Fig 3.
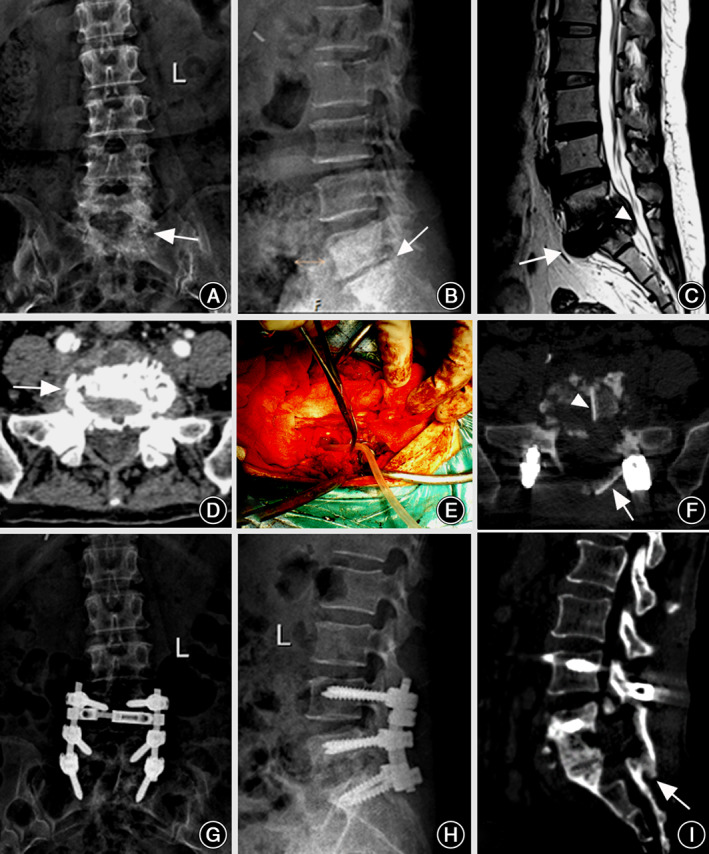
Representative case 2. A 56‐year‐old female patient with typical lumbosacral tuberculosis underwent only posterior approach for debridement, internal fixation and allogeneic bone grafting. (A) Preoperative anteroposterior X‐ray indicated the osseous sclerosis in L5 and S1 vertebral bodies (arrow). (B) Lateral X‐ray showed the collapse of L5/S1 intervertebral space, accompanied by the decrease of lumbosacral lordosis (arrow). (C) The MR sagittal imaging revealed the mild pre‐sacral cold abscess (arrow) and some necrotic disc herniates into the lumbosacral canal resulting in sciatica neuralgia (triangle). (D) The CT transverse slice showed the bony lesion on sacral sclerotic endplate (arrow). (E) A drainage tube was inserted into the wound to wash away the inflammatory mediator and puriform fluid after unilateral limited laminectomy. (F) One week later, a CT transverse slice showed the location of intervertebral bone graft (triangle) and vertebral plate bone graft (arrow). (G, H) The anteroposterior and lateral X‐rays confirmed the solidity of the internal instruments and the increase of lumbar lordosis 1 year postoperatively. (I) The intervertebral and vertebral plate bony fusions were observed in sagittal CT imaging 1 year postoperatively (arrows).
