Abstract
Introduction:
Cost sharing can deter the use of health services and act as a potential contributor to racial/ethnic disparities in cancer. The Affordable Care Act required most health plans to cover, without cost sharing, preventive services, including colorectal cancer screening. Population-based data were used to estimate the impact of the Affordable Care Act’s cost-sharing provision (together with other Affordable Care Act provisions targeting preventive care) on ethnic disparities in colorectal cancer screening, comparing Hispanics with non-Hispanics.
Methods:
An interrupted time series quasi-experimental analysis was used to examine ethnic differences in colorectal cancer screening pre- and post-implementation of the Affordable Care Act (analysis performed in 2018). The study cohort included insured individuals aged 50–64 years who participated in the Medical Expenditure Panel Survey from 2007 through 2015 (n=44,343).
Results:
During the pre-Affordable Care Act period, screening rates decreased annually for non-Hispanics by −0.38 per 100 adults per year (95% CI= −0.55, −0.22) but remained level for Hispanics (annual trend per 100 adults: 0.01, 95% CI= −0.34, 0.35). After cost sharing was eliminated in 2011, colorectal cancer screening rates increased for both Hispanics (by 1.29 per 100 adults, 95% CI=0.69, 1.89) and non-Hispanics (by 0.58 per 100 adults, 95% CI=0.18, 0.99). The difference in trend increases between Hispanics and non-Hispanics was not statistically significant (0.70%, 95% CI= −0.24, 1.64).
Conclusions:
These findings suggest that Affordable Care Act implementation resulted in increased colorectal cancer screening; however, the effect of the law was not significantly different between Hispanics and non-Hispanics. These results provide indications that more needs to be done to reduce racial/ethnic disparities in colorectal cancer screening.
INTRODUCTION
Colorectal cancer (CRC) is the third leading cause of cancer deaths in the U.S. Routine screening for CRC can both prevent the disease through the identification and removal of precancerous polyps and detect cancer at earlier stages when treatment is more successful.1 On average, CRC screening is associated with a 30%—60% reduction in CRC incidence and mortality.2 As such, the U.S. Preventive Services Task Force assigned CRC screening in adults aged 50—75 years an A rating to reflect the substantial net benefits of this screening service.3 Despite overwhelming evidence in support of CRC screening as a cancer preventive service, less than two thirds of age-eligible Americans are CRC screening compliant, with much lower compliance among some racial/ethnic groups. For example, whereas screening prevalence among the general population of individuals aged 50–75 years is 62%, the prevalence among Hispanics is only 50%.4 There are several deterrents to screening, but cost is considered an important barrier, as well as a potential contributor to screening disparities.5
A substantive body of literature shows that cost sharing, in the form of a deductible, copayment, or other out-of-pocket expense, can deter the use of preventive health services.6–13 Compared with whites, Hispanics are more likely to have incomes lower than 100% of the federal poverty level and report cost as a barrier to accessing healthcare services.14 Hispanics also report worse access to and utilization of health services than other racial/ethnic groups.15 In 2006, Hispanics were twice as likely as black, non-Hispanics and 3 times as likely as white, non-Hispanics to lack a regular healthcare provider.16,17 Moreover, whereas 12% of nonelderly whites were uninsured before implementation of the Affordable Care Act (ACA), nearly 26% of Hispanics were uninsured during this timeframe.18
Among many policy changes, the ACA addressed cost-related barriers to preventive care through no cost-sharing provisions for preventive services. Starting January 1, 2011, the ACA required most health plans to cover, without cost sharing, all U.S. Preventive Services Task Force-recommended services with A or B ratings, including CRC screening.19,20 Before this provision, the cost to patients for some cancer screenings was high, especially for colonoscopy,19 which is the most common form of CRC screening across ethnic groups.1
Findings on the impact of the ACA’s cost-sharing provision in 2011 on CRC screening utilization have been mixed, but evidence to date suggests that the impact was greatest among those with cost-related barriers to screening.2,19,21,22 Owing to data lags, most existing studies examine only short time periods post-ACA. Further, although a few studies examine screening changes by race/ethnicity,19,21 many do not and very few studies have directly examined the ACA’s impact on longstanding ethnic disparities in CRC screening.22 This work extends previous studies by directly comparing changes in screening between ethnic groups over time and using additional data years post-implementation of the cost-sharing provision.
This study examined the impact of the ACA’s cost-sharing provision implemented in 2011 (together with other ACA provisions targeting preventive care) on CRC screening disparities, comparing pre- and post-ACA screening trends among Hispanics versus non-Hispanics. Nine years of data were analyzed, including 5 years before and 4 years after the ACA eliminated cost sharing. Based on the expectation that Hispanics faced greater cost barriers to screening, authors hypothesized that the magnitude of ethnic disparities in CRC screening decreased after implementation of the cost-sharing provision.
METHODS
Data were obtained from the household component of the Medical Expenditure Panel Survey (MEPS), a nationally representative survey of the U.S. civilian non-institutionalized population administered by the Agency for Health Care Research and Quality.23 The MEPS collects detailed information during 5 rounds of interviewing over a 2-year period on demographics, household income, person-level health conditions/status, quality of care, employment, health insurance, and person-level medical care use and expenditures. The household component has an overlapping panel design and oversamples for racial/ethnic minorities to increase the precision of estimates for these groups. Pooled MEPS consolidated files for 2007–2015 were used for this analysis.
Study Sample
The study sample included insured individuals aged 50–64 years at their survey. The pre- and post-ACA cohorts were constructed around elimination of cost sharing for preventive care, which started on January 1, 2011. The retrospective nature of the survey (participants asked if they have had a CRC screening within the past year) was accounted for by including 2011 survey takers in the pre-ACA cohort. The past year for these 2011 participants included some time in 2010, before elimination of cost sharing for preventive services. This cohort definition also allowed for examination of potential lags for the law to have an impact; the pre-ACA group included individuals surveyed during 2007–2011 and the post-ACA cohort included individuals surveyed during 2012–2015. The analytic cohort included 44,343 individuals over 9 years. Both the Hispanic and non-Hispanic populations comprised all racial groups.
Measures
The primary outcome measure was annual CRC screening rates by Hispanic ethnicity, defined as the number of individuals within each ethnic group who completed a CRC screening in the past year divided by the total number of individuals within that group for each year. Screening was self-reported receipt of a colonoscopy, sigmoidoscopy, or fecal occult blood test within the past year. Annual screening rates were used instead of the prevalence of being up to date to more narrowly focus on new CRC screenings. Further, the structure of the response categories to CRC screening questions in MEPS 2007 and 2008 made it difficult to capture up-to-date status for individuals who were screened using colonoscopy. Individuals with missing values for screening (including those with a don’t know or refused response) were classified as not screened. The distribution of missing screening data was similar over time.
Statistical Analysis
Standardized mean differences were used to compare sociodemographic and health characteristics between the pre- and post-ACA cohorts.24 The standardized difference assesses the degree of imbalance in covariates across pre- and post-ACA time periods using pooled SD units and is not influenced by sample size, unlike other common hypothesis tests.25 Standardized differences for measured covariates indicated low imbalance between the preand post-ACA cohorts24,25; therefore, in estimating screening trends over time, these characteristics were not adjusted for.
A stratified interrupted time series (ITS) analysis with segmented linear regression was conducted to examine changes in CRC screening rates pre- and post-ACA. In using ITS, the analysis controlled for the presence of temporal confounders and secular trends in CRC use over time and quantified the change in the slope of CRC screening trends over time, comparing the post-with pre-ACA periods.26 The immediate level change (jump) was not computed as is sometimes implemented in its analysis because of the anticipation of a more gradual increase in screening around the period when the provision was first implemented. Excluding the jump parameter also removes the flexibility at the point of the intervention before the increase in slopes and reduces potential overestimation of the post-ACA trend that may be an artifact of the jump fluctuation and model sensitivity.
The analytic model included the 2 standard ITS components: pre-ACA slope and change in slope in the post-ACA period, separately for Hispanics and non-Hispanics. To compute the overall change in pre-post screening slopes comparing Hispanics with non-Hispanics, a model that adds a main effect term for ethnicity and an interaction term for ethnicity and time since the ACA interruption was used; the latter identifies the difference-in-trend-change between these 2 ethnic groups that occurred at the interruption. Trends and differences in slopes along with 95% CIs were estimated. The full specification of the main regression model can be found online in the Appendix (available online).
Serial autocorrelation over time was assessed using Durbin-Watson tests27 with a sensitive a priori a level (0.1); however, given that none of the models exhibited evidence of serial autocorrelation, no parameters for autocorrelated errors were included.
Four sensitivity analyses were performed. First, the level change (jump) was added in the ITS model to anticipate a potentially more immediate effect of the interruption instead of a more gradual change as currently modeled in the ITS analysis. Second, to address concerns related to measurement error and uncertainty, individuals surveyed in 2011 were dropped as the CRC screening timeframe for these individuals might have included both the preand post-ACA interruption time periods. Third, a model that both included the level change and excluded the 2011 data was implemented. Finally, to evaluate the potential impact of coding individuals with don’t know and refused outcome responses as not screened, those individuals were recoded as having missing outcome data and the new data set was analyzed using complete case analysis.
Analyses were performed in 2018 using Stata, version 13.1 and SAS, version 9.4.
RESULTS
Sample characteristics by pre- and post-ACA interruption time periods are shown in Table 1. In this study population, the average age was 56 years, and most participants were white, female, married, privately insured, and middle or high income and reported an overall health status of excellent or very good. Hispanics constituted 15.0% of the pre-ACA and 19.4% of the post-ACA study sample. Outside of ethnicity, there were small imbalances in characteristics between the pre- and post-ACA periods.
Table 1.
Characteristics of Pre- and Post-ACA Study Population Age 50–64 Years (n=44,343)
| Characteristics | Pre-ACA, 2007–2011 (n=23,271) n (%) |
Post-ACA, 2012–2015 (n=21,072) n (%) |
SMD |
|---|---|---|---|
| Hispanic ethnicity | 3,483 (15.0) | 4,094 (19.4) | 0.118 |
| Nonwhite race | 6,251 (27.1) | 6,541 (31.5) | 0.096 |
| Age, years, mean (SD) | 56.4 (4.2) | 56.6 (4.2) | 0.043 |
| Male | 10,810 (46.5) | 9,693 (46.0) | −0.009 |
| Education | |||
| High school or less | 10,727 (46.6) | 8,261 (45.3) | −0.027 |
| Some college or degree | 9,317 (40.5) | 7,992 (43.8) | 0.067 |
| Graduate/professional | 2,955 (12.8) | 1,988 (10.9) | −0.060 |
| Missing | 272 | 2,831 | |
| Poverty level | |||
| Poor or near poor | 3,223 (13.8) | 3,612 (17.1) | 0.091 |
| Low income | 2,499 (10.7) | 2,547 (12.1) | 0.042 |
| Middle income | 6,788 (29.2) | 6,057 (28.7) | −0.009 |
| High income | 10,761 (46.2) | 8,856 (42.0) | −0.085 |
| Insurance status | |||
| Private | 19,529 (83.9) | 16,429 (78.0) | −0.152 |
| Public only | 3,742 (16.1) | 4,643 (22.0) | 0.152 |
| Marital status | |||
| Married | 15,249 (65.5) | 12,931 (61.4) | −0.086 |
| Widowed | 1,029 (4.4) | 977 (4.6) | −0.010 |
| Divorced | 4,145 (17.8) | 3,859 (18.3) | 0.013 |
| Never married | 2,848 (12.2) | 3,304 (15.7) | 0.099 |
| Missing | 0 | 1 | |
| Self-reported overall health | |||
| Excellent or very good | 9,622 (45.5) | 8,294 (44.5) | −0.020 |
| Good | 7,217 (34.1) | 6,234 (33.4) | −0.015 |
| Fair | 3,350 (15.8) | 3,252 (17.4) | 0.043 |
| Poor | 961 (4.5) | 867 (4.6) | 0.005 |
| Missing | 2,121 | 2,425 | |
ACA, Affordable Care Act; SMD, standardized mean difference.
Figure 1 and Table 2 show results from the interrupted time series analysis of trends in CRC screening over time, stratified by ethnicity. A visual inspection of screening trends indicates discernible changes in screening slopes for both Hispanics and non-Hispanics from pre- to post-ACA. Before elimination of cost sharing for preventive services, the average annual CRC screening prevalence for 2007–2011 was 22 per 100 adults. During the pre-ACA period, screening rates decreased annually for non-Hispanics by −0.38 per 100 adults per year (95% CI= −0.55, 0.22) but remained level for Hispanics (annual trend per 100 adults: 0.01, 95% CI= −0.34, 0.35). After the ACA was implemented, screening rates increased for both groups. Hispanics had a post-ACA slope of 1.29 per 100 adults per year (95% CI=0.69, 1.89) and non-Hispanics had a post-ACA slope of 0.20 per 100 adults per year (95% CI= −0.09, 0.48). In summary, after implementation of the law, Hispanics experienced an upward change in the annual trend for screening rates of 1.29 per 100 adults (95% CI=0.69, 1.89) versus a smaller upward change in the annual trend for screening rates among non-Hispanics (0.58 per 100 adults, 95% CI=0.18, 0.99). However, the difference-in-trend-change between Hispanics and non-Hispanics was insignificant (0.70 per 100 per year, 95% CI= −0.24, 1.64).
Figure 1.
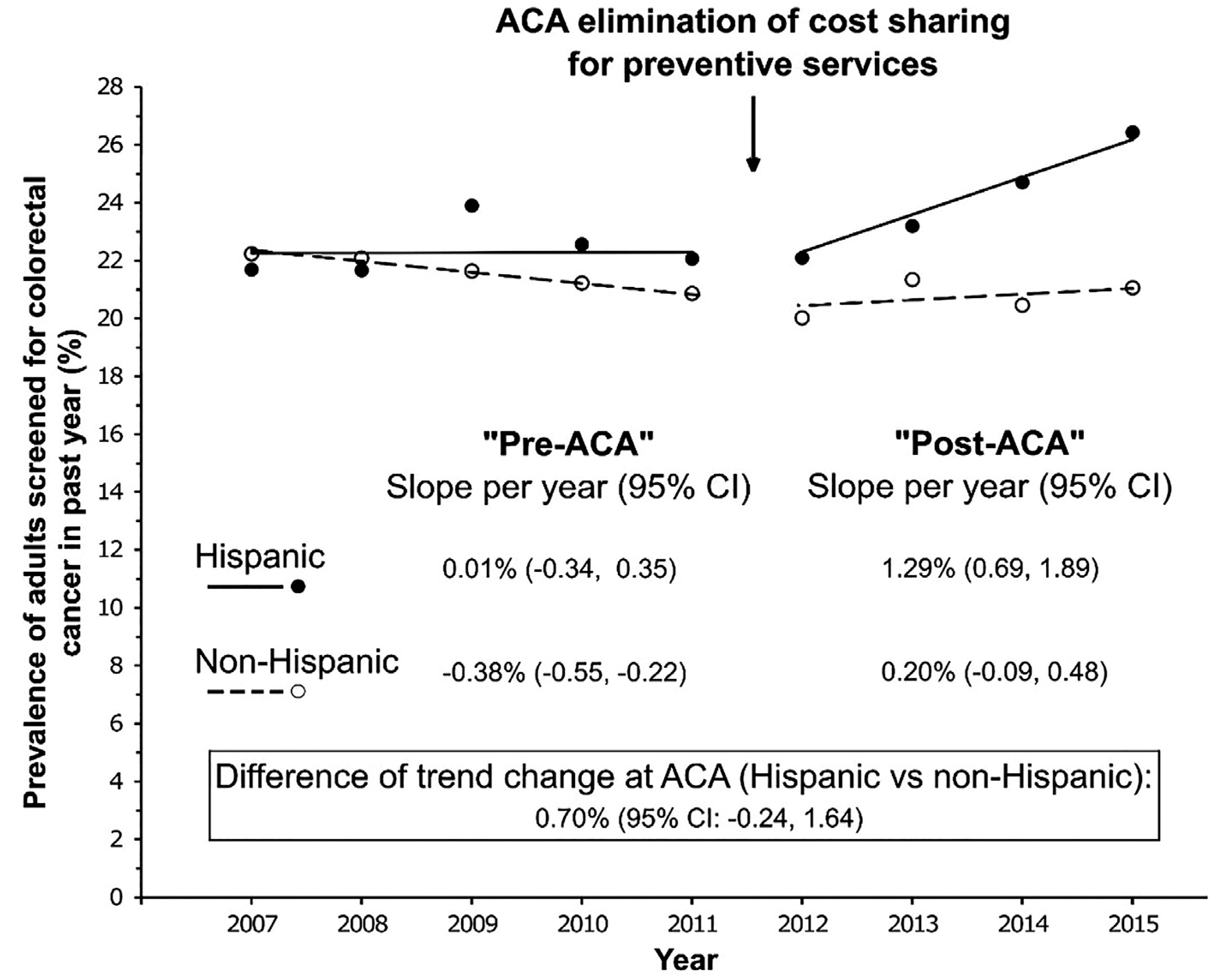
Segmented trend estimates of annual colorectal cancer screening rates for Hispanic versus non-Hispanic adults aged 50–64 years, 2007–2015.
Source: Authors’ analysis of data from the Medical Expenditure Panel Survey, 2007–2015.
ACA, Affordable Care Act.
Table 2.
Segmented Linear Regression Model for Annual Colorectal Cancer Screening Rates for Hispanic Versus Non-Hispanic Adults Aged 50–64 Years, 2007–2015
| Parameter | Hispanic Estimate (95% CI) | Non-Hispanic Estimate (95% CI) |
|---|---|---|
| Intercept | 22.25 (20.84, 23.66) | 22.75 (22.08, 23.42) |
| Pre-ACA trend | 0.01 (−0.34, 0.35) | −0.38 (−0.55, −0.22) |
| Post-ACA trend | 1.29 (0.69,1.89) | 0.20 (−0.09, 0.48) |
| Post-ACA trend change | 1.29 (0.44, 2.13) | 0.58 (0.18, 0.99) |
Note: Boldface indicates statistical significance (p<0.05). Estimates correspond to the prevalence per 100 individuals (for the intercept) or the change in prevalence per 100 individuals per year (for trends).
ACA, Affordable Care Act.
The interpretation of these results was not altered by 3 of the 4 sensitivity analyses: adding the level change in the ITS model, dropping individuals surveyed in 2011, and running a model that both included the level change and excluded the 2011 data (Appendix Figure 1 and Appendix Tables 1–3, available online). However, when the authors assessed don’t know and refused outcome status as missing data rather than not screened (Appendix Table 4, available online), the post-ACA increasing trends in screening were statistically significant only for Hispanics (1.00 per 100 adults, 95% CI=0.23, 1.78) and not for non-Hispanics (0.08 per 100 adults, 95% CI= −0.27, 0.44). Changes in pre-post trends were not statistically significant for both groups (Hispanics: 0.64 per 100 adults, 95% CI= −0.46, 1.74; non-Hispanics: 0.33 per 100 adults, 95% CI= −0.17, 0.83).
DISCUSSION
Study findings indicate that annual rates of CRC screening increased for both Hispanic and non-Hispanic individuals aged 50–64 years after the ACA eliminated cost sharing for preventive services. There was a slight post-implementation trend reversal, from a decreasing to a slightly increasing screening slope among non-Hispanics and an increasing post-ACA screening slope among Hispanics. However, the difference in pre-post ACA changes in CRC screening between Hispanics and non-Hispanics was not significant. These findings suggest that although implementation of the ACA’s cost-sharing provision (and other ACA provisions targeting preventive care) resulted in increased CRC screening in both Hispanics and non-Hispanics, the study’s hypothesis that the law would be more pronounced among Hispanics, and thus reduce screening disparities, did not hold. The primary goal of the cost-sharing provision was to eliminate out-of-pocket costs for preventive care, including for CRC screening. The higher rates of annual screening post-ACA among Hispanics compared with non-Hispanics indicate that Hispanics may have benefitted more from elimination of cost sharing than non-Hispanics. These results therefore lend credence to the notion that Hispanics might have experienced greater cost-related barriers to screening before implementation of the law, despite the present estimates of the difference-in-trend-change between ethnic groups being imprecise at α=0.05.
Although early studies examining the impact of the ACA’s cost-sharing provision on CRC screening have produced mixed results, this study’s findings are consistent with several studies that have shown a post-implementation uptake in screening. Examining the 1-year impact of the ACA provision on CRC screening among high deductible health plan members, Wharam et al.28 similarly showed a decline in screening rates pre-ACA and an increasing rate post-ACA. Fedewa and colleagues19 also reported an overall increase in CRC screening prevalence after implementation of the cost-sharing provision, notably among low-income and least-educated individuals. Although several prior studies examined the impact of the cost-sharing provision on cancer screening in the overall population and among subpopulations, such as men and low-income individuals, very few have shed light on the effect of the provision on persistent ethnic disparities in CRC screening. This is also one of very few studies that have examined the impact of the ACA using 9 years of data.
Reduced cost sharing and health insurance coverage are important enablers for accessing health services. These study findings provide encouraging indications that provisions targeting increased access to preventive services may help reduce disparities in CRC screening, with potential for impacting inequities in CRC diagnosis and survival. The benefits of eliminating cost sharing are, however, limited to individuals with health insurance coverage. Although the ACA enabled large coverage gains among Hispanics, this group remains disproportionately uninsured.29 CRC screening disparities persist, with a much lower proportion of Hispanics reporting being up to date with screening when compared with non-Hispanics.1 It is important to note that this study examined annual screening rates (i.e., new screenings within the past year) and not prevalence of adults who report being up to date on CRC screening. Although study findings indicate that the rate of annual CRC screening increased for Hispanics and non-Hispanics, the historically lower annual rates make the prevalence of being up to date much lower for Hispanics. Further, the nonsignificant estimate for pre-post changes in screening between the 2 groups indicates that there was no meaningful reduction in CRC screening disparities because of the law. If annual screening trends continue as observed in this study, the prevalence gap may eventually close, but this will likely take a very long time. Hispanics are one of the fastest growing racial/ethnic groups in the U.S. and are projected to reach 30% of the U.S. population by 2030.15 Though study findings of increasing annual CRC screening trends among Hispanics is encouraging, much more needs to be done to mitigate ethnic disparities in the prevalence of CRC screening. These findings also have important implications for health insurance expansion efforts.
Limitations
The analysis has several limitations. Although ITS analysis can be a useful method for examining population-level policy interventions30 when individual-level confounding variables remain constant over time, these results might have been affected by other population-level factors that were associated with CRC screening rates. The assumption was made, based on thorough review, that no other policies outside of the ACA were implemented during the study period that would have plausibly affected CRC screening differently between Hispanics and non-Hispanics at the national level. It was difficult to disentangle the effect of the cost-sharing provision from other ACA provisions (e.g., health insurance expansion implemented in 2014); therefore, effect estimates likely reflect a combined effect of ACA provisions implemented during the post-ACA study period (2011–2015). The MEPS data provide annual data, which limited the ITS analysis to 9 time points; however, Lopez et al.31 have pointed out that there is no clear minimum number of time points for ITS analysis, as their power depends on multiple factors. There was no distinction in the MEPS data between screening and diagnostic CRC procedures before 2009; therefore, although the cost-sharing provision applies to screening tests only, both tests were assessed. Individuals reporting a diagnostic or other nonroutine screening accounted for a small proportion of screened individuals, and that proportion remained stable over time (data not shown). The study’s use of annual screening rates (versus prevalence of up-to-date screening) might have resulted in underestimation of disparities, given that non-Hispanics may be more likely than Hispanics to get colonoscopies,32 which are recommended once every 10 years and thus have lower annual screening rates. Sensitivity analysis dealing with treatment of missing data led to slightly different results than the main analysis; findings should therefore be interpreted with some caution. A final limitation was potential recall bias, as MEPS cancer screening data are based on self-report.33
CONCLUSIONS
This study examined the impact of the ACA’s cost-sharing provision on ethnic disparities in CRC screening among individuals aged 50–64 years. Study findings suggest that the ACA was associated with increased CRC screening in both Hispanics and non-Hispanics, but the difference in pre-post ACA changes in screening between Hispanics and non-Hispanics was not significant. Policies targeting increased access to preventive services may help reduce disparities by disproportionately benefiting previously underserved groups. The law did not disproportionately increase the rate of screening among Hispanics in this case, so more needs to be done to close this screening gap.
Supplementary Material
ACKNOWLEDGMENTS
Olive M. Mbah is supported by the National Cancer Institute’s National Research Service Award sponsored by the Lineberger Comprehensive Cancer Center at the University of North Carolina (grant number: T32 CA116339). Cleo A. Samuel is funded by the National Cancer Institute Mentored Research Scientist Development Award (grant number: 1 K01 CA218473–01A1). Alan C. Kinlaw received funding support from a National Research Service Award Postdoctoral Traineeship from the Agency for Health care Research and Quality sponsored by the Cecil G. Sheps Center for Health Services Research at the University of North Carolina at Chapel Hill (5T32 HS000032–28).
The study was conceptualized by OMM, but all authors contributed to the design. Data analysis was carried out by OMM and ACK. All authors contributed to the writing and final approval of the manuscript.
No financial disclosures were reported by the authors of this paper.
Footnotes
SUPPLEMENTAL MATERIAL
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2019.09.002.
REFERENCES
- 1.American Cancer Society. Colorectal Cancer Facts & Figures 2017–2019. Atlanta, GA: American Cancer Society, 2017. [Google Scholar]
- 2.Hamman MK, Kapinos KA. Affordable Care Act provision lowered out-of-pocket cost and increased colonoscopy rates among men in Medicare. Health Aff (Millwood). 2015;34(12):2069–2076. 10.1377/hlthaff.2015.0571. [DOI] [PubMed] [Google Scholar]
- 3.U.S. Preventive Services Task Force. Grade definitions after July 2012. www.uspreventiveservicestaskforce.org/Page/Name/grade-definitions. Published 2012. Accessed September 10, 2019.
- 4.American Cancer Society. Cancer Facts & Figures 2017. Atlanta, GA: American Cancer Society, 2017. [Google Scholar]
- 5.Bromley EG, May FP, Federer L, Spiegel BM, van Oijen MG. Explaining persistent under-use of colonoscopic cancer screening in African Americans: a systematic review. Prev Med. 2015;71:40–48. 10.1016/j.ypmed.2014.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Trivedi AN, Leyva B, Lee Y, Panagiotou OA, Dahabreh IJ. Elimination of cost sharing for screening mammography in Medicare Advantage plans. N Engl J Med. 2018;378(3):262–269. 10.1056/NEJMsa1706808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trivedi AN, Rakowski W, Ayanian JZ. Effect of cost sharing on screening mammography in Medicare health plans. N Engl J Med. 2008;358(4):375–383. 10.1056/NEJMsa070929. [DOI] [PubMed] [Google Scholar]
- 8.Rubin RJ, Mendelson DN. Cost sharing in health insurance. N Engl J Med. 1995;333(11):733–734. 10.1056/NEJM199509143331115. [DOI] [PubMed] [Google Scholar]
- 9.Newhouse JP, Manning WG, Morris CN, et al. Some interim results from a controlled trial of cost sharing in health insurance. N Engl J Med. 1981;305(25):1501–1507. 10.1056/NEJM198112173052504. [DOI] [PubMed] [Google Scholar]
- 10.Rice T, Matsuoka KY. The impact of cost-sharing on appropriate utilization and health status: a review of the literature on seniors. Med Care Res Rev. 2004;61(4):415–452. 10.1177/1077558704269498. [DOI] [PubMed] [Google Scholar]
- 11.Swartz K. Cost-sharing: effects on spending and outcomes. Boston, MA: Robert Wood Johnson Foundation. https://pdfs.semanticscholar.org/786b/cb85cdd5bba0f4b5939d0f428707b6e9bbe2.pdf. Published 2010. Accessed September 10, 2019. [Google Scholar]
- 12.Lurie N, Manning WG, Peterson C, Goldberg GA, Phelps CA, Lillard L. Preventive care: do we practice what we preach. Am J Public Health. 1987;77(7):801–804. 10.2105/ajph.77.7.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Solanki G, Schauffler HH. Cost-sharing and the utilization of clinical preventive services. Am J Prev Med. 1999;17(2):127–133. 10.1016/s0749-3797(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 14.Kaiser Family Foundation. Health and Health Care for Hispanics in the United States. Kaiser Family Foundation. www.kff.org/infographic/health-and-health-care-for-hispanics-in-the-united-states/. Published 2019. Accessed September 10, 2019. [Google Scholar]
- 15.Ortega AN, Rodriguez HP, Vargas Bustamante A. Policy dilemmas in Latino health care and implementation of the Affordable Care Act. Annu Rev Public Health. 2015;36:525–544. 10.1146/annurev-publhealth-031914-122421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Livingston G, Minushkin S, Cohn D. Hispanics and Health Care in the United States: Access, Information and Knowledge. Pew Research Center. www.pewresearch.org/hispanic/2008/08/13/hispanics-and-health-care-in-the-united-states-access-information-and-knowledge/.Published 2008. Accessed September 24, 2018. [Google Scholar]
- 17.Pleis JR, Lethbridge-Cejku M. Summary health statistics for U.S. adults: National Health Interview Survey, 2006. Vital Health Stat 10. 2007;235(235):1–153. 10.1037/e403882008-001. [DOI] [PubMed] [Google Scholar]
- 18.Artiga S, Ubri P, Foutz J, Damico A. Health coverage by race and ethnicity: examining changes under the ACA and the remaining uninsured. http://files.kff.org/attachment/Issue-Brief-Health-Coverage-by-Race-and-Ethnicity-Examining-Changes-Under-the-ACA-and-the-Remaining-Uninsured. Published 2016. Accessed September 24, 2019.
- 19.Fedewa SA, Goodman M, Flanders WD, et al. Elimination of cost-sharing and receipt of screening for colorectal and breast cancer. Cancer. 2015;121(18):3272–3280. 10.1002/cncr.29494. [DOI] [PubMed] [Google Scholar]
- 20.Koh HK, Sebelius KG. Promoting prevention through the Affordable Care Act. N Engl J Med. 2010;363(14):1296–1299. 10.1056/NEJMp1008560. [DOI] [PubMed] [Google Scholar]
- 21.Richman I, Asch SM, Bhattacharya J, Owens DK. Colorectal cancer screening in the era of the Affordable Care Act. J Gen Intern Med. 2016;31(3):315–320. 10.1007/s11606-015-3504-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sabik LM, Adunlin G. The ACA and cancer screening and diagnosis. Cancer J. 2017;23(3):151–162. 10.1097/PPO.0000000000000261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agency for Health care Research and Quality. Medical Expenditure Panel Survey - Survey Background. Agency for Health care Research and Quality. https://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp. Accessed September 24, 2018. [Google Scholar]
- 24.Yang D, Dalton E. A unified approach to measuring the effect size between two groups using SAS. SAS Glob Forum. 2012;335:1–6. https://pdfs.semanticscholar.org/6cf4/bd36ca4c90006a5d6563f646a391c255581b.pdf?_ga=2.155892605.71930856.1571423641-1110825170.1571423641. Accessed September 20, 2018. [Google Scholar]
- 25.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–3107. 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huesch MD, Schetter S, Segel J, Chetlen A. Evaluation of the “Angelina Jolie Effect” on screening mammography utilization in an academic center. J Am Coll Radiol. 2017;14(8):1020–1026. 10.1016/j.jacr.2017.03.016. [DOI] [PubMed] [Google Scholar]
- 27.Durbin J, Watson GS. Testing for serial correlation in least squares regression. I. Biometrika. 1950;37(3–4):409–428. 10.1093/biomet/37.3-4.409. [DOI] [PubMed] [Google Scholar]
- 28.Wharam JF, Zhang F, Landon BE, LeCates R, Soumerai S, Ross-Degnan D. Colorectal cancer screening in a nationwide high-deductible health plan before and after the Affordable Care Act. Med Care. 2016;54(5):466–473. 10.1097/MLR.0000000000000521. [DOI] [PubMed] [Google Scholar]
- 29.Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr. 2013;13(6 suppl):S38–S44. 10.1016/j.acap.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 30.Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–355. 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Inadomi JM, Vijan S, Janz NK, et al. Adherence to colorectal cancer screening: a randomized clinical trial of competing strategies. Arch Intern Med. 2012;172(7):575–582. 10.1001/archinternmed.2012.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hiatt RA, Pérez-Stable EJ, Quesenberry C Jr., Sabogal F, Otero-Sabogal R, McPhee SJ. Agreement between self-reported early cancer detection practices and medical audits among Hispanic and non-Hispanic white health plan members in northern California. Prev Med. 1995;24(3):278–285. 10.1006/pmed.1995.1045. [DOI] [PubMed] [Google Scholar]
- 33.Doty MM, Beutel S, Rasmussen PW, Collins SR. Latinos Have Made Coverage Gains but Millions Are Still Uninsured. The Commonwealth Fund. www.commonwealthfund.org/blog/2015/latinos-have-made-coverage-gains-millions-are-still-uninsured. Published 2015. Accessed September 26, 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


