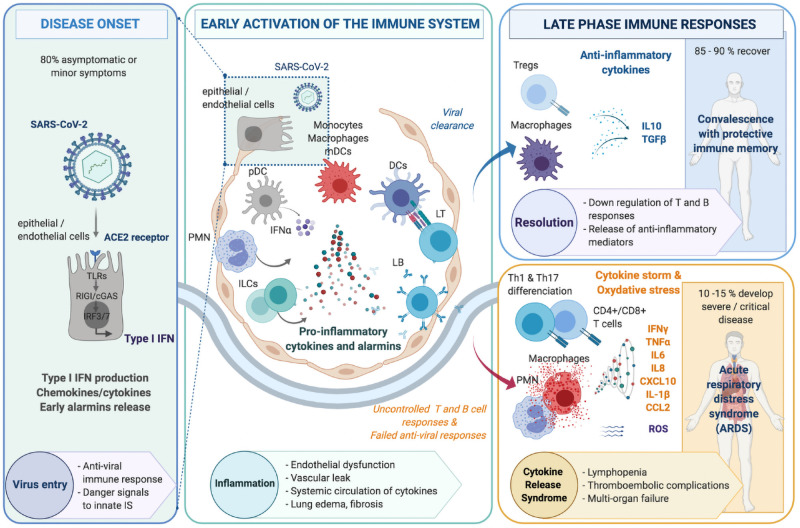
Fig 2. Three step progression towards severe COVID-19.
The pathophysiology of COVID-19 in the airways encompasses schematically three successive steps, including (i) Disease onset following viral infection of alveolar epithelial or endothelial cells expressing the ACE2 receptor (left panel) leading to the activation of the innate immune system, with IFNα production by plasmacytoid dendritic cells (pDC). (ii) An early inflammatory phase within lung tissues where a cross-talk between infected epithelial/endothelial cells and innate immune cells such as monocytes, macrophages, myeloid dendritic cells (mDC) and innate lymphoid cells (ILCs) leads to a release of pro-inflammatory alarmins, cytokines and chemokines (center panel). This results in the activation of adaptive immunity, involving both CD4+ T cell help, CD8+ T cells cytotoxic for virally-infected cells as well as production of neutralizing antibodies against surface viral antigens. (iii) A late inflammatory phase with two potential outcomes: 85 to 90% of cases evolve towards resolution of inflammation with downregulation of T and B cell responses concomitant with the release of anti-inflammatory mediators (right upper panel); whereas 10 to 15% patients rather exhibit major tissue damage and severe acute respiratory distress syndrome (ARDS) caused by a deleterious uncontrolled inflammation linked with persisting T cell activation, excessive myeloid cell activation associated with a cytokine storm as well as oxidative stress (right lower panel).