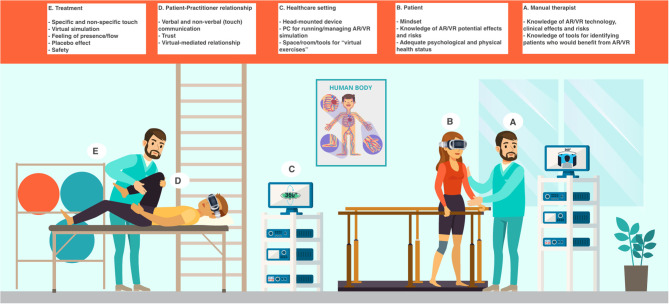
Figure 1.
The integration of VR and AR in the MT setting. The MT setting would be enhanced by the addition of VR and AR: however, this implies the therapist and the patient need to pay attention to both old and new therapeutic factors. The factors could be summarized as follows (see the section “The Crossroads between MTs, VR and AR,” for further information). (A) Manual therapist's features: knowledge of AR and VR technology, clinical effects and risks; knowledge of tools (e.g., questionnaires, biomarkers such as heart rate variability) for identifying patients who would benefit from AR or VR (every patient could respond differently to them and some patients could be at a higher risk of experiencing adverse effects, from cybersickness to depersonalization). (B) Patient's features: mindset (i.e., expectation about VR or AR positive effects); knowledge of AR and VR potential effects and risks; adequate psychological and physical health status (based on their psychophysical health, some patients could be at a higher risk of experiencing adverse effects, from cybersickness to depersonalization). (C) Healthcare setting: head-mounted device; PC (or other types of hardware) for running/managing AR or VR simulation; space/room/tools for “virtual exercises.” (D) Patient-practitioner relationship: verbal and non-verbal (touch) communication; trust (it is paramount when the patient is immersed in the virtual environment and, therefore, does not see the “real” therapist); virtual-mediated relationship (in the virtual simulation, there could be an avatar of the therapist and phenomena like the uncanny valley could happen). (E) Treatment features: specific (technical) and non-specific (placebo) touch; virtual simulation; feeling of presence/flow (necessary for an optimal AR and VR experience); placebo effect (the patient could feel better just due to the simple fact that an “awesome” technology is being used); safety.