention Groups for the AH/CS Study Participants, Toronto Site.
| Outcome | Variable | High need |
Moderate need |
||
|---|---|---|---|---|---|
| HF | TAU | HF | TAU | ||
| PCP outcomes | |||||
| Incidence of a PCP visit | 1-year pre-randomization | ||||
| N | 80 | 83 | 158 | 134 | |
| Person-years | 27.48 | 26.48 | 76.98 | 46.43 | |
| 0- to 7-years post-randomization | |||||
| N | 86 | 93 | 190 | 151 | |
| Person-years | 41.45 | 27.95 | 83.12 | 77.95 | |
| Number of PCP visits | 1-year pre-randomization | ||||
| N | 1327 | 1446 | 2555 | 2227 | |
| Person-years | 87.00 | 93.00 | 193.00 | 154.00 | |
| 0- to 7-year post-randomization | |||||
| N | 5554 | 8675 | 13026 | 11037 | |
| Person-years | 559.47 | 571.38 | 1208.7 | 934.14 | |
| Non-PCP outcomes | |||||
| Incidence of a non-PCP visit | 1-year pre-randomization | ||||
| N | 84 | 79 | 155 | 127 | |
| Person-years | 27.40 | 37.29 | 90.76 | 65.55 | |
| 0- to 7-years post-randomization | |||||
| N | 87 | 91 | 190 | 150 | |
| Person-years | 20.77 | 36.41 | 126.57 | 104.23 | |
| Number of non-PCP visits | 1-year pre-randomization | ||||
| N | 2463 | 2111 | 2424 | 1786 | |
| Person-years | 87.00 | 93.00 | 193.00 | 154.00 | |
| 0- to 7-year post-randomization | |||||
| N | 9359 | 11958 | 15690 | 8484 | |
| Person-years | 559.47 | 571.38 | 1208.7 | 934.14 | |
Among HN participants, the incidence of a PCP visit during the 0 to 7 year post-randomization compared to the 1-year pre-randomization did not change significantly in the HF-ACT group (RR: 0.70; 95% CI, 0.44-1.13) or the TAU group (RR: 1.06; 95% CI, 0.72-1.56). The RRR (0.66; 95% CI, 0.36-1.22) indicates that the change in the HF-ACT group was not significantly different from that in the TAU group (Table 3).
Table 3.
Incidence and Number of Primary Care Physician (PCP) Visits Over According to the Need Level for Mental Health Services and HF Intervention Groups for the AH/CS Study Participants, Toronto Site.
| Outcome | Estimates | High need |
Moderate need |
||
|---|---|---|---|---|---|
| HF-ACT | TAU | HF-ICM | TAU | ||
| Incidence of a PCP visit | 1-year pre-randomization | ||||
| Rate per person-year (95% CI) | 2.95 (2.34-3.67) | 3.13 (2.50-3.89) | 2.05 (1.74-2.40) | 2.89 (2.42-3.42) | |
| Rate ratio (95% CI), HF vs TAU | 0.94 (0.64-1.39) | 0.71 (0.53-0.96) | |||
| 0- to 7-years post-randomization | |||||
| Rate per person-year (95% CI) | 2.08 (1.66-2.56) | 3.33 (2.69-4.08) | 2.29 (1.97-2.64) | 1.94 (1.64-2.27) | |
| Rate Ratio (95% CI), HF vs TAU | 0.62 (0.33-1.19) | 1.18 (0.77-1.82) | |||
| 0-7 years post-randomization vs 1-year pre-randomization | |||||
| Rate ratio (95% CI), post vs pre-randomization | 0.70 (0.44-1.13) | 1.06 (0.72-1.56) | 1.11 (0.87-1.42) | 0.67 (0.48-0.93) | |
| Ratio of rate ratios (95% CI), HF vs TAU | 0.66 (0.36-1.22) | 1.66 (1.10-2.50) | |||
| Number of PCP visits | 1-year pre-randomization | ||||
| Average rate (95% CI) | 15.25 (14.44-16.10) | 15.55 (14.76-16.37) | 13.24 (12.73- 3.76) | 14.46 (13.87-15.07) | |
| Rate ratio (95% CI), HF vs TAU | 0.98 (0.71-1.35) | 0.92 (0.70-1.19) | |||
| 0-7 years post-randomization | |||||
| Average rate (95% CI) | 9.93 (9.67-10.19) | 15.18 (14.86-15.51) | 10.78 (10.59-10.96) | 11.82 (11.60-12.04) | |
| Rate ratio (95% CI), HF vs TAU | 0.65 (0.46-0.93) | 0.91 (0.72-1.16) | |||
| 0-7 years post-randomization vs 1-year pre-randomization | |||||
| Rate ratio, post vs pre-randomization | 0.65 (0.51-0.83) | 0.98 (0.78-1.22) | 0.81 (0.69-0.97) | 0.82 (0.69-0.96) | |
| Ratio of rate ratios (95% CI), HF vs TAU | 0.66 (0.48-0.93) | 0.99 (0.79-1.26) | |||
In contrast, among MN participants, the incidence of PCP visits during 0 to 7 years post-randomization compared to 1-year pre-randomization did not change in the HF-ACT group, but decreased significantly in the TAU group (RR: 0.67; 95% CI, 0.48-0.93). The RRR (1.66; 95% CI, 1.10-2.50) shows that the change in the HF-ICM group was significantly higher than the change in the TAU group (Table 3).
Among HN participants, the rate for the number of PCP visits during the 0 to 7 years post-randomization compared to the 1-year pre-randomization decreased significantly in the HF-ACT group (RR: 0.65; 95% CI 0.51-0.83), but not in the TAU group (RR: 0.98; 95% CI, 0.78-1.22). The RRR (0.66; 95% CI, 0.48-0.93) indicates that this change in the HF-ACT group was of significantly greater magnitude than the change in the TAU group (Table 3).
In the MN participants, the rate of PCP visits during 0 to 7 years post-randomization compared to 1-year pre-randomization decreased significantly in both the HF-ICM group (RR: 0.81; 95% CI 0.69-0.97) and the TAU group (RR: 0.82; 95% CI, 0.69-0.96) (Table 3). The RRR (0.99; 95% CI, 0.79-1.26) indicates that the change in the HF-ICM group was not significantly different from that in the TAU group (Table 3).
Regarding the incidence rate of a non-PCP visit, no statistically significant change was found for the intervention groups in both HN and MN participants (Table 4). When comparing the changes (RRR) between HF intervention groups, no changes were observed either in the HN participants or in the MN participants (Table 4).
Table 4.
Incidence and Number of Non-Primary Care Physician (Non-PCP) Visits According to the Level of Needs for Mental Health Services and HF Intervention Groups for the AH/CS Study Participants, Toronto Site.
| Outcome | Estimates | High need |
Moderate need |
||
|---|---|---|---|---|---|
| HF-ACT | TAU | HF-ICM | TAU | ||
| Incidence of a non-PCP visit | 1-year pre-randomization | ||||
| Rate per person-year (95% CI) | 3.07 (2.45-3.80) | 2.12 (1.68-2.64) | 1.71 (1.45-2.00) | 1.94 (1.62-2.31) | |
| Rate ratio (95% CI), HF vs TAU | 1.45 (1.03-2.04) | 0.88 (0.68-1.14) | |||
| 0- to 7-years post-randomization | |||||
| Rate per person-year (95% CI) | 4.19 (3.35-5.17) | 2.50 (2.01-3.07) | 1.50 (1.30-1.73) | 1.44 (1.22-1.69) | |
| Rate ratio (95% CI), HF vs TAU | 1.68 (0.82-3.41) | 1.04 (0.73-1.50) | |||
| 0-7 years post-randomization vs 1-year pre-randomization | |||||
| Rate ratio (95% CI), post vs pre-randomization | 1.37 (0.84-2.22) | 1.18 (0.67-2.09) | 0.88 (0.70-1.10) | 0.74 (0.57-0.97) | |
| Ratio of rate ratios (95% CI), HF vs TAU | 1.16 (0.55-2.45) | 1.18 (0.84-1.68) | |||
| Number of non-PCP visits | 1-year pre-randomization | ||||
| Average rate (95% CI) | 28.31 (27.20-29.45) | 22.7 (21.74-23.69) | 12.56 (12.06-13.07) | 11.6 (11.07-12.15) | |
| Rate ratio (95% CI), HF vs TAU | 1.25 (0.85-1.82) | 1.08 (0.78-1.51) | |||
| 0-7 years post-randomization | |||||
| Average rate (95% CI) | 16.73 (16.39-17.07) | 20.93 (20.55-21.31) | 12.98 (12.78-13.19) | 9.08 (8.89-9.28) | |
| Rate ratio (95% CI), HF vs TAU | 0.80 (0.57-1.12) | 1.43 (1.07-1.91) | |||
| 0-7 years post-randomization vs 1-year pre-randomization | |||||
| Rate ratio, post vs pre-randomization | 0.59 (0.44-0.80) | 0.92 (0.69-1.23) | 1.03 (0.83-1.28) | 0.78 (0.60-1.02) | |
| Ratio of rate ratios (95% CI), HF vs TAU | 0.64 (0.42-0.97) | 1.32 (0.94-1.86) | |||
Regarding the rate of non-PCP visits during the 0 to 7 years post-randomization to the 1-year pre-randomization, a significant decrease was observed only for the HN participants of the HF-ACT group (RR: 0.59, 95% CI, 44-0.80). Similar findings were observed in the rate change for the number of non-PCP visits in the HF-ACT group compared to the TAU group (RRR: 0.64, 95% CI, 0.42-0.97). No significant changes in the number of non-PCP were observed for the MN participants (Table 4).
Discussion
We used AH databases to examine the effects of HF on the use of PCP and non-PCP visits over a 7-year follow-up period. In this analysis of changes in the HF intervention groups compared to the TAU groups, HF had differential effects depending on participants’ level of need for mental health supports. Among individuals with HN, HF-ACT did not significantly affect the incidence of a PCP and non-PCP visit but significantly decreased the number of both PCP visits and non-PCP visits over time. In contrast, HF-ICM significantly increased the incidence of a PCP visit among individuals with MN but not the number of PCP visits over time. There was no significant effect of HF-ICM on changes related to the incidence and number of non-PCP visits.
Compared with housed or the general population, a recent study using ICES databases (similar data source for the present study), 22 found that during March to July 2019 (pre-COVID-19), there were on average 7.66 visits per 1000 people/day to PCPs in the province of Ontario (the setting of our study), while in our participants overall, there were on average 14.34 person-year visits (or 39.3 visits per 1000 people/day) to PCPs during 1-year pre-randomization. This finding suggests that our study population tended to accumulate more visits to PCs than the general population. In homeless populations, very few previous RCTs of HF have examined the effects of this intervention on PC utilization. In a 1-year follow-up study in the United States, researchers found that veterans with a history of homelessness that received HF services through the HUD-VASH program had more visits to PC services than other low-income and homeless veterans who did not receive HF. 16 Most other RCTs of HF have examined the effect of HF on emergency department visits and hospitalizations, but not PCP visits.23,24 No previous studies have assessed the impact of a housing intervention for homeless people on non-PCP visits outside a hospital-based setting.
Our findings indicate that although HF clearly reduces homelessness over 7 years of follow-up, 18 it does not result in a consistent increase in PCP and non-PCP visits over this time frame. Among high-need individuals who received HF with ACT, the observation of a reduction in the rate of PCP and non-PCP visits was unexpected. It is possible that the HF-ACT model, in which a team of psychiatrists, case managers, and peer support workers provide high-intensity supports in the community, including health supports (eg, mental health assessments and treatment and harm reduction and substance use disorders), reduces participants’ desire or need for frequent PCP and non-PCP visits.19,25 It is also possible that due to severe mental illness and functional impairment, participants who receive HF-ACT may not seek help or attend scheduled appointments 26 with both PCPs and non-PCPs despite receiving HF support. Seeking health care is voluntary rather than a requirement under the HF framework.12,13 Further, stigma and discrimination within the healthcare system toward vulnerable people could constitute a barrier to more frequently accessing PC services by this population. 27
Among moderate-need individuals who received HF-ICM, the observed effect of an increased incidence of PCP visits was expected, as one of the goals of ICM is to connect clients to PC and other services in the community. In addition, the provision of stable housing through the HF intervention is expected to reduce barriers to connecting with PC. However, the lack of a significant effect on the number of PCP and non-PCP visits indicates that in this population, an initial connection to a PCP does not necessarily lead to more frequent PCP and non-PCP visits over time. Regarding non-significant findings on the non-PCP visits outcomes, this may be explained by the potential connection between fewer visits to PCPs and fewer visits to non-PCPs, since having a PCP facilitates access to more specialized healthcare services. 9 It is also likely that having a PCP supports the delivery of more holistic management or treatment of individuals’ health needs 9 without requiring further assessment or treatment by other health specialists.
The study’s findings have significant implications for practice and research. First, organizations providing HF, particularly in conjunction with ACT for homeless people with HN for mental health services, should monitor their clients’ need for and potential under-utilization of PC services and access to specialized health services outside the hospital.
Second, organizations providing HF should assess the initial connection of their clients with PCPs and other medical specialists in out-of-hospital settings and their ongoing rate of PCP and non-PCP visits over time to inform efforts to improve care. Further, integrating PC services within existing HF and other types of support programs serving people with lived experiences of homelessness could reduce existing structural and individual barriers to accessing and receiving PC.
Third, PCPs and health systems that provide care for people experiencing homelessness and those who have transitioned out of homelessness should be aware that HF interventions do not necessarily ensure successful ongoing connection to PC. Thus, PC systems may need to develop collaborations with their patients’ social service providers to ensure these individuals receive appropriate preventive care. Furthermore, PCPs could contribute to leading changes in the way they engage with vulnerable people to facilitate their access to PC and non-PC services.28,29 Additionally, PCPs, non-PCPs, and support services could lead coordinating efforts 9 in partnership with other allied health professionals (including nurses, nutritionists, physiotherapists, psychologists, and social workers) to enhance and provide timely and appropriate multidisciplinary health support29,30 for addressing the complex health needs of homeless people.29,31,32
Fourth, PCPs and non-PCPs could also advocate for collecting and sharing medical and non-medical information with health and social support providers working within the existing social support programs (eg, psychiatrists, nurses, social workers, case managers working with HF clients) 29 ; carry out closer and frequent health and well-being follow-up visits, and allocate more time for the medical encounter with this population. 28 All of this has the potential to promote and facilitate the continuity of healthcare 28 through a more collaborative PC model. 30
Fifth, promote a participatory learning approach and skills-building activities 33 of the current and future PCPs and Non-PCPs and allied PC professionals on homelessness and mental illness and its contributing factors, and how it intersects with systemic issues such as racism, stigma, and discrimination within primary care and social support settings,5,33,34 and building trusting professional relationships with people with lived experiences of homelessness28,35 may also contribute to increasing the help-seeking behavior of people experiencing homelessness, and the quality of care they receive within the in primary care services.34,36
Finally, future studies should assess the extent of unmet needs for primary care among formerly homeless individuals receiving HF services. Also, the effect of the HF intervention on PC-related health outcomes such as management of chronic diseases and mental health and substance use symptomatology and access and delivery of preventive or screening services in people with lived or recent experiences of homelessness need further research. Since the incidence and number of PCP and non-PCP visits may not always be a good proxy to assess potential improvements or decline in individuals’ health status, such studies should include qualitative approaches to have a better and more comprehensive understanding of the dynamic on how HF-based approaches and other contributing factors or circumstances mitigate or increase the usage of primary care and other out-of-hospital care services by homeless people.
The present study used a rigorous randomized controlled design to examine the long-term impact of an HF intervention on PCP and non-PCP visits. PCP and non-PCP visits were ascertained using highly reliable administrative databases rather than self-report, reducing the possibility of misreporting. However, further studies comparing the number of visits to PCPs and non-PCPs of homeless and housed people with and without mental illness can provide a further understanding of the contribution of access to care in these populations.
This study has certain limitations. First, eligibility for the study required the presence of a mental disorder; therefore, our findings may not be generalizable to homeless individuals without mental illness. Second, data on the reasons for visits (eg, preventive care, diagnosis, treatment, or follow-up) and the quality of care provided during these visits were not available. Third, we did not have data on PC services provided by other health care professionals such as nurse practitioners. In Ontario, where this study was conducted, these professionals are paid by salary rather than by billing the Ontario Health Insurance Plan, which was our source for healthcare utilization data. Fourth, as the study was conducted in a setting with a Universal Health Insurance system, the findings may not be generalizable to settings where homeless individuals do not have access to universal health coverage. Further studies in other jurisdictions may provide further insight into the effects of HF programs on PC and non-PC services utilization.
In conclusion, HF has differing effects on visits to PCPs and non-PCPs among homeless people with high and moderate needs for mental health supports. HF does not result in a consistent increase in PCP and non-PCP visits over a 7-year follow-up period.
Acknowledgments
We thank the participants in the AH/CS study for their involvement and the AH/CS project team, site coordinators, and service providers who have contributed to the design, implementation, and follow-up of participants.
Footnotes
Author Contributions: Stephen W. Hwang, Vicky Stergiopoulos, Patricia O’Campo, Rosane Nisenbaum, Cilia Mejia-Lancheros conceptualized the study and analysis. James Lachaud, Cilia Mejia-Lancheros, and Rosane Nisenbaum oversaw and validated the statistical analyses. Cilia Mejia-Lancheros carried out the first interpretation of the study findings and drafted the manuscript. James Lachaud, Patsy Lee, and Matthew J. To contributed to the validation and interpretation of the findings and critical revision and editing of the manuscript. Rosane Nisenbaum, Patricia O’Campo, Vicky Stergiopoulos, and Stephen W. Hwang made substantive intellectual contributions in the interpretation of the findings and revision of the final version of the manuscript. Stephen W. Hwang edited the final version of the manuscript. Patricia O’Campo, Vicky Stergiopoulos, and Stephen W. Hwang are also the co-principal investigators of the Toronto site of the AH/CS study. All co-authors approved the final version of the manuscript and are accountable for all aspects of the work.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The Toronto site of the At Home/Chez Soi study was funded by the Mental Health Commission of Canada, the Ontario Ministry of Health and Long-Term Care (HSRF #259), and the Canadian Institute of Health Research (CIHR MOP-130405). The present study also received funding from a St. Michael’s Hospital Research Training Centre Scholarship (#2019) awarded to Dr. Cilia Mejia-Lancheros. This study was also supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). The funding institutions had no role in the study design, collection, analysis and interpretation of the data, nor in the preparation, revision, or approval of the present manuscript. No endorsement by the OHDP, its partners, or the Province of Ontario and the funding institutions is intended or should be inferred. The views expressed in this publication are solely those of the authors.
Ethics Approvals: The AH/CS study received approval from the Research Ethics Board of St Michael’s Hospital, Toronto, Canada. Participants provided written informed consent to participate in the study and to have their health administrative records linked. This study was registered with ISRCTN (ISRCTN42520374).
ORCID iD: Cilia Mejia-Lancheros  https://orcid.org/0000-0003-1131-8439
https://orcid.org/0000-0003-1131-8439
Data Availability: The dataset from this study is held securely in coded form at ICES. While legal data sharing agreements between ICES and data providers (eg, healthcare organizations and government) prohibit ICES from making the dataset publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS (email: das@ices.on.ca). The full dataset creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification. The AH/CS survey dataset cannot be made publicly available due to the sensitive nature of the data and agreements and procedures governing the use of the dataset that were established by the study sponsor, the Mental Health Commission of Canada. However, anonymized participant data from the AH/CS study (excluding data held at ICES) can be made available to investigators who complete the following steps: (1) present a study proposal that has received approval from an independent research committee or research ethics board; (2) provide a data request for review by the AH/CS data access committee; (3) following approval of the request, execute a data-sharing agreement between the investigators and the AH/CS data custodians. Study proposals and data access requests should be sent to Evie Gogosis (Evie.Gogosis@unityhealth.to), research manager for the Toronto site of the AH/CS study, and to Dr. Stephen Hwang (Stephen.Hwang@unityhealth.to), co-principal investigator of the Toronto site of the AH/CS study.
References
- 1. Startfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Starfield B, Lemke KW, Bernhardt T, Foldes SS, Forrest CB, Weiner JP. Comorbidity: implications for the importance of primary care in “case” management. Ann Fam Med. 2003;1(1):8-14. doi: 10.1370/afm.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shi L. The impact of primary care: a focused review. Scientifica (Cairo). 2012;2012:1-22. doi: 10.6064/2012/432892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. O’Carroll A, Wainwright D. Making sense of street chaos: an ethnographic exploration of homeless people’s health service utilization. Int J Equity Health. 2019;18:1-22. doi: 10.1186/s12939-019-1002-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gunner E, Chandan SK, Yahyouche A, et al. Provision and accessibility of primary healthcare services for people who are homeless: a qualitative study of patient perspectives in the UK. Br J Gen Pract. 2019;69:e526-e536. doi: 10.3399/bjgp19X704633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014;384(9953):1529-1540. doi: 10.1016/S0140-6736(14)61132-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Beijer U, Wolf A, Fazel S. Prevalence of tuberculosis, hepatitis C virus, and HIV in homeless people: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(11):859-870. doi: 10.1016/S1473-3099(12)70177-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Stubbs JL, Thornton AE, Sevick JM, et al. Traumatic brain injury in homeless and marginally housed individuals: a systematic review and meta-analysis. Lancet Public Health. 2020;5(1):e19-e32. doi: 10.1016/S2468-2667(19)30188-4 [DOI] [PubMed] [Google Scholar]
- 9. Bodenheimer T, Lo B, Casalino L. Primary care physicians should be coordinators, not gatekeepers. J Am Med Assoc. 1999;281:2045-2049. doi: 10.1001/jama.281.21.2045 [DOI] [PubMed] [Google Scholar]
- 10. Sarma S, Devlin RA, Hogg W. Physician’s production of primary care in Ontario, Canada. Health Econ. 2010;19:14-30. doi: 10.1002/hec [DOI] [PubMed] [Google Scholar]
- 11. Hutchison B, Levesque JF, Strumpf E, Coyle N. Primary health care in Canada: systems in motion. Milbank Q. 2011; 89(2):256-288. doi: 10.1111/j.1468-0009.2011.00628.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Padgett DK, Heywood BF, Tsemberis S. Housing First: Ending Homelessness, Transforming Systems, and Changing Lives. Oxford University Press; 2016. [DOI] [PubMed] [Google Scholar]
- 13. Nelson G, Aubry T, Tsemberis S, Macnaughton E. Psychology and public policy: the story of a Canadian Housing First project for homeless people with mental illness. Can Psychol. 2020. 61(3):257-268. doi: 10.1037/cap0000206 [DOI] [Google Scholar]
- 14. Busch-Geertsema V. Housing First Europe. Final Report. European Union Programme for Employment and Social Security – PROGRESS; 2013. [Google Scholar]
- 15. Tsemberis S. The Pathways Model to End Homelessness for People with Mental Illness and Addiction. Revised ed. Hazelden Information & Educational Services; 2015. [Google Scholar]
- 16. Gabrielian S, Yuan AH, Andersen RM, Rubenstein LV, Gelberg L. VA health service utilization for homeless and low-income veterans: a spotlight on the VA supportive housing (VASH) program in greater Los Angeles. Med Care. 2014;52(5):454-461. doi: 10.1097/MLR.0000000000000112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Weinstein LC, La Noue MD, Plumb JD, King H, Brianna S, Tsemberis S. A primary care-public health partnership addressing homelessness, serious mental illness, and health disparities. J Am Board Fam Med. 2013;26:279-287. doi: 10.3122/jabfm.2013.03.120239 [DOI] [PubMed] [Google Scholar]
- 18. Stergiopoulos V, Mejia-lancheros C, Nisenbaum R, et al. Long-term effects of rent supplements and mental health support services on housing and health outcomes of homeless adults with mental illness: extension study of the At Home/Chez Soi randomised controlled trial. Lancet Psychiatry. 2019;6(11):915-925. doi: 10.1016/S2215-0366(19)30371-2 [DOI] [PubMed] [Google Scholar]
- 19. Hwang SW, Stergiopoulos V, O’Campo P, Gozdzik A. Ending homelessness among people with mental illness: the At Home/Chez Soi randomized trial of a Housing First intervention in Toronto. BMC Public Health. 2012;12(1):787. doi: 10.1186/1471-2458-12-787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Goering PNPN, Streiner DLDL, Adair C, et al. The At Home/Chez Soi trial protocol: a pragmatic, multi-site, randomised controlled trial of a Housing First intervention for homeless individuals with mental illness in five Canadian cities. BMJ Open. 2011;1(2):e000323. doi: 10.1136/bmjopen-2011-000323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(SUPPL. 20):22-33. doi: 10.1016/S0924-9338(99)80239-9 [DOI] [PubMed] [Google Scholar]
- 22. Glazier RH, Green ME, Wu FC, Frymire E, Kopp A, Kiran T. Shifts in office and virtual primary care during the early COVID-19 pandemic in Ontario, Canada. CMAJ. 2021;193:E200-E210. doi: 10.1503/cmaj.202303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stergiopoulos V, Hwang SW, Gozdzik A, et al. Effect of scattered-site housing using rent supplements and intensive case management on housing stability among homeless adults with mental illness: a randomized trial. JAMA. 2015;313(9):905-915. doi: 10.1001/jama.2015.1163 [DOI] [PubMed] [Google Scholar]
- 24. Sadowski LS, Kee RA, Vanderweele TJ, Buchanan D. Effect of a housing and case management program on emergency department visitsand hospitalizations among chronically ill homeless adults a randomized trial. JAMA. 2009;301(17): 1771-1778. doi: 10.1001/jama.2009.561 [DOI] [PubMed] [Google Scholar]
- 25. Stenius-Ayoade A, Haaramo P, Erkkilä E, et al. Mental disorders and the use of primary health care services among homeless shelter users in the Helsinki metropolitan area, Finland. BMC Health Serv Res. 2017;17(1):1-11. doi: 10.1186/s12913-017-2372-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Centre for Addiction and Mental Health. Mental Health and Primary Care Policy Framework. Centre for Addiction and Mental Health; 2016. [Google Scholar]
- 27. Knaak S, Mantler E, Szeto A. Mental illness-related stigma in healthcare: barriers to access and care and evidence-based solutions. Healthc Manag Forum. 2017;30(2):111-116. doi: 10.1177/0840470416679413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jego M, Grassineau D, Balique H, et al. Improving access and continuity of care for homeless people: how could general practitioners effectively contribute? Results from a mixed study. BMJ Open. 2016;6(11). doi: 10.1136/bmjopen-2016-013610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Andermann A, Bloch G, Goel R, et al. Caring for patients with lived experience of homelessness. Can Fam Physician. 2020;66(8):563-570. [PMC free article] [PubMed] [Google Scholar]
- 30. Stergiopoulos V, Schuler A, Nisenbaum R, et al. The effectiveness of an integrated collaborative care model vs. a shifted outpatient collaborative care model on community functioning, residential stability, and health service use among homeless adults with mental illness: a quasi-experimental study. BMC Health Serv Res. 2015;15:348. doi: 10.1186/s12913-015-1014-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Desai MM, Rosenheck RA. Unmet need for medical care among homeless adults with serious mental illness. Gen Hosp Psychiatry. 2005;27(6):418-425. doi: 10.1016/j.genhosppsych.2005.06.003 [DOI] [PubMed] [Google Scholar]
- 32. Wright NMJ, Tompkins CNE. How can health services effectively meet the health needs of homeless people? Br J Gen Pract. 2006;56(525):286-293. [PMC free article] [PubMed] [Google Scholar]
- 33. Nyblade L, Stockton MA, Giger K, et al. Stigma in health facilities: why it matters and how we can change it. BMC Med. 2019;17:25. doi: 10.1186/s12916-019-1256-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Parker D, Byng R, Dickens C, McCabe R. Patients’ experiences of seeking help for emotional concerns in primary care: doctor as drug, detective and collaborator. BMC Fam Pract. 2020;21:35. doi: 10.1186/s12875-020-01106-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Pitcher C, Saewyc E, Browne A, Rodney P. Access to primary health care services for youth experiencing homelessness: “you shouldn’t need a health card to be healthy.” Witn Can J Crit Nurs Discourse. 2019;1(2):73-92. doi: 10.25071/2291-5796.34 [DOI] [Google Scholar]
- 36. Gilmer C, Buccieri K. Homeless patients associate clinician bias with suboptimal care for mental illness, addictions, and chronic pain. J Prim Care Community Heal. 2020;11:1-7. doi: 10.1177/2150132720910289 [DOI] [PMC free article] [PubMed] [Google Scholar]