Abstract
Background and Objectives
Diabetic ketoacidosis (DKA) rates in the United States are rising. Prior studies suggest higher rates in younger populations, but no studies have evaluated national trends in pediatric populations and differences by subgroups. As such, we sought to examine national trends in pediatric DKA.
Methods
We used the 2006, 2009, 2012, and 2016 Kids’ Inpatient Database to identify pediatric DKA admissions among a nationally representative sample of admissions of youth ≤20 years old. We estimate DKA admission per 10 000 admissions and per 10 000 population, charges, length of stay (LOS), and trends over time among all hospitalizations and by demographic subgroups. Regression models were used to evaluate differences in DKA rates within subgroups overtime.
Results
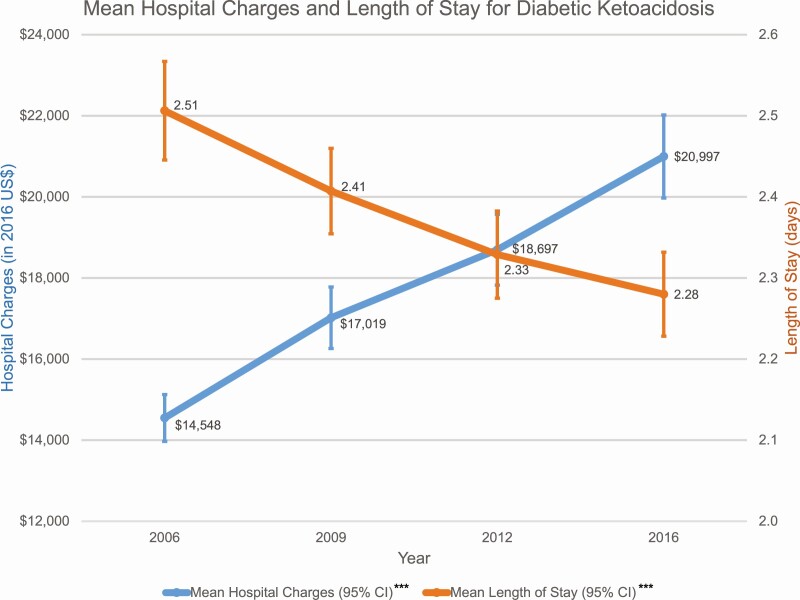
Between 2006 and 2016, there were 149 535 admissions for DKA. Unadjusted DKA rate per admission increased from 120.5 (95% CI, 115.9-125.2) in 2006 to 217.7 (95% CI, 208.3-227.5) in 2016. The mean charge per admission increased from $14 548 (95% CI, $13 971-$15 125) in 2006 to $20 997 (95% CI, $19 973-$22 022) in 2016, whereas mean LOS decreased from 2.51 (95% CI, 2.45-2.57) to 2.28 (95% CI, 2.23-2.33) days. Higher DKA rates occurred among 18- to 20-year-old females, Black youth, without private insurance, with lower incomes, and from nonurban areas. Young adults, men, those without private insurance, and from nonurban areas had greater increases in DKA rates across time.
Conclusions
Pediatric DKA admissions have risen by 40% in the United States and vulnerable subgroups remain at highest risk. Further studies should characterize the challenges experienced by these groups to inform interventions to mitigate their DKA risk and to address the rising DKA rates nationally.
Keywords: diabetic ketoacidosis, type 1 diabetes, disparities, pediatrics
Diabetic ketoacidosis (DKA) is an acute complication of diabetes associated with serious consequences, including cerebral edema and death (1). Although mortality from DKA has drastically decreased in the past century, to less than 1% in 2014 (2, 3), DKA hospitalization rates continue to rise (2, 4) despite many advances in insulin formulations and diabetes technology in recent decades.
Analysis of the National Inpatient Sample have demonstrated that younger populations with diabetes have a substantially higher rate of DKA admissions compared with older ages. Benoit et al demonstrated that those younger than 45 years old (yo) had the highest rates of DKA in 2014, with rates 8-fold higher than those between 45 and 64 yo (2). Desai et al stratified this group (age < 45 yo) even further into those 1 to 17 yo and 18 to 44 yo and found that those age 1 to 17 yo had the highest rates of DKA admissions by age per 10 000 admissions, which was 30% higher than DKA rates seen in those 18 to 44 yo in 2014 (5). These data suggest that pediatric patients with diabetes may be contributing to the rising rates of DKA admissions nationally.
Few studies have examined rates of pediatric DKA admissions, but there are several important limitations, notably the use of data from single centers, registries, or from 1 insurance provider (6-11). To address this lack of national estimates of pediatric DKA admissions, we examined data from the Kids’ Inpatient Database (KID), which is the largest all-payer pediatric inpatient care database in the United States. Our objective was to (1) describe the patient and hospital characteristics prevalent in pediatric DKA admissions nationally, (2) describe the rates and trends of DKA admissions relative to all pediatric admissions, and (3) identify subgroups of pediatric patients more likely to be admitted with DKA and evaluate whether this risk changes over time.
Methods
Study population and data elements
We used the Healthcare Cost and Utilization Project KID, developed by the Agency for Healthcare Research and Quality (12). KID is a publicly available deidentified database containing admissions from children and youth ≤ 20 yo from 42 000 hospitals across 46 states, sampled at a rate of 80% for non-newborn admissions. KID data are available every 3 years, but 2015 data were not released and instead 2016 data were released because of the transition from International Code of Diseases (ICD)-9 to ICD-10 coding. We identified admissions with a primary diagnosis of DKA in study years 2006, 2009, 2012, and 2016, using the ICD-9 and ICD-10 codes for type 1 diabetes with ketoacidosis (250.11, 250.13, E10.1, E10.11, E11.10), type 2 diabetes with ketoacidosis (250.10, 250.12 E11.1, E11.10, E11.11,) and other diabetes with ketoacidosis (249.10, 249.11, E13.1, E13.10, E13.11). KID does not allow for identification of readmissions and cannot distinguish between DKA in the setting of new-onset diabetes vs known diabetes. We classified diabetes as either type 1 or 2 using ICD coding. We excluded newborn and pregnancy-related admissions.
We evaluated hospital and patient-level variables for each admission. Patient-level variables included age, sex, race/ethnicity, admission payer, income, and urbanicity. Race/ethnicity were defined as reported by the data source (hospital) and presumed to be self-reported. Admission payers included public insurance (eg, Medicare, Medicaid), private payers (eg, private health maintenance organizations, preferred provider organizations), other (workers’ compensation, title V, Civilian Health and Medical Health and Medical Program of the Department of Veteran Affairs, or other government programs), and self-pay or no charge (eg, charity care). Median household income was reported as quartiles and was determined based on median household income per ZIP code for the calendar year. Patient location was reported per the 2010 US urban-rural classification, which defines an urbanized area as 50 000 residents or more and a nonurban area as less than 50 000 residents.
Hospital-level variables included region, ownership, and size. Region was defined as 4 geographical regions of the United States: Northeast, Midwest, South, and West. Ownership was defined as either government or private (eg, nonprofit private, private-investment). Size was characterized as small, medium, or large, based on hospital region, urbanicity, and teaching status.
Length of stay (LOS) is defined as the difference in days between the admission date and the discharge date. Total charges for the admission are reported from the hospital to KID and does not include professional fees and noncovered charges. Charges accounted for inflation using the Consumer Price Index and were reported as 2016 US dollars.
External comparison
Because overall admission rates may have changed over the study period, including because of the switch from ICD-9 to ICD-10, we used data from corresponding years of the National Health Interview Survey (NHIS) to determine population totals for those with diabetes, overall and by corresponding patient characteristics, and estimate the rate of DKA admissions per population with diabetes.
Statistical analysis
Weights provided by KID were used to generate nationally representative estimates of hospitalizations and all analyses accounted for the stratified sampling design. We used descriptive statistics to describe the weighted frequency of DKA admissions and the rate of DKA admissions per 10 000 pediatric admissions by patient-level and hospital-level characteristics. The weighted frequency and rate of DKA admissions were also stratified by year to investigate unadjusted trends over time (Appendix 1) (13). Charges and LOS were compared across years.
Multivariable logistic regression was used to evaluate the adjusted odds of DKA admission compared with all other pediatric admissions by patient-level and hospital-level factors in KID and to evaluate the adjusted odds of any overnight hospitalization for the US pediatric population in the NHIS. Multivariate logistic regression with interaction terms between hypothesized modifying factors and year were used to evaluate differences in trends of DKA admissions over time; adjusted marginal probabilities were output from these models to calculate adjusted DKA prevalence and rates (Appendix 2 and 3) (13), and to visualize differing trends by patient-level and hospital-level characteristics (13). KID models were adjusted for year, age, sex, race/ethnicity, payer, urbanicity, income, region, hospital ownership, and bed size; NHIS models adjusted for year, age, sex, race/ethnicity, payer, income, and region. All analyses were performed with Stata version 15.1 (StataCorp, College Station, TX). This study was institutional review board exempt because it was a secondary analysis of preexisting and deidentified data (12). This report follows the Strengthening the Reporting of Observational Studies in Epidemiology reporting guidelines for cross-sectional studies.
Results
We identified 149 535 DKA admissions; the majority were among those with type 1 diabetes (95.0%), ages 18 to 20 (37.3%), females (53.7%), White non-Hispanic (49.5%), publicly insured (44.05), from urban areas (80.8%), and in the lowest income quartile (32.2%; Table 1). Most admissions were to large (60.1%), private hospitals (71.3%), and Southern states (40.0%). There were 151.01 (95% CI, 147.1-155.0) DKA admissions per 10 000 pediatric admissions and 1547.3 (95%CI, 1434.7-1660.0) per 10 000 population from 2006 through 2016. The unadjusted rate of DKA admissions increased over time from 120.5 (95% CI, 115.9-125.2) in 2006, to 128.6 (95% CI, 123.4-134.1) in 2009, 151.8 (95% CI, 145.7-158.0) in 2012, and 217.7 (95% CI, 208.3-227.5) in 2016; DKA rate per population also increased over time. Mean charge significantly increased over time from $14 458 (95% CI, $13 971-$15 125) in 2006 to $20 997 (95% CI, $19 973-$22 022) in 2016, whereas LOS significantly decreased from 2.51 (95% CI, 2.45-2.57) days to 2.28 (95% CI, 2.23-2.33) days (Fig. 1).
Table 1.
Prevalence and rate of diabetic ketoacidosis (DKA) by patient and hospital characteristics in the US pediatric population
| N (%), DKA admissions | Rate per 10 000 admissions (95% CI) | P value | Rate per 10 000 youth with diabetes (95% CI) | |
|---|---|---|---|---|
| Total | 149 535 (100) | 151.0 (147.1-155.0) | 1547.3 (1434.7-1660.0) | |
| Admissions by type | ||||
| Type 1 diabetes | 142 112 (95.0) | -- | -- | |
| Type 2 diabetes | 7422 (5.0) | -- | -- | |
| Age, y | <0.0001 | |||
| 0-2 | 4036 (2.7) | 10.9 (10.2-11.6) | 4859.5 (2424.8-7294.2) | |
| 3-5 | 4914 (3.3) | 55.7 (52.7-58.9) | 1497.4 (1110.2-1884.6) | |
| 6-8 | 9856 (6.6) | 120.1 (114.3-126.2) | 1426.3 (1109.4-1743.3) | |
| 9-11 | 15 760 (10.5) | 243.7 (233.2-254.7) | 1966.2 (1241.7-2690.7 | |
| 12-14 | 28 200 (18.9) | 285.5 (273.5-298.1) | 1600.9 (1326.6-1875.3) | |
| 15-17 | 30 356 (20.3) | 230.5 (221.7-239.7) | 1373.1 (1157.1-1589.1) | |
| 18-20 | 55 788 (37.3) | 371.4 (363.1-379.8) | 1472.8 (1270.5-1675.1) | |
| Unknown | 624 (0.4) | 129.5 (111.2-150.8) | -- | |
| Sex | <0.0001 | |||
| Male | 68 325 (45.7) | 129.2 (125.6-133.1) | 1423.6 (1256.7-1590.6) | |
| Female | 80 335 (53.7) | 176.9 (172.3-181.6) | 1651.4 (1451.2-1851.7) | |
| Unknown | 875 (0.6) | 118.5 (99.7-140.7) | -- | |
| Race/ethnicity | <0.0001 | |||
| White | 74 041 (49.5) | 170.1 (165.2-175.2) | 1269.0 (1136.0-1401.9) | |
| Black | 27 616 (18.5) | 188.1 (180.9-195.5) | 1815.8 (1448.1-2183.5) | |
| Hispanic | 18 415 (12.3) | 102.6 (97.7-107.8) | 1120.6 (926.7-1314.5) | |
| Asian or Pacific Islander | 1554 (1.0) | 67.7 (60.3-74.6) | 789.3 (140.8-1437.7) | |
| Native American | 1052 (0.7) | 134.0 (117.8-152.5) | 659.3 (504.8-813.8) | |
| Other | 4924 (3.3) | 108.3 (101.7-115.3) | 1595.1 (1064.1-2126.0) | |
| Unknown | 21 932 (14.7) | 144.1 (134.8-153.9) | -- | |
| Payer | <0.0001 | |||
| Private | 63 240 (42.3) | 148.8 (144.2-153.6) | 1345.9 (1188.6-1503.2) | |
| Public | 65 768 (44.0) | 139.6 (135.3-144.1) | 1773.5 (1561.1-1985.9) | |
| Self-pay or no charge | 11 825 (7.9) | 248.5 (237.8-259.5) | 1532.7 (1240.2-1825.1) | |
| Other | 8438 (5.6) | 188.2 (175.7-201.5) | 1984.5 (1551.7-2417.3) | |
| Unknown | 264 (0.2) | 142.9 (104.9-194.5) | -- | |
| Urbanicity | <0.0001 | |||
| Nonurban | 27 919 (18.7) | 174.0 (168.2-180.0) | -- | |
| Urban | 120 757 (80.8) | 147.4 (143.3-151.6) | -- | |
| Unknown | 859 (0.6) | 82.4 (70.9-95.8) | -- | |
| Household income | <0.0001 | |||
| Quartile 1 (lowest) | 48 095 (32.2) | 156.7 (151.6-162.0) | 1520.7 (1307.8-1733.6) | |
| Quartile 2 | 38 943 (26.0) | 162.1 (157.5-166.9) | 1506.9 (1278.5-1735.2) | |
| Quartile 3 | 34 095 (22.8) | 152.9 (148.0-158.0) | 1562.1 (1234.5-1889.7) | |
| Quartile 4 (highest) | 25 614 (17.1) | 129.5 (123.8-135.5) | 1476.9 (1280.4-1673.3) | |
| Unknown | 2788 (1.9) | 124.3 (114.5-134.9) | -- | |
| Hospital region | <0.0001 | |||
| Northeast | 21 079 (14.1) | 114.5 (107.2-122.5) | 1449.6 (1181.2-1718.1) | |
| Midwest | 36 374 (24.3) | 163.4 (155.0-172.3) | 1607.7 (1394.2-1821.3) | |
| South | 59 829 (40.0) | 161.2 (154.8-167.9) | 1561.0 (1371.2-1750.8) | |
| West | 32 253 (21.6) | 151.8 (142.9-161.2) | 1525.2 (1229.2-1821.2) | |
| Hospital ownership | <0.0001 | |||
| Government | 16 851 (11.3) | 163.8 (154.0-174.2) | -- | |
| Private | 106 561 (71.3) | 160.0 (155.4-164.6) | -- | |
| Unknown | 26 123 (17.5) | 118.1 (112.1-124.5) | -- | |
| Hospital size by bed number | 0.0331 | |||
| Small | 18 846 (12.6) | 163.9 (151.4-177.5) | -- | |
| Medium | 36 642 (24.5) | 155.1 (146.6-164.2) | -- | |
| Large | 89 811 (60.1) | 147.4 (142.8-152.2) | -- | |
| Unknown | 4236 (2.8) | 142.0 (125.6-160.6) | -- | |
| Year | <0.0001 | |||
| 2006 | 32 612 (21.8) | 120.5 (115.9-125.2) | 1349.8 (1212.5-1487.2) | |
| 2009 | 34 473 (23.1) | 128.6 (123.4-134.0) | 1426.9 (1288.1-1565.6) | |
| 2012 | 36 444 (24.4) | 151.8 (145.7-158.1) | 1508.4 (1355.9-1661.0) | |
| 2016 | 46 006 (30.8) | 217.7 (208.3-227.5) | 1904.2 (1691.9-2116.6) |
Weighted frequency counts of DKA admissions across all years (2006, 2009, 2012, 2016 Kid’s Inpatient Database) are shown; weighted column percentages reflect the prevalence of each characteristic among all DKA admissions. Two average annual DKA rates are shown. The first indicates the unadjusted number of DKA admissions per 10 000 pediatric admissions (for all causes) by characteristics included in the Kid’s Inpatient Database. The second indicates the unadjusted number of DKA admissions per 10 000 US youth with diabetes by characteristics included in the National Health Interview Survey.
Figure 1.
Mean hospital charges and length of stay for diabetic ketoacidosis. Unadjusted mean (95% CI) hospital charges in 2016 US dollars and mean (95% CI) length of stay for diabetic ketoacidosis admissions by year, using the Kid’s Inpatient Database. ***Statistical significance <0.001 in the P value for trend across years.
Adjusted DKA rates by patient characteristics
The highest unadjusted rates of DKA per admissions were for those ages 18 to 20 (371.4; 95% CI, 363.1-379.8), females (176.9; 95% CI, 172.3-181.6), Black non-Hispanic (188.1; 95% CI, 181.0-195.5), self-pay or no charge (248.5; 95% CI, 237.8-259.5), and from nonurban areas (174.0; 95% CI, 168.2-180.0; Table 1). Notably, although Native Americans had a low overall prevalence amongst those with DKA (0.7%), they had the third highest rate of DKA by reported race (134.0; 95% CI, 117.8-152.5). Similar elevation in DKA rates per population were seen by age, sex, and race/ethnicity, whereas those with public or other insurance and of lowest income had the highest unadjusted rates of DKA per population.
Overall, odds of DKA significantly increased with age, decreased with higher income, increased for females compared with males (OR:1.25, 95% CI, 1.23–1.27), Black compared to white youth (odds ratio [OR]: 1.08; 95% CI, 1.04-1.12), those without private insurance compared to with, and for those in nonurban compared with urban areas (OR: 1.13; 95% CI, 1.09-1.17; Table 2).
Table 2.
Adjusted odds ratios for diabetic ketoacidosis (DKA) Admissions
| Adjusted OR (95% CI) for DKA vs other admission | P value | Adjusted OR (95% CI) for hospitalized vs not | P value | |
|---|---|---|---|---|
| Age, y | ||||
| 0-2 | 0.19 (0.18-0.21) | <0.001 | 11.26 (0.66-193.09) | 0.095 |
| 3-5 | 1.00 (reference) | 1.00 (reference) | ||
| 6-8 | 2.18 (2.07-2.29) | <0.001 | 1.44 (0.18-11.58) | 0.733 |
| 9-11 | 4.49 (4.28-4.70) | <0.001 | 0.59 (0.08-4.57) | 0.613 |
| 12-14 | 5.16 (4.90-5.44) | <0.001 | 0.61 (0.09-4.15) | 0.610 |
| 15-17 | 4.14 (3.93-4.37) | <0.001 | 1.04 (0.16-6.83) | 0.964 |
| 18-20 | 6.64 (6.29-7.02) | <0.001 | 1.10 (0.14-8.86) | 0.928 |
| Unknown | 3.13 (2.63-3.72) | <0.001 | -- | |
| Sex | ||||
| Male | 1.00 (reference) | 1.00 (reference) | ||
| Female | 1.25 (1.23-1.27) | <0.001 | 1.12 (0.57-2.18) | 0.750 |
| Unknown | 0.67 (0.55-0.82) | <0.001 | -- | |
| Race/ethnicity | ||||
| White | 1.00 (reference) | 1.00 (reference) | ||
| Black | 1.08 (1.04-1.12) | <0.001 | 0.24 (0.08-0.71) | 0.010 |
| Hispanic | 0.67 (0.64-0.70) | <0.001 | 0.89 (0.36-2.21) | 0.801 |
| Asian or Pacific Islander | 0.50 (0.45-0.55) | <0.001 | 0.33 (0.07-1.49) | 0.148 |
| Native American | 0.74 (0.65-0.85) | <0.001 | 0.06 (0.01-0.78) | 0.032 |
| Other | 0.80 (0.75-0.85) | <0.001 | 2.66 (0.62-11.31) | 0.186 |
| Unknown | 0.97 (0.91-1.04) | 0.397 | -- | |
| Payer | ||||
| Private | 1.00 (reference) | 1.00 (reference) | ||
| Public | 1.17 (1.14-1.20) | <0.001 | 0.56 (0.19-1.66) | 0.293 |
| Self-pay or no charge | 1.33 (1.28-1.38) | <0.001 | 1.20 (0.20-7.07) | 0.842 |
| Other | 1.16 (1.08-1.23) | <0.001 | 1.46 (0.20-10.82) | 0.714 |
| Unknown | 0.81 (0.56-1.16) | 0.241 | -- | |
| Urbanicity | ||||
| Nonurban | 1.13 (1.09-1.17) | <0.001 | -- | |
| Urban | 1.00 (reference) | -- | ||
| Unknown | 0.67 (0.56-0.80) | <0.001 | -- | |
| Household income | ||||
| Quartile 1 (lowest) | 1.25 (1.19-1.31) | <0.001 | 1.36 (0.45-4.10) | 0.584 |
| Quartile 2 | 1.26 (1.21-1.32) | <0.001 | 0.83 (0.21-3.27) | 0.793 |
| Quartile 3 | 1.19 (1.14-1.23) | <0.001 | 0.76 (0.26-2.21) | 0.613 |
| Quartile 4 (highest) | 1.00 (reference) | 1.00 (reference) | ||
| Unknown | 1.07 (0.99-1.17) | <0.001 | -- | |
| Hospital region | ||||
| Northeast | 1.00 (reference) | 1.00 (reference) | ||
| Midwest | 1.29 (1.19-1.40) | <0.001 | 1.10 (0.35-3.41) | 0.871 |
| South | 1.39 (1.29-1.50) | <0.001 | 1.43 (0.51-4.06) | 0.498 |
| West | 1.56 (1.45-1.69) | <0.001 | 1.26 (0.40-4.00) | 0.697 |
| Hospital ownership | ||||
| Government | 0.94 (0.88-1.01) | 0.094 | -- | |
| Private | 1.00 (reference) | -- | ||
| Unknown | 0.95 (0.87-1.04) | 0.230 | -- | |
| Hospital size by bed number | ||||
| Small | 1.16 (1.08-1.24) | <0.001 | -- | |
| Medium | 1.11 (1.05-1.17) | <0.001 | -- | |
| Large | 1.00 (reference) | -- | ||
| Unknown | 1.36 (1.13-1.64) | 0.001 | -- | |
| Year | ||||
| 2006 | 1.00 (reference) | 1.00 (reference) | ||
| 2009 | 1.00 (0.93-1.07) | 0.998 | 1.37 (0.47-3.98) | 0.561 |
| 2012 | 1.16 (1.07-1.25) | <0.001 | 1.14 (0.44-2.93) | 0.791 |
| 2016 | 1.63 (1.50-1.76) | <0.001 | 0.93 (0.37-2.36) | 0.882 |
Table shows adjusted odds ratios for DKA vs non-DKA admission using the Kid’s Inpatient Database and adjusted odds ratios for any overnight hospitalization vs none using the National Health Interview Survey. For both analyses, results are adjusted for all other variables listed in the table column. The regression for hospitalized or not is underpowered, so please interpret with caution.
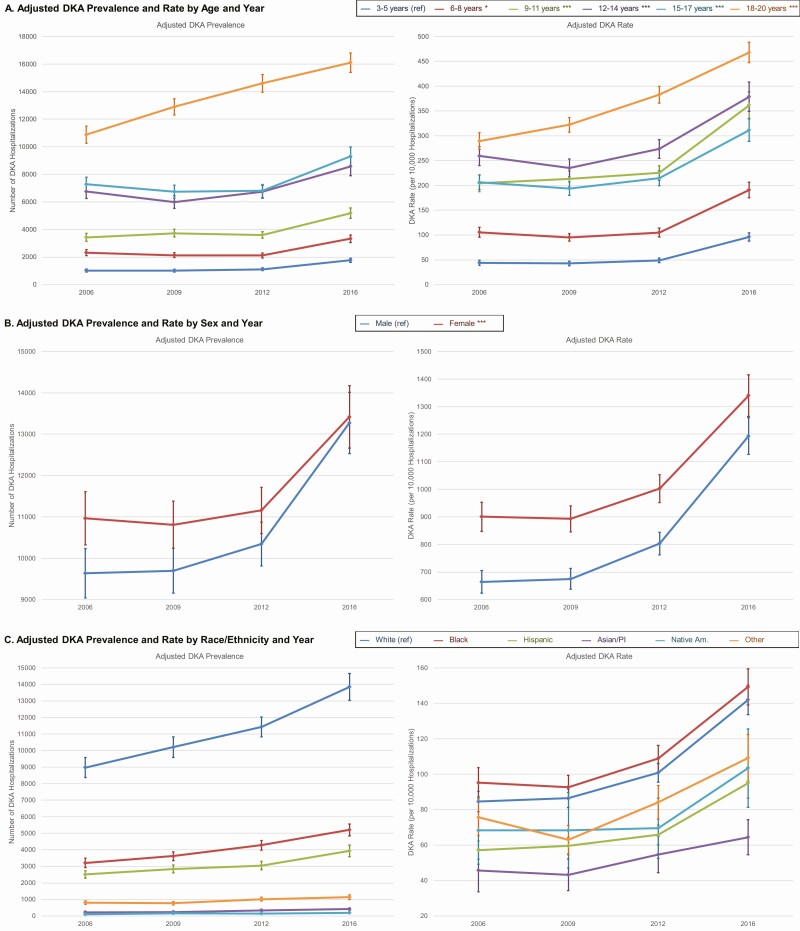
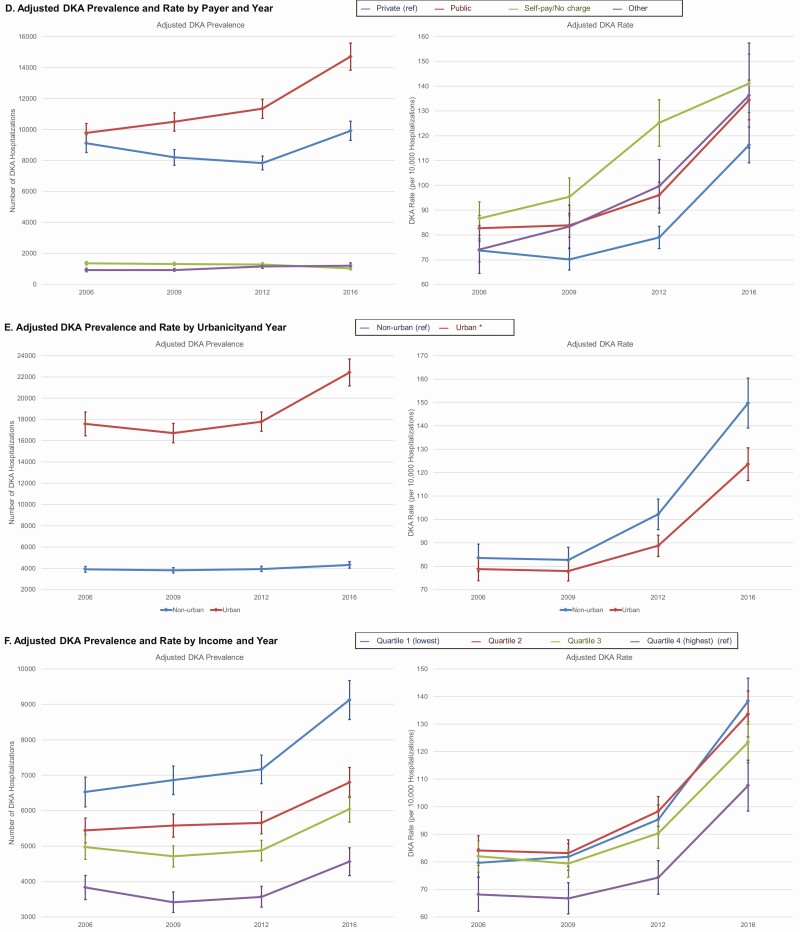
Although all age groups experienced a rise in adjusted DKA rates over time, the greatest and earliest absolute change in DKA rates occurred in those 18 to 20 yo (Fig. 2). Females continued to have higher DKA rates at all time points but the difference between sex diminished over time because males experienced a greater increase in DKA than females. Compared with those privately insured, those without private insurance had a greater rise in adjusted DKA rates in 2009 and 2012 but a similar increase in 2016. Those in nonurban areas experienced a greater increase in adjusted DKA rates over time compared with those in urban areas. DKA trends were similar across race/ethnicity and income.
Figure 2.
Adjusted diabetic ketoacidosis prevalence and rate by year and patient characteristics. Figures show adjusted marginal prevalence (left) and adjusted marginal rate (right) of diabetic ketoacidosis (DKA) admissions and associated 95% CIs by patient characteristics and year. Marginal probabilities were output from multivariate models that included interactions between each characteristic and year, and that were adjusted for age, sex, race/ethnicity, payer, urbanicity, income, region, hospital ownership, and hospital bed size. Marginal probabilities were applied to observed hospitalization totals to estimate adjusted prevalence of DKA admissions and were applied to a hypothetical population of 10 000 admissions to estimate adjusted rate of DKA admissions. Not all covariate subgroups are shown. Adjusted annual trend was statistically significant for all subgroups at P < 0.01. Statistically significant differences in the annual trend between subgroups relative to the reference (ref) subgroup (ie, interaction) is noted by asterisks in the legend; *P < 0.05, **P < 0.01, and ***P < 0.001.
Adjusted DKA rates by hospital characteristics
The highest unadjusted rates of DKA per admissions were from small hospitals (163.9; 95% CI, 151.4-177.5) and those in the Midwest (163.4; 95% CI, 1550.0-172.3; Table 1). Odds of DKA significantly increased as bed size decreased and were elevated for all regions compared with the Northeast (Table 2). The rise in adjusted DKA rates over time were similar across hospital size, ownership, and region (Appendix 4) (13).
Discussion
Despite a decline in total pediatric admissions in this nationally representative sample, we found that the prevalence and rate of DKA admissions have significantly increased from 2006 to 2016. Several subgroups were identified with higher risk of DKA admission overall and a greater increase in DKA admission rate over time. Given these trends and observed disparities, careful consideration is needed to determine the probable mechanisms, ultimately to advise appropriate clinical interventions.
The rising prevalence and incidence of type 1 diabetes likely contributes to rising DKA rates (14, 15), but the relative impact of prevalent vs incident cases is less clear. Studies that have evaluated trends in DKA at diagnosis in the United States have shown conflicting results (16-21). Because we know that there are approximately 18 000 new cases of diabetes per year (22), of which about 30% present with DKA at diagnosis (16), we do not suspect that the increase in DKA rates over time are primarily driven by the potential increase in incidence of DKA at diabetes diagnosis because these admissions likely represent a small portion of DKA in our study (~14%).
We found that adolescents and young adults had the highest DKA admission rates, consistent with previous findings (6, 9) because this peak in late teenage years also corresponds with the worsened glycemic control typically documented in this age group (23). In our study, young adults also show the largest rise in DKA admissions over time. This may reflect vulnerability during transitions from pediatric to adult care and/or a period of substantial life changes overall that can lead to gaps in outpatient care and increase risk of acute complications (24).
Consistent with prior literature, our findings demonstrate a higher prevalence of DKA admissions in females compared with males with existing diabetes (6-8, 11, 17, 25, 26), although our study is first to demonstrate higher rate of increase over time in males. Higher rates in females may reflect psychosocial challenges that are more predominant in females, including higher rates of depressive symptoms and struggles with body image (sometimes resulting in omission of insulin) (27). These conditions are both associated with poor glycemic control and diabetes-related complications (27); thus, higher DKA rates in females may be a consequence of unaddressed yet prevalent psychosocial barriers experienced by this population.
Our findings demonstrate that DKA rates are higher in Black youth when compared with Whites, consistent with other pediatric studies that found those of Black race have higher risk of DKA both at diagnosis of diabetes and with existing diabetes compared with other races (6, 9, 28). Unlike previous studies, we had the ability to evaluate national DKA rates among Native American youth. Notably, despite representing the lowest prevalence amongst those admitted for DKA, Native American youth had the highest rates of DKA admission by race after White and Black youth. Social disadvantage is thought to be a major mediator of poor diabetes outcomes seen in racial/ethnic minorities and is associated with several factors that influence clinical outcomes, including timeliness of diabetes diagnosis, diabetes self-management practices, access to care, and psychosocial well-being (28-33). Although we controlled for median neighborhood income, this proxy for individual socioeconomic status is unlikely to capture the complexity of social disadvantage that could explain observed disparities and so observed racial/ethnic differences may reflect unmeasured social disadvantage rather than an inherent predisposition for DKA.
We found that income quartile and admission payer were 2 of the strongest patient factors associated with DKA admission after age. The majority of DKA admissions were in patients with public insurance, with correspondingly high per population rates of DKA, but when compared with all admissions, the highest rates were among those with self-pay or no charge (presumably uninsured). Uninsured youth may have higher rates per admission because although hospitalization may be avoided for more minor conditions, the severity of DKA and its life-threatening nature would likely oblige admission despite hesitations that can arise from lack of insurance and the threat of high out-of-pocket health care costs (34). This likely contributes to DKA, not only in those with existing diabetes, but also in those with newly diagnosed diabetes because these hesitations to pursue care may result in a delay of diagnosis, which is a predictor of DKA at diabetes onset (28, 35). Regardless of payer, the risk of DKA admission was elevated for all lower income groups compared with the highest income quartile, which may reflect economic barriers to access to care, effective self-management, and medication adherence (28, 36, 37). In patients with existing diabetes, the dramatic rise in the price of insulin in the United States over the past few decades (38) has been implicated as a cause of insulin rationing, poor glycemic control, DKA, and even death (36, 39, 40). Although the implications of rising insulin costs for adults with diabetes have been studied, lower income families may also face high financial burden from their child’s insulin and experience similar consequences.
The rise in charges for DKA admission (even after accounting for inflation) may reflect the rise in general health care costs in the United States, including costs associated with diabetes management (41-44). These rising cost often result in increased out-of-pocket cost for patients with diabetes, even for those with private insurance (38). Although those in the highest income quartile may not be strongly affected by these rising out-of-pocket costs, those in lower income quartiles, especially those who are underinsured, maybe more sensitive to small changes in out-of-pocket cost (34, 45). If high financial burden associated with routine diabetes management indeed contributes to an increase in pediatric DKA admissions, then the increasing charges associated with such admissions are particularly concerning because they may compound financial hardship for already vulnerable families. Despite the rise in charges, length of stay decreased. This may be due to premature discharge in attempts to mitigate cost or reflective of more efficient DKA management facilitated by the widely growing adoption of DKA management protocols (46, 47). Future work is needed to understand contributors to high admission charges, despite more efficient DKA management during admissions, to inform system and policy interventions to mitigate the financial burden passed to families with a child hospitalized for DKA.
We found that smaller hospitals outside the Northeast had the highest rates of DKA admission. This may be related to the concentration of large tertiary medical care centers located in the Northeast, which often have greater experience diagnosing and managing relatively rare medical conditions, thus DKA admissions may comprise a lower share of their total admissions and they may be also better equipped with resources to provide more comprehensive and timely outpatient care that may in turn reduce DKA risk and the need for inpatient services.
The limitations of this study include potential misclassification of diabetes diagnosis or DKA given this was a claims-based analysis. There may also be inaccuracies in the race and ethnicity classification. We also were unable to account for changes in coding practices in the setting of the ICD-9 to ICD-10 transition, which may have affected case detection of DKA admissions, and likely accounts for some of the relatively larger increase in DKA rate seen between 2012 and 2016 (48). However, given the significant rise in DKA admissions also seen before 2016, it is likely that at least some of this trend is unrelated to the ICD switch. Although we were able to quantify DKA admissions as a whole, the KID dataset does not distinguish admissions from readmissions. We can estimate based on other studies (7, 49), that approximately 20% of the admissions described may represent readmissions. Lastly, we do not know which admissions were associated with a new diagnosis of diabetes vs an admission for DKA in a patient with established disease. As previously discussed, we do not suspect that DKA at diagnosis is the primary driver of the rise in DKA admissions because these admissions likely only represent 14% of all DKA admissions in our study.
Despite these limitations, our study captures the most recent estimate of pediatric DKA admissions nationally, and, to our knowledge, is the largest and most comprehensive analysis of pediatric DKA admissions. Because we have a representative sample from 46 states, we were also able to evaluate subgroups not sufficiently represented by other datasets, including Native Americans (for whom there is a dearth of studies describing DKA rates). The majority of DKA studies do not report any rates of DKA among Native Americans, and the studies that do so often have fewer than 75 participants in this subgroup (2, 5, 6, 9, 16, 17, 50). At more than 1000 admissions among Native American youth, our study captures the largest number of DKA events in this population while also quantifying trends in admissions in this group over time. Finally, unlike most published studies evaluating DKA admissions, our study sampled DKA admissions from hospitals across the nation and so was able to evaluate DKA rates by hospital factors (eg, hospital size, region, ownership) in addition to patient factors.
Conclusions
The number of pediatric admissions for DKA in the United States have increased from 2006 to 2016. Certain patient-level and hospital-level characteristics are associated with higher rates of admissions including young adults (18-20 yo), females, Black youth, those with no or public insurance, of low socioeconomic status, from nonurban areas, and those cared for at smaller hospitals. Further studies are needed to evaluate the role of other factors such as the rise in diabetes technology use (51) on changes in DKA rates over time. Additional studies are also needed to better understand the specific barriers, especially those relating to psychosocial and financial burden that may be avertable, and how they drive the heighted risk for DKA in these populations. This will be critical to determine what clinical interventions, models of care, and policies may be most appropriate to mitigate the rising DKA rates in patients most vulnerable to experiencing poor short-term and long-term clinical outcomes.
Acknowledgments
Financial Support: The authors wish to acknowledge the generous funding support from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) K01DK116932 (principal investigator: L. E. W.). T. M. also receives support from the Department of Veterans Affairs (under QUE15-272, QUE15-286, and CSP2002), from the NIDDK of the National Institutes of Health under grant R18DK105464, the Centers for Disease Control and Prevention (CDC) under grant U18DP006535, from the Patient-Centered Outcomes Research Institute (PCORI) under grant SDM-2018C2-13543, and from the University of California at Los Angeles (UCLA). The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author Contributions: E. M. E. conceptualized and designed the study, analyzed and interpreted the data, drafted the initial manuscript, and reviewed and revised the manuscript. T. P. C. analyzed and interpreted the data and reviewed and revised the manuscript. T. M. conceptualized and designed the study and reviewed and revised the manuscript. L. E. W. conceptualized and designed the study, analyzed and interpreted that data, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Glossary
Abbreviations
- DKA
diabetic ketoacidosis
- ICD
International Code of Diseases
- KID
Kids’ Inpatient Database
- LOS
length of stay
- NHIS
National Health Interview Survey
- yo
years old
Additional Information
Disclosures: The authors have no relevant conflict of interests, including specific financial interests, relationships, and affiliations relevant to the subject of this manuscript to disclose.
Data Availability
Some or all data generated or analyzed during this study are included in this published article or in the data repositories listed in the References.
References
- 1. Dhatariya KK, Glaser NS, Codner E, Umpierrez GE. Diabetic ketoacidosis. Nat Rev Dis Primers. 2020;6(1):40. [DOI] [PubMed] [Google Scholar]
- 2. Benoit SR, Zhang Y, Geiss LS, Gregg EW, Albright A. Trends in diabetic ketoacidosis hospitalizations and in-hospital mortality—United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2018;67(12):362-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Liu CC, Chen KR, Chen HF, Huang HL, Ko MC, Li CY. Trends in hospitalization for diabetic ketoacidosis in diabetic patients in Taiwan: analysis of national claims data, 1997–2005. J Formos Med Assoc. 2010;109(10):725-734. [DOI] [PubMed] [Google Scholar]
- 4. Zhong VW, Juhaeri J, Mayer-Davis EJ. Trends in hospital admission for diabetic ketoacidosis in adults with type 1 and type 2 diabetes in England, 1998–2013: a retrospective cohort study. Diabetes Care. 2018;41(9):1870-1877. [DOI] [PubMed] [Google Scholar]
- 5. Desai D, Mehta D, Mathias P, Menon G, Schubart UK. Health care utilization and burden of diabetic ketoacidosis in the U.S. over the past decade: a nationwide analysis. Diabetes Care. 2018;41(8):1631-1638. [DOI] [PubMed] [Google Scholar]
- 6. Cengiz E, Xing D, Wong JC, et al. ; T1D Exchange Clinic Network . Severe hypoglycemia and diabetic ketoacidosis among youth with type 1 diabetes in the T1D Exchange clinic registry. Pediatr Diabetes. 2013;14(6):447-454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Everett E, Mathioudakis N. Association of area deprivation and diabetic ketoacidosis readmissions: comparative risk analysis of adults vs children with type 1 diabetes. J Clin Endocrinol Metab. 2019;104(8):3473-3480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Maahs DM, Hermann JM, Holman N, et al. ; National Paediatric Diabetes Audit and the Royal College of Paediatrics and Child Health, the DPV Initiative, and the T1D Exchange Clinic Network . Rates of diabetic ketoacidosis: international comparison with 49 859 pediatric patients with type 1 diabetes from England, Wales, the U.S., Austria, and Germany. Diabetes Care. 2015;38(10):1876-1882. [DOI] [PubMed] [Google Scholar]
- 9. Malik FS, Hall M, Mangione-Smith R, et al. . Patient characteristics associated with differences in admission frequency for diabetic ketoacidosis in united states children’s hospitals. J Pediatr. 2016;171:104-110. [DOI] [PubMed] [Google Scholar]
- 10. Rewers A, Chase HP, Mackenzie T, et al. . Predictors of acute complications in children with type 1 diabetes. Jama. 2002;287(19):2511-2518. [DOI] [PubMed] [Google Scholar]
- 11. Shrestha SS, Zhang P, Barker L, Imperatore G. Medical expenditures associated with diabetes acute complications in privately insured U.S. youth. Diabetes Care. 2010;33(12):2617-2622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. HCUP- KID Overview. Agency for Healthcare Research and Quality. Accessed May 29, 2020. https://www.hcup-us.ahrq.gov/kidoverview.jsp
- 13. Everett E, Copeland T, Moin T, Wisk LE. National trends in pediatric admissions for diabetic ketoacidosis, 2006–2016 (appendix). Accessed January 12, 2021. doi: 10.6084/m9.figshare.13565060 [DOI] [PMC free article] [PubMed]
- 14. Dabelea D, Mayer-Davis EJ, Saydah S, et al. . Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA. 2014;311(17):1778-1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rogers MAM, Kim C, Banerjee T, Lee JM. Fluctuations in the incidence of type 1 diabetes in the United States from 2001 to 2015: a longitudinal study. BMC Med. 2017;15(1):199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dabelea D, Rewers A, Stafford JM, et al. ; SEARCH for Diabetes in Youth Study Group . Trends in the prevalence of ketoacidosis at diabetes diagnosis: the SEARCH for diabetes in youth study. Pediatrics. 2014;133(4):e938-e945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rewers A, Klingensmith G, Davis C, et al. . Presence of diabetic ketoacidosis at diagnosis of diabetes mellitus in youth: the Search for Diabetes in Youth Study. Pediatrics. 2008;121(5): e1258-e1266. [DOI] [PubMed] [Google Scholar]
- 18. Schober E, Rami B, Waldhoer T, Austrian Diabetes Incidence Study Group . Diabetic ketoacidosis at diagnosis in Austrian children in 1989–2008: a population-based analysis. Diabetologia. 2010;53(6):1057-1061. [DOI] [PubMed] [Google Scholar]
- 19. Cherubini V, Grimsmann JM, Åkesson K, et al. . Temporal trends in diabetic ketoacidosis at diagnosis of paediatric type 1 diabetes between 2006 and 2016: results from 13 countries in three continents. Diabetologia. 2020;63(8). doi: 10.1007/s00125-020-05152-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Todd Alonso G, Coakley A, Pyle L, Manseau K, Thomas S, Rewers A. Diabetic ketoacidosis at diagnosis of type 1 diabetes in Colorado children, 2010–2017. Diabetes Care. 2020;43(1). doi: 10.2337/dc19-0428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mencher SR, Frank G, Fishbein J. Diabetic ketoacidosis at onset of type 1 diabetes: rates and risk factors today to 15 years ago. Glob Pediatr Health. 2019;6. doi: 10.1177/2333794X19870394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hamman RF, Bell RA, Dabelea D, et al. . The SEARCH for diabetes in youth study: rationale, findings, and future directions. Diabetes Care. 2014;37(12). doi: 10.2337/dc14-0574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Miller KM, Foster NC, Beck RW, et al. ; T1D Exchange Clinic Network . Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D Exchange clinic registry. Diabetes Care. 2015;38(6):971-978. [DOI] [PubMed] [Google Scholar]
- 24. Peters A, Laffel L; American Diabetes Association Transitions Working Group . Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems: a position statement of the American Diabetes Association, with representation by the American College of Osteopathic Family Physicians, the American Academy of Pediatrics, the American Association of Clinical Endocrinologists, the American Osteopathic Association, the Centers for Disease Control and Prevention, Children with Diabetes, The Endocrine Society, the International Society for Pediatric and Adolescent Diabetes, Juvenile Diabetes Research Foundation International, the National Diabetes Education Program, and the Pediatric Endocrine Society (formerly Lawson Wilkins Pediatric Endocrine Society). Diabetes Care. 2011;34(11):2477-2485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Everett E, Mathioudakis NN. Association of socioeconomic status and DKA readmission in adults with type 1 diabetes: analysis of the US National Readmission Database. BMJ Open Diabetes Res Care. 2019;7(1):e000621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Weinstock RS, Xing D, Maahs DM, et al. ; T1D Exchange Clinic Network . Severe hypoglycemia and diabetic ketoacidosis in adults with type 1 diabetes: results from the T1D Exchange clinic registry. J Clin Endocrinol Metab. 2013;98(8):3411-3419. [DOI] [PubMed] [Google Scholar]
- 27. Delamater AM, de Wit M, McDarby V, et al. . ISPAD clinical practice consensus guidelines 2018: psychological care of children and adolescents with type 1 diabetes. Pediatr Diabetes. 2018;19 Suppl 27:237-249. [DOI] [PubMed] [Google Scholar]
- 28.Usher-Smith JA, Thompson MJ, Sharp SJ, Walter FM. Factors associated with the presence of diabetic ketoacidosis at diagnosis of diabetes in children and young adults: a systematic review. BMJ. 2011;343. doi: 10.1136/bmj.d4092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chalew S, Gomez R, Vargas A, et al. . Hemoglobin A1c, frequency of glucose testing and social disadvantage: metrics of racial health disparity in youth with type 1 diabetes. J Diabetes Complications. 2018;32(12):1085-1090. [DOI] [PubMed] [Google Scholar]
- 30. Özcan B, Rutters F, Snoek FJ, et al. ; Diabetes Pearl from the Parelsnoer Initiative . High diabetes distress among ethnic minorities is not explained by metabolic, cardiovascular, or lifestyle factors: findings from the dutch diabetes pearl cohort. Diabetes Care. 2018;41(9):1854-1861. [DOI] [PubMed] [Google Scholar]
- 31. Spanakis EK, Golden SH. Race/ethnic difference in diabetes and diabetic complications. Curr Diab Rep. 2013;13(6):814-823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wagner J, Abbott G. Depression and depression care in diabetes: relationship to perceived discrimination in African Americans. Diabetes Care. 2007;30(2):364-366. [DOI] [PubMed] [Google Scholar]
- 33. Willi SM, Miller KM, DiMeglio LA, et al. ; T1D Exchange Clinic Network . Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics. 2015;135(3):424-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wisk LE, Witt WP. Predictors of delayed or forgone needed health care for families with children. Pediatrics. 2012;130(6):1027-1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bui H, To T, Stein R, Fung K, Daneman D. Is diabetic ketoacidosis at disease onset a result of missed diagnosis? J Pediatr 2010;156(3). doi: 10.1016/j.jpeds.2009.10.001 [DOI] [PubMed] [Google Scholar]
- 36. Herkert D, Vijayakumar P, Luo J, et al. . Cost-related insulin underuse among patients with diabetes. JAMA Intern Med. 2019;179(1):112-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Karter AJ, Parker MM, Solomon MD, et al. . Effect of out-of-pocket cost on medication initiation, adherence, and persistence among patients with type 2 diabetes: the Diabetes Study of Northern California (DISTANCE). Health Serv Res. 2018;53(2):1227-1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Luo J, Avorn J, Kesselheim AS. Trends in medicaid reimbursements for insulin from 1991 through 2014. JAMA Intern Med. 2015;175(10):1681-1686. [DOI] [PubMed] [Google Scholar]
- 39. Fralick M, Kesselheim AS. The U.S. insulin crisis—rationing a lifesaving medication discovered in the 1920s. N Engl J Med. 2019;381(19):1793-1795. [DOI] [PubMed] [Google Scholar]
- 40. Rosenthal E. When high prices mean needless death. JAMA Intern Med. 2019;179(1):114-115. [DOI] [PubMed] [Google Scholar]
- 41. American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917-928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Anderson GF, Hussey P, Petrosyan V. It’s still the prices, stupid: why the US spends so much on health care, and a tribute to uwe reinhardt. Health Aff (Millwood). 2019;38(1):87-95. [DOI] [PubMed] [Google Scholar]
- 43. McDermott KW, Elixhauser A, Sun R. Staistical brief #225: patient trends in hospital inpatient stays in the United States, 2005–2014. 2017.225. June 2017. Accessed February 6, 2020. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb225-Inpatient-US-Stays-Trends.jsp?utm_source=ahrq&utm_medium=en1&utm_term=&utm_content=1&utm_campaign=ahrq_en7_5_2017
- 44. Riddle MC, Herman WH. The cost of diabetes care-an elephant in the room. Diabetes Care. 2018;41(5):929-932. [DOI] [PubMed] [Google Scholar]
- 45. Wisk LE, Gangnon R, Vanness DJ, Galbraith AA, Mullahy J, Witt WP. Development of a novel, objective measure of health care-related financial burden for U.S. families with children. Health Serv Res. 2014;49(6):1852-1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Bull SV, Douglas IS, Foster M, Albert RK. Mandatory protocol for treating adult patients with diabetic ketoacidosis decreases intensive care unit and hospital lengths of stay: results of a nonrandomized trial. Crit Care Med. 2007;35(1):41-46. [DOI] [PubMed] [Google Scholar]
- 47. Islam T, Sherani K, Surani S, Vakil A. Guidelines and controversies in the management of diabetic ketoacidosis—a mini-review. World J Diabetes. 2018;9(12):226-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Copeland T, Wisk LE. Changes in the measurement of chronic disease burden in the US resulting from the switch from ICD-9 to ICD-10. Poster presented at: Academy Health Annual Research Meeting. July 28-August 6, 2020.
- 49. Tieder JS, McLeod L, Keren R, et al. . Variation in resource use and readmission for diabetic ketoacidosis in children’s hospitals. Pediatrics. 2013;132(2). doi: 10.1542/peds.2013-0359. [DOI] [PubMed] [Google Scholar]
- 50. Newton CA, Raskin P. Diabetic ketoacidosis in type 1 and type 2 diabetes mellitus: clinical and biochemical differences. Arch Intern Med. 2004;164(17):1925-1931. [DOI] [PubMed] [Google Scholar]
- 51. van den Boom L, Karges B, Auzanneau M, et al. . Temporal trends and contemporary use of insulin pump therapy and glucose monitoring among children, adolescents, and adults with type 1 diabetes between 1995 and 2017. Diabetes Care. 2019;42(11). doi: 10.2337/dc19-0345. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Some or all data generated or analyzed during this study are included in this published article or in the data repositories listed in the References.