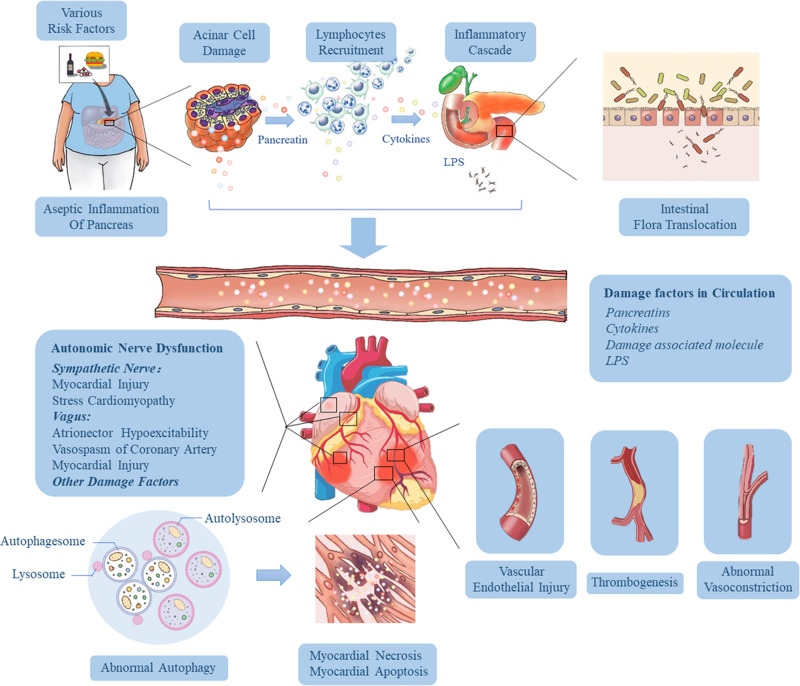
Figure 2.
Pathophysiological mechanisms influencing the development of cardiac injury in SAP. Various risk factors (gallstones, alcohol, diet and drugs) cause acinar cell damage and the release of pancreatic hydrolase, leading to excessive activation and autocrine of macrophages and neutrophils, resulting in the accumulation of a large number of pro-inflammatory factors. Then the local inflammation at the lesion is amplified through the inflammatory cascade effect, which eventually results in necrosis and hemorrhage of most pancreatic tissue, releasing more and more cytokines, and induces hypercytokinemia (a cytokine storm). As the disease progresses and pancreatic inflammation involves the intestine, it causes dysfunction of intestinal barrier, which leads to the migration of intestinal flora to the pancreas and blood, followed by pancreatic infection and sepsis. These high levels of risk factors (including trypsin, endotoxin and cytokines) in the blood can damage vascular endothelial cells, trigger systemic inflammatory response, lead to myocardial microcirculatory disturbance, autonomic nerve dysfunction and abnormal autophagy, and eventually result in myocardial injury and cardiac dysfunction.