FIG 1.
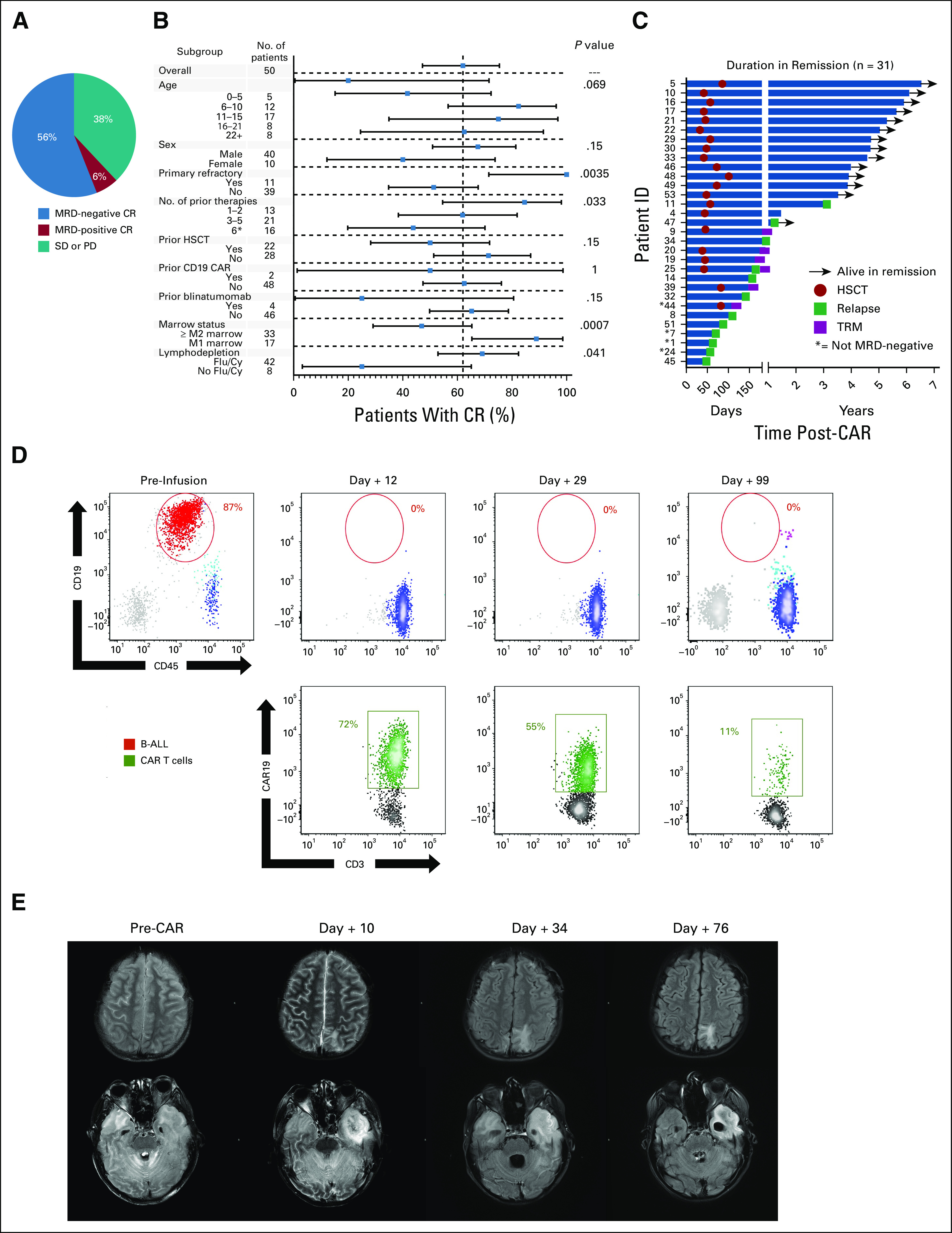
Response to CD19.28ζ CAR T-cell therapy. (A) Rate of those with MRD-positive or MRD-negative CR and those who had SD or PD among those with acute lymphoblastic leukemia. (B) Fraction of CR (MRD-positive and MRD-negative) according to patient demographics, disease characteristics, and treatment course. Squares represent the observed CR rate with the lines representing the 95% CIs for the difference of proportions from the reference category. The forest plots are based on the fraction and a Clopper-Pearson exact two-tailed 95% CI. (C) Duration in continuous remission among those who achieved a CR, indicating those who remain alive in remission, when HSCT was performed, the time of relapse, and those who experienced TRM. (D) Flow cytometric analysis of the CSF in patient 45 showing progressive CAR T-cell expansion (green) along with leukemia regression (red) in a patient with extensive CNS disease. (E) Brain magnetic resonance imaging findings from before, during, and after CAR T-cell infusion corresponding with patient 45, whose concurrent flow cytometry samples are shown in (D). Top panel (postcontrast axial fluid-attenuated inversion recovery) shows the evolution of intraparenchymal edema related to the leptomeningeal involvement to encephalomalacia. Bottom panel shows the evolution of widespread patchy white matter injury or edema involving the cerebrum and cerebellum with extensive involvement of the left temporal lobe (pretreatment). At day +10, neurologic symptoms included encephalopathy and right gaze preference. Necrosis had developed in the portion of the left temporal lobe that was most edematous. Diffusion-weighted images (not shown) demonstrated restricted diffusion corresponding to the area that is dark on fluid-attenuated inversion recovery. By day +76, the necrosis in the left temporal lobe had evolved to encephalomalacia (not ex vacuo expansion of the left temporal horn). B-ALL, B-cell acute lymphoblastic leukemia; CR, complete remission; HSCT, hematopoietic stem-cell transplant; MRD, minimal residual disease; PD, progressive disease; SD, stable disease; TRM, transplant-related mortality.
