Figure.
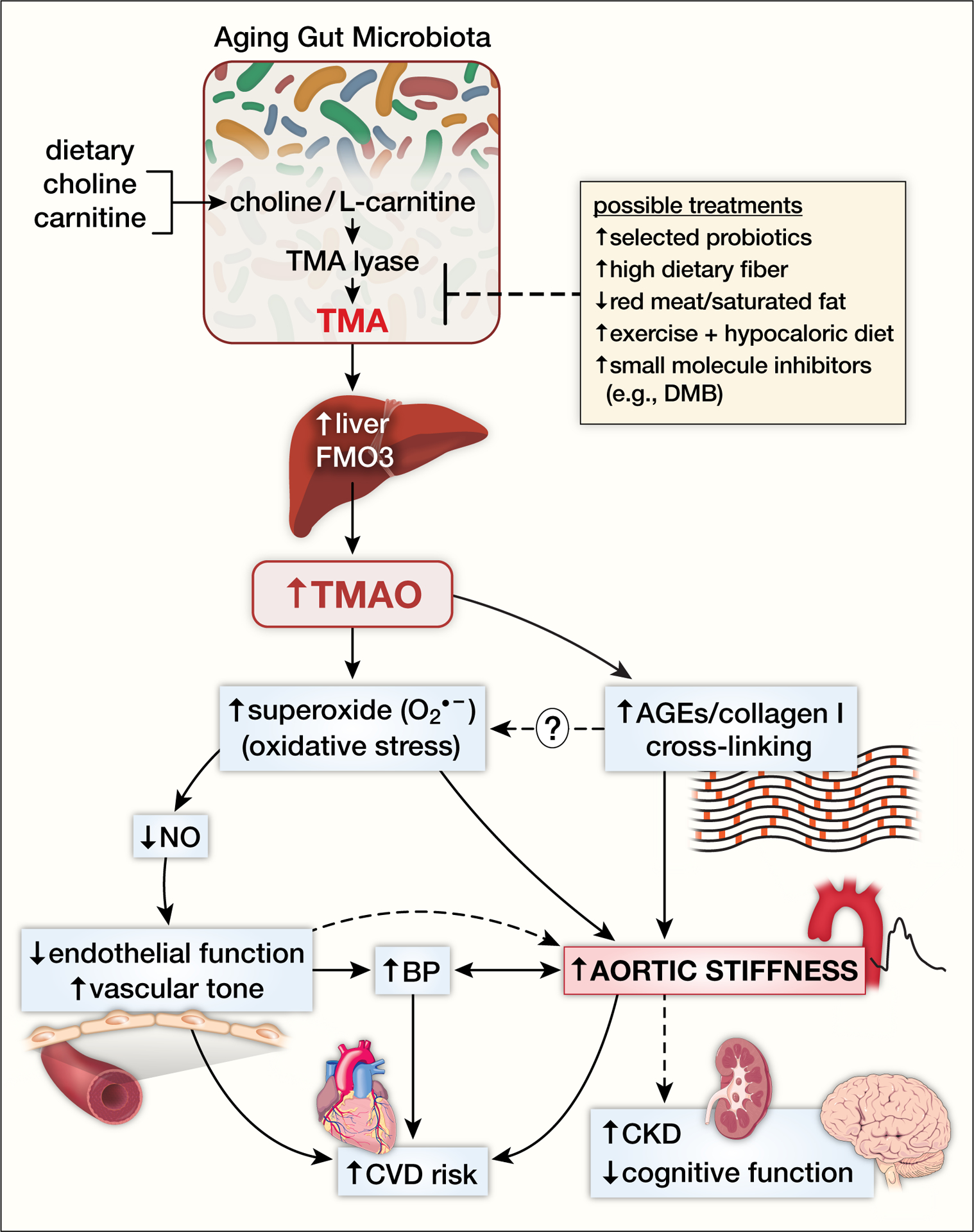
The gut-arterial axis stiffness with aging. Consumption of foods that contain choline and L-carnitine (e.g., red meat, high saturated fat dairy products) are converted to trimethylamine (TMA) by the enzyme TMA lyase by gut microbiota. TMA is released into the portal circulation where it is taken up by the liver and converted to trimethylamine N-oxide (TMAO) by the flavin containing monooxygenase (FMO) enzymes. In particular, FMO3 isoform expression is elevated in preclinical models with aging suggesting augmented conversion of TMA to TMAO. TMAO is then released from the liver into the systemic circulation where it is elevated in aged humans and increases superoxide anion-associated oxidative stress in the arterial wall leading to reductions in nitric oxide (NO)-mediated endothelial function and increases in vascular tone. TMAO-associated increased arterial oxidative stress and advanced glycation end products (AGEs) are associated with formation of cross-links between collagen and other structural proteins in the aortic wall. TMAO-related aortic stiffness is also associated with increases in blood pressure, but the causal direction of the relation is likely bidirectional. Aortic stiffness and endothelial dysfunction are associated with clinical cardiovascular disease (CVD) events in humans, and with the development of chronic kidney disease (CKD) and cognitive dysfunction with aging. Possible treatments to prevent or treat downstream effects of elevated TMAO include strategies that alter gut microbiota production of TMA including select probiotics, dietary fiber, decreased red meat/saturated fat consumption, exercise plus hypocaloric diet and novel small molecule inhibitors of gut-derived metabolites such as 3,3,-dimethyl-1-butanol (DMB).
