Abstract
A 74-year-old male patient who was admitted with non–ST-segment elevation myocardial infarction, severe left ventricular impairment, severe mitral regurgitation, and full viability who was turned down for surgery underwent high-risk and indicated multivessel stenting with Impella (Abiomed) support. At 6-month follow-up he was angina free, with complete resolution of the mitral regurgitation. (Level of Difficulty: Intermediate.)
Key Words: myocardial ischemia, myocardial revascularization, percutaneous coronary intervention
Abbreviations and Acronyms: AMICS, acute myocardial infarction with cardiogenic shock; CTO, chronic total occlusion; HR-PCI, high-risk percutaneous coronary intervention; IABP, intra-aortic balloon pump; LAD, left anterior descending; LMS, left main stem; LV, left ventricular; MCS, mechanical circulatory support; MR, mitral regurgitation; OM, obtuse marginal; PCI, percutaneous coronary intervention; RCA, right coronary artery; RCT, randomized controlled trial
Graphical abstract
A 74-year-old male patient who was admitted with non–ST-segment elevation myocardial infarction, severe left ventricular impairment, severe mitral…
History of Presentation
A 74-year-old male patient was admitted on an emergency basis with chest pain and a troponin-T level of 2,000 ng/l. He was treated as being at high risk for non–ST-segment elevation myocardial infarction.
Learning Objectives
-
•
Clinicians will understand the role of hemodynamic support in indicated multivessel stenting in patients with a high risk of periprocedural major adverse events.
-
•
Clinicians will be able to discuss the current global controversy and variation of hemodynamic support in these patients.
Past Medical History
There was no significant medical history. His cardiac risk factors included hypertension, hypercholesterolemia, and a positive family history.
Investigations
The patient had normal renal function with an estimated glomerular filtration rate of 89 ml/min. An electrocardiogram showed sinus rhythm with anterolateral T-wave inversion. Transthoracic echocardiography demonstrated severe left ventricular (LV) impairment with ejection fraction of 23%, inferior and anterior hypokinesis, and severe mitral regurgitation (MR), occupying 70% of the left atrium. Diagnostic angiography revealed severe left main stem (LMS) into left anterior descending (LAD) artery stenosis with chronic total occlusions (CTOs) of both proximal right coronary artery (RCA) and a large first obtuse marginal (OM) vessel. Both distal CTO segments filled from LAD territory collateral vessels.
Management
The case was discussed at our heart team multidisciplinary meeting. Risk scoring revealed an anatomic SYNTAX score of 37, EuroScore 2 mortality score of 9.5%, BCIS Jeopardy score of 12/12, and Washington Protected PCI score of 6. Cardiac magnetic resonance demonstrated 11 viable segments (7 in the LAD territory). Given the high surgical risk, our patient was turned down for coronary artery bypass graft and likely mitral valve replacement. Therefore, Impella (Abiomed)–supported multivessel PCI to achieve complete revascularization was planned with the option of MitraClip (Abbott) for treatment of MR if required.
Interventional procedure and outcome
An Impella CP (femorally) set at P7 (3.2 l/min) and biradial guides were inserted (7-F EBU 3.5 and 6-F AL 0.75) (Figure 1). Intravascular ultrasound examination classified the LMS as having a severe midbody stenosis (minimum lumen area <3 mm2) and the LMS bifurcation as Medina 1, 1, 0 with no significant ostial circumflex disease. In light of this a provisional strategy of stenting LMS and LAD was undertaken, using a 3.5 × 48 mm Boston Scientific Synergy stent. The OM and RCA CTOs, both with low Japanese CTO scores, were successfully opened using an antegrade wire escalation technique, and the following stents were implanted: OM, 2.5 × 28 mm Synergy; RCA, 3.0 × 48 mm Synergy. All stents received appropriate intravascular ultrasound-guided optimization. At the end of the procedure the Impella CP was weaned and removed with 2 ProGlide sutures (Abbott) to achieve hemostasis. Periprocedural pressure traces confirmed repeated loss of pulsatile flow and reliance on Impella to maintain perfusion. In total, 195 ml of iodixanol (Visipaque) contrast medium was used, the patient received <1.0 Gy, and the procedure was completed in 116 min. Throughout the procedure no inotropic support was required.
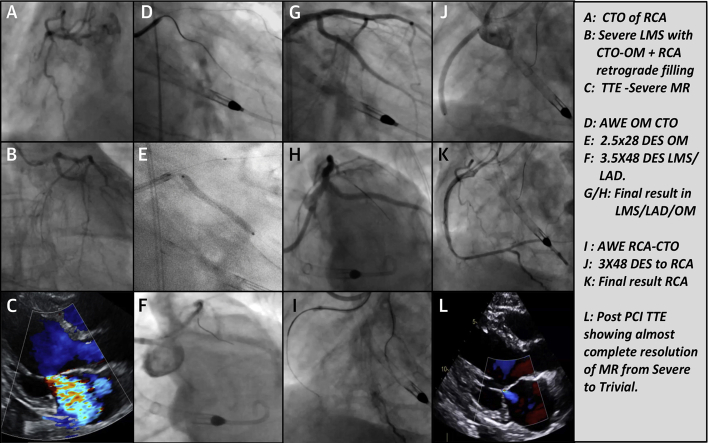
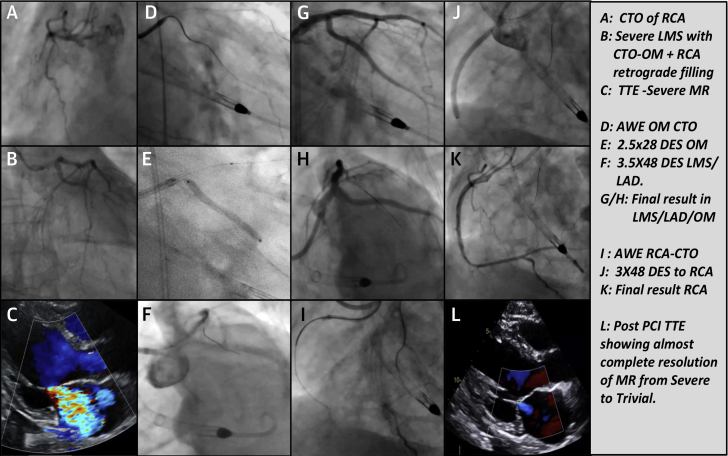
Figure 1.
Original Coronary Angiogram, Echocardiogram (Pre-Procedure and at 6-Month Follow-Up), and Percutaneous Coronary Interventional Procedure Images
(A) Chronic total occlusion (CTO) of the right coronary artery (RCA). (B) Severe left main stem stenosis (LMS) with CTO of the obtuse marginal artery (OM) and RCA retrograde filling. (C) Transthoracic echocardiogram (TTE) showing severe mitral regurgitation (MR). (D) Antegrade wire escalation in CTO of the OM. (E) A 2.5 × 28 mm drug-eluting stent in the OM. (F) A 3.5 × 48 mm drug-eluting stent (DES) in the LMS and left anterior descending coronary artery (LAD). (G and H) Final result in the LMS, LAD, and OM. (I) Antegrade wire escalation in CTO of the LAD. (J) A 3 × 48 mm DES in the RCA. (K) Final result in the RCA. (L) Post-procedural TTE showing almost complete resolution of MR from severe to trivial.
Discussion
Impella CP in complex, high-risk, and indicated PCI is currently not commissioned for use by the National institute of Health and Clinical Excellence (NICE) or National Health Service England. Both European (European Society of Cardiology) and U.S. (American College of Cardiology) guidelines advise mechanical circulatory support (MCS) in high-risk percutaneous coronary intervention (HR-PCI) as a Class IIb indication, whereas the American College of Cardiology gives MCS in acute myocardial infarction with cardiogenic shock (AMICS) a Class I indication (1,2). Significant global variations in Impella use exist, with uptake in the United Kingdom at 0.03% of total PCI cases, whereas in the United States penetration is 10% in both HR-PCI and AMICS cohorts (3). Observational studies and registry data currently constitute the primary evidence base for Impella, with no true randomized controlled trials (RCTs). In our center we recognize that a subset of patients is likely to benefit from the use of Impella support during HR-PCI. We demonstrate a case of high-risk multivessel revascularization in an unstable patient, feasible through use of Impella CP, with substantial symptomatic, clinical, and prognostic benefits.
Follow-up
Our patient made an excellent recovery with no acute kidney injury and was symptom free at 6-month follow-up with no interim hospital admissions. Repeat echocardiogram revealed improvement in LV ejection fraction to 35% with significant resolution of MR, which is now trivial. He is now angina free, in New York Heart Association functional class I, is able to perform all desired activities, and has a markedly improved quality of life.
Conclusions
Our case highlights the benefits of Impella LV support in completion of multivessel PCI in a high-risk and unstable patient. In the absence of access to Impella, a strategy of historical intra-aortic balloon pump (IABP) and inotrope-supported PCI or a conservative symptom-based approach would have been pursued, the former carrying a high risk of periprocedural mortality and morbidity and the latter likely resulting in refractory ischemic cardiomyopathy and recurrent hospitalizations for decompensated heart failure. We recognize that a select cohort of patients potentially stands to gain benefit from the use of Impella CP to facilitate complete and optimal revascularization. Although registry and observational data demonstrate trends toward improvement in some secondary outcomes with Impella use, to date there are no robust RCTs demonstrating a statistically significant primary outcome of mortality benefit with use of this device, in either the AMICS or HR-PCI cohorts. Studies such as ISAR-SHOCK (Impella vs. IABP in AMICS; n = 26), IMPRESS (Impella CP vs. IABP; n = 48, predominantly patients with out-of-hospital cardiac arrest), and PROTECT II (Impella 2.5 vs. IABP in HR-PCI; n = 448) demonstrated equivalent 30-day mortality or adverse event outcomes between Impella and IABP (4, 5, 6). Larger registry data have shown pre-PCI implantation of Impella 2.5 in AMICS (the concept of “unloading”) to be superior to post-PCI implantation (USpella) and safety, feasibility, and usefulness of Impella 2.5 in HR-PCI (Europella). The lack of early data demonstrating a mortality benefit forms the basis on which Impella is not currently funded in the National Health Service (7,8).
However, more recently, studies incorporating the use of MCS, including Impella, into standardized “shock protocols” have demonstrated significant improvements in outcomes with an increase of up to 50% and reported rates of up to 72% survival to hospital discharge (9). Furthermore, Burzotta et al. (10) showed a significant association between Impella-protected HR-PCI and LV recovery that carries important implications regarding longer-term prognosis (10). A primary theme both from registry and more recent observational data is the facilitation of complete revascularization with Impella use, including image-optimized precision stenting, use of adjunctive therapy for calcium modification, and ability to overcome the challenges of multivessel, single remaining vessel, LMS, and CTO HR-PCI in an unstable cohort of patients. Successfully optimized PCI in all these anatomic or lesion subtypes in theory should lead to a reduction in target vessel or target lesion failure and stent complications.
RCTs directly comparing the use of Impella-facilitated HR-PCI against the alternative conventional treatment or medical management (where both surgical revascularization and percutaneous revascularization are declined) are required to identify the patient cohort most likely to gain the greatest incremental benefit from Impella-assisted PCI.
In this case Impella CP allowed safe and complete image-optimized complex multivessel revascularization leading to improved LV function and resolution of MR. This has improved both quality of life and long-term prognosis for our patient. We conclude that in a select group of patients appropriately discussed with the multidisciplinary heart team and filtered on the basis of comorbidities, cardiac hemodynamic status, and anatomic and functional severity of coronary disease, as well as with appropriate risk scoring systems, the use of Impella to support HR-PCI is likely to be of significant benefit both to patients and longer-term PCI outcomes.
Footnotes
Both authors have reported that they have no relationships relevant to the contents of this paper to disclose. Konstantinos Charitakis, MD, served as Guest Associate Editor for this article.
Informed consent was obtained for this case.
References
- 1.Neumann F.J., Sousa-Uva M., Ahlsson A. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40:87–165. doi: 10.1093/eurheartj/ehy855. [DOI] [PubMed] [Google Scholar]
- 2.Levine G.N., Bates E.R., Blankenship J.C. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58:e44–e122. doi: 10.1016/j.jacc.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Myocardial Infarction National Audit Project 2019 Summary Report. (2017/18 data). Available at: https://www.hqip.org.uk/resource/myocardial-ischaemia-national-audit-project-minap-2019-summary-report/#.Xd1OFC2cZQI. Accessed November 2019.
- 4.Seyfarth M., Sibbing D., Bauer I. A randomized clinical trial to evaluate the safety and efficacy of a percutaneous left ventricular assist device versus intra-aortic balloon pumping for treatment of cardiogenic shock caused by myocardial infarction. J Am Coll Cardiol. 2008;52:1584–1588. doi: 10.1016/j.jacc.2008.05.065. [DOI] [PubMed] [Google Scholar]
- 5.Ouweneel D.M., Erikson E., Sjauw K.D. Percutaneous mechanical circulatory support versus intra-aortic balloon pump in cardiogenic shock after acute myocardial infarction. J Am Coll Cardiol. 2017;69:278–287. doi: 10.1016/j.jacc.2016.10.022. [DOI] [PubMed] [Google Scholar]
- 6.O’Neill W.W., Kleiman N.S., Moses J. A prospective, randomized clinical trial of hemodynamic support with Impella 2.5 versus intra-aortic balloon pump in patients undergoing high-risk percutaneous coronary intervention: the PROTECT II study. Circulation. 2012;126:1717–1727. doi: 10.1161/CIRCULATIONAHA.112.098194. [DOI] [PubMed] [Google Scholar]
- 7.O'Neill W.W., Schreiber T., Wohns D.H. The current use of Impella 2.5 in acute myocardial infarction complicated by cardiogenic shock: results from the USPella Registry. J Interv Cardiol. 2014;27:1–11. doi: 10.1111/joic.12080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sjauw K.D., Konorza T., Erbel R. Supported high-risk percutaneous coronary intervention with the Impella 2.5 device: the Europella registry. J Am Coll Cardiol. 2009;54:2430–2434. doi: 10.1016/j.jacc.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 9.Basir M.B., Kapur N.K., Patel K. Improved outcomes associated with the use of shock protocols: updates from the National Cardiogenic Shock Initiative. Catheter Cardiovasc Interv. 2019;93:1173–1183. doi: 10.1002/ccd.28307. [DOI] [PubMed] [Google Scholar]
- 10.Burzotta F., Russo G., Ribichini F. Long-term outcomes of extent of revascularization in complex high risk and indicated patients undergoing Impella-protected percutaneous coronary intervention: report from the Roma-Verona Registry. J Interv Cardiol. 2019 doi: 10.1155/2019/5243913. 5243913. [DOI] [PMC free article] [PubMed] [Google Scholar]