Abstract
White spots are common side effects of orthodontic treatment, and their presence after debonding appears unesthetic. This study aimed to quantify and compare the visual improvement in postdebonding white spot lesions following fluoride and casein phosphopeptide–amorphous calcium phosphate (CPP–ACP) application. The sample included 42 upper premolars extracted for orthodontic reasons. Universal premolar brackets were bonded to the facial surfaces of the teeth that were exposed to a demineralization solution to create artificial white spot lesions, after which the brackets were debonded. The specimens were randomly allocated to three treatment groups (n = 14, each): acidulated phosphate fluoride (APF) gel application group; CPP–ACP paste application group; and control group. pH cycling was conducted to all groups for 14 days. Quantitative measurements were carried out using a spectrophotometer at the following times: before and after the white spot lesions artificially formed and after treating them. All groups showed significant differences in color change before and after treatment. However, there was no significant difference in the color improvement between the APF gel and CPP–ACP paste application groups. Although CPP–ACP application improved the color of the white spot lesions, it did not differ significantly from that of fluoride application.
Keywords: Color improvement, casein phosphopeptide–amorphous calcium phosphate, fluoride, white spot
INTRODUCTION
The consequences of side effect in any medical treatment may hinder achieving the main treatment goal effectively. The incidence of white spot lesions after orthodontic treatment with a fixed appliance ranged between 73% and 95%[1,2] and was commonly observed in the labiogingival areas of the upper lateral incisors, while those in the posterior teeth were rare Figure 1.[3,4,5]
Figure 1.

White spot lesions seen clinically when debonding (Source: Sudjalim TR, 2006)[5]
White spot lesions represent the early clinical appearance of carious lesions that can be detected visually. They are formed due to demineralization or dissolution of minerals in the enamel subsurface, while the top surface remains intact.[6] The placement of fixed orthodontic appliances on the labial or buccal surfaces of the teeth increases the retentive area for plaque. Moreover, it reduces the self-cleansing mechanism of the saliva and oral muscles, and plaque removal from the areas around the fixed appliances by tooth brushing alone is difficult. If it persists for long, it will increase the risk of white spot lesion formation.[3,4,7]
Reportedly, white spot lesions can occur 1 month after placement of fixed orthodontic appliances and can last up to 5 years after their removal.[8] This can cause clinical problems, especially esthetic issues. Once the fixed appliance is removed, the white spot lesions are seen more clearly.[9]
The noninvasive approaches to treat white spot lesions include application of topical fluoride and casein phosphopeptide–amorphous calcium phosphate (CPP–ACP). Fluoride has been widely used to prevent and inhibit caries development. The most widely used professional topical fluoride is acidulated phosphate fluoride (APF), containing 1.23% of fluoride or 12,300 ppm fluoride at a pH of 3. Low pH environment facilitates fluoride uptake from enamel to form fluorapatite.
The breakdown of casein by trypsin enzymes produces peptides known as phosphopeptide casein/CPP, which can stabilize and bind clusters of ACP and prevent its precipitation into crystals. This increases the solubility of calcium phosphate and its ions in a solution of saliva and plaque.[10] When enamel is exposed to acid, localized CPP–ACP acts as a buffer for the calcium and phosphate ions on the tooth surface, thereby increasing the level of calcium phosphate in the plaque and maintaining a state of supersaturation in the enamel. This supersaturation state decreases demineralization and increases remineralization.[10,11,12] Andersson et al. reported the improvement of white spot lesions after orthodontic treatment with CPP–ACP application.[13]
Clinically, white spot lesion is often seen as white, chalky, and different from the surrounding healthy enamel. However, color assessment may be subjective and unreliable and has several limitations. An objective color assessment requires standardized measurement tools such as spectrophotometry, colorimetry, spectroradiometers, and digital images, which are more reliable than visual qualitative assessment.[14] Our study aimed to quantify and compare the visual improvement in postdebonding white spot lesions following fluoride and CPP–ACP application.
MATERIALS AND METHODS
The laboratory experimental study obtained ethical approval from the Dentistry Research Ethics Committee, Faculty of Dentistry, University of Indonesia no. 3/Ethical Exempted/FKGUI/III/2015. The study sample included 42 upper premolar teeth that had been extracted for orthodontic reasons. Enamel specimens were created by embedding the teeth in decorative acrylic with the buccal surface facing upward. Each specimen was mounted with a standard edgewise premolar bracket, and a “window” measuring 2 mm × 2 mm was made in the gingival area of the bracket. The specimen was then immersed in a demineralization solution (2.2 mm/L calcium chloride, 2.2 mm/L monopotassium phosphate, and 50 mm/L acetic acid; pH 4.8–5) to form an artificial white spot lesion, and subsequently, the bracket was removed. pH cycling was conducted in an incubator at 37°C. Remineralization was simulated using an artificial saliva solution (1.5 mm/L calcium chloride, 0.9 mm/L monopotassium phosphate, and 130 mm/L potassium chloride; pH 7). Then, these samples were randomly divided into the following groups of 14 samples each: fluor application group; CPP–ACP paste application group; and control group. Quantitative measurement of the color characteristics of the specimens was conducted using the CIELAB system, with values of L*, a*, and b* in units, using a spectrophotometer (Konica Minolta CM-2600d) [Figure 2]. This study recorded the following values: the target value (value of the initial enamel surface) recorded before the creation of the artificial white spot; the ΔEstart value obtained after the white spot was artificially formed; and the ΔEend value obtained after the white spot was treated for 14 days. Data were analyzed using IBM SPSS Statistics 20.0, IBM, Indonesia Asia Pacific, Wilcoxon test, with significance set at P ≤ 0.05.
Figure 2.
Illustration of the spectrophotometer used in research and industry (Konica Minolta CM-2600d) (Source: http://www.quiminet.com)
RESULTS
In this study, all the retrieval and data inputs were performed by a single observer. The color changes were measured twice within 24 h. Bland–Altman tests revealed conformity between the first and second measurements of the ΔE before and after treatment values [Figures 3 and 4].
Figure 3.
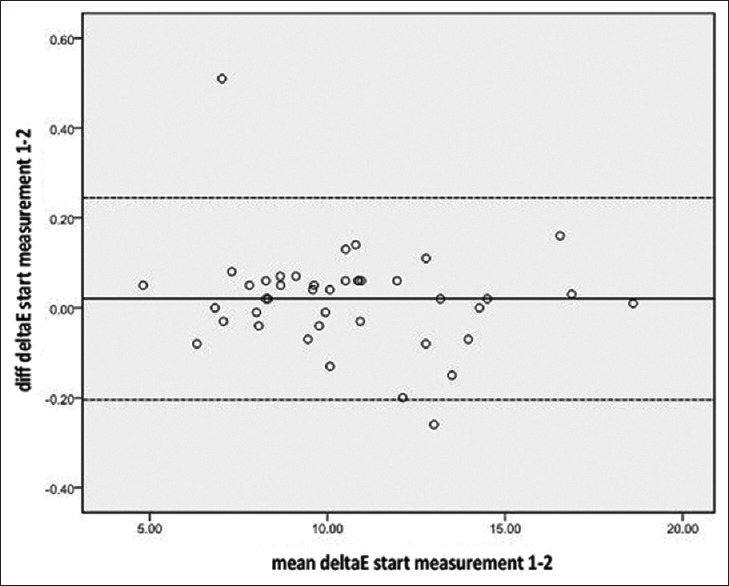
Bland–Altman plot for ΔEstart measurement. (ΔEstart, value obtained after the white spot was artificially formed)
Figure 4.
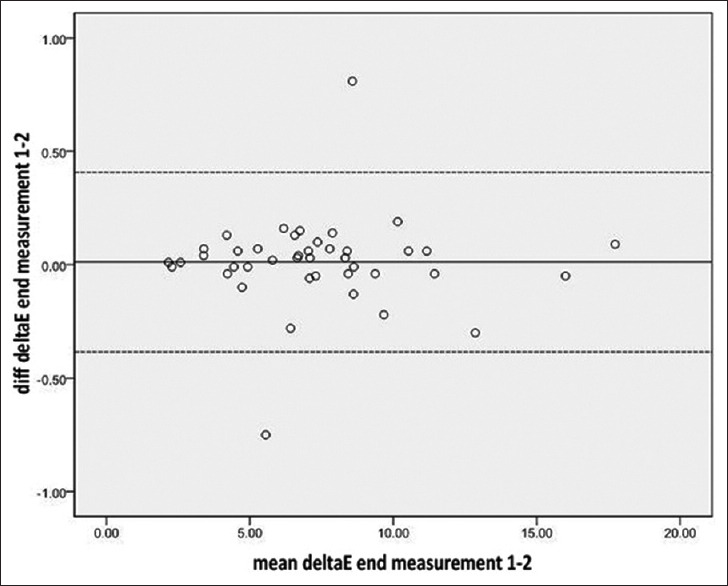
Bland–Altman plot for ΔEend measurement. (ΔEend, value obtained after the white spot was treated for 14 days)
Shapiro–Wilk tests show that almost all data were distributed normally, except for the white spot color before CPP–ACP application with P < 0.05 [Table 1].
Table 1.
Descriptive test results
| Group | n | Value obtained | Color change (unit), mean±SD | Normality test, Shapiro-Wilk (P) |
|---|---|---|---|---|
| Fluoride application | 14 | ΔEstart* | 11.015±1.976 | 0.943 (>−0.05) |
| ΔEend† | 7.358±1.992 | 0.624 (>0.05) | ||
| CPP-ACP application | 14 | ΔEstart | 10.259±2.748 | 0.044 (<−0.05)§ |
| ΔEend | 5.462±2.749 | 0.134 (>−0.05) | ||
| Control | 14 | ΔEstart | 10.348±4.050 | 0.333 (>−0.05) |
| ΔEend | 9.196 ± 3.945 | 0.060 (>−0.05) |
*Value obtained after the white spot was artificially formed, †Value obtained after the white spot was treated for 14 days, §P<0.05, data distribution was not normal. CPP-ACP: Casein phosphopeptide-amorphous calcium phosphate, SD: Standard deviation
Wilcoxon test in each group showed that the null hypothesis was rejected (P < 0.001). This means that all groups provide a significant change before and after treatment [Tables 2-4].
Table 2.
Wilcoxon test results for white spot color change before and after fluoride application
| Group | n | Value obtained | Median (minimum-maximum) | P |
|---|---|---|---|---|
| Fluoride application | 14 | ΔEstart | 10.94 (7.04-14.28) | 0.001 |
| ΔEend* | 7.19 (2.58-10.53) |
*Value obtained after the white spot was treated for 14 days
Table 4.
Wilcoxon test results for white spot color change in the control group
| Group | n | Value obtained | Median (minimum-maximum) | P |
|---|---|---|---|---|
| Control | 14 | ΔEstart* | 9.68 (4.82-18.60) | 0.001 |
| ΔEend† | 8.36 (4.58-17.74) |
*Value obtained after the white spot was artificially formed, †Value obtained after the white spot was treated for 14 days
Table 3.
Wilcoxon test results for white spot color change before and after casein phosphopeptideamorphous calcium phosphate application
| Group | n | Value obtained | Median (minimum-maximum) | P |
|---|---|---|---|---|
| CPP-ACP* application | 14 | ΔEstart† | 9.37 (7.31-16.55) | 0.001 |
| ΔEend‡ | 4.61 (2.16-11.17) |
*P<0.00. †Value obtained after the white spot was artificially formed, ‡Value obtained after the white spot was treated for 14 days. CPP-ACP: Casein phosphopeptideamorphous calcium phosphate
The P value of post hoc Mann–Whitney U-test was > 0.05 in the test between the fluoride application group and CPP–ACP application group, thus accepting the null hypothesis. Furthermore, this means that there was no significant difference in the white spot color change after treatment between the fluoride application and CPP–ACP application groups [Table 5].
Table 5.
Comparison of white spot color changes after treatment in acidulated phosphate fluoride application, casein phosphopeptide-amorphous calcium phosphate application, and control groups
| Group | n | Median (minimum-maximum) | P* |
|---|---|---|---|
| Fluoride application | 14 | 3.18 (1.19-10.18) | <0.001 |
| CPP-ACP† application | 14 | 4.23 (2.55-8.23) | |
| Control | 14 | 0.96 (0.19-2.52) |
*Kruskal-Wallis test, †P<0.001 post hoc MannWhitney U-test: Fluoride application group versus CPP-ACP application group, P=0.05; Fluoride application group versus control group, P<0.001; CPP-ACP application group versus control group, P<0.001. CPP-ACP: Casein phosphopeptide-amorphous calcium phosphate
DISCUSSION
During treatment of the specimens in our study, pH cycling was conducted in an incubator at 37°C, which is the same as the body temperature. pH cycling simulated the process of demineralization and remineralization in vivo, where demineralization occurs in an acidic environment, which was simulated using a demineralization solution (pH 4.4–4.8). Remineralization occurs in a normal environment, which was simulated using an artificial saliva solution (pH 7).[15,16]
Before the hypothesis test, the intraexaminer method was used to avoid the possibility of systematic errors due to several factors such as variation in the morphology of the sample surface, position of the measurement tool relative to the sample surface, humidity, and temperature of the room at the time of measurement, and internal factors of the operator such as tiredness. The intraexaminer method shows very little bias potency. In this study, the mean value of the enamel color change after creating the white spot was 10.54 ± 2.99 units. This value was obtained from the difference in the values of L*, a*, and b* between the white spot color and the target color (enamel color), which was calculated automatically by SpectraMagic NX software with the formula ΔE = (ΔL*2+ Δa*2+ Δb*2)(1/2).
All the groups (fluoride application group, CPP–ACP application group, and control group) showed statistically significant color improvement. Color improvement was demonstrated by a significant decrease in ΔE values. The best white spot color improvement was observed in the CPP–ACP group, followed by the fluoride application group and the control group.
The median of decrease in ΔE after fluoride application was 3.18 (1.19–10.18) units, which means that the color improvement of the white spots was not statistically significant. The ability of fluoride to remineralize enamel is widely known, but there is not enough evidence regarding its effectiveness in esthetically remineralizing the postdebonding white spots. This study used APF, because it can be applied professionally by clinicians and can be better compared with the other self-applied topical fluorides whose optimal results depend on patient compliance. The study by Geiger et al. showed that the rate of compliance in orthodontic patients in using fluoridated mouthwash daily was only 13%.[17] Furthermore, Ogaard et al. stated that high concentration fluorides applied directly to white spot lesions gives poor result esthetically. Because the outer surface of the enamel undergoes remineralization first, the fluoride ions will be blocked from entering the subsurface enamel. This affects the reflection of the light that falls on the enamel surface; hence, a chalky white opaque appearance will remain on the enamel surface.[18,19]
In this study, the white spot color improvement (decrease in ΔE) after CPP–ACP application was 4.23 (2.55–8.23) units, which was the largest value when compared to the fluoride application and control groups, with a statistically and visually significant difference. This result indicates that the lesion was improved closer to the initial enamel color. This is likely because CPP–ACP is able to fill the subsurface enamel pores.[20] In the latest study by Yuan et al., there were no significant color changes of postdebonding white spot lesions after CPP–ACP application, probably because it was applied only once, followed by follow-up after 6 weeks.[9] In contrast to this study, which CPP–ACP were applied once in 24 h for 14 days simulated the clinical situation of daily use by patients.
This study revealed that the difference in the white spot color improvement between the fluoride application group and CPP–ACP application group was not statistically significant. This was because the samples in this study were followed up after 2 weeks, with reference to the manufacturer's manual that said optimal results could be obtained after 14 days of use. Bröchner et al. reported that improvement in the lesion resulting from a remineralization agent might be achieved in the long term.[21]
Our study was limited in its ability to evaluate the effectiveness of a remineralization agent, which is one of the noninvasive approaches for treating postdebonding white spots. The other treatment choice is the invasive approach, which reportedly gave better esthetic results in several studies. One of them was the study conducted by Pliska et al. that compared CPP–ACP application and microabrasion in treating postorthodontic white spot lesions. Microabrasion gave significantly better results, because this method allows the hypermineralized tissue located in the outer surface of lesions to be removed so that the minerals can penetrate the inner part of the lesions deeply.[22] Another limitation of our study was that the treatment duration and follow-up time. Moreover, because our study was conducted in vitro, it was difficult to simulate the complex oral clinical environment.
CONCLUSIONS
From this study, it can be concluded that CPP–ACP provided better visual improvement in the white spot color changes but did not show a statistically significant difference from that of fluoride.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to acknowledge Prof. Endang W. Bachtiar for Proofread the manuscript.
REFERENCES
- 1.Lovrov S, Hertrich K, Hirschfelder U. Enamel demineralization during fixed orthodontic treatment-incidence and correlation to various oral-hygiene parameters. J Orofac Orthop. 2007;68:353–63. doi: 10.1007/s00056-007-0714-1. [DOI] [PubMed] [Google Scholar]
- 2.Richter AE, Arruda AO, Peters MC, Sohn W. Incidence of caries lesion among patients treated with treated with comprehensive orthodontics. Am J Orthod Dentofacial Orthop. 2011;139:657–64. doi: 10.1016/j.ajodo.2009.06.037. [DOI] [PubMed] [Google Scholar]
- 3.Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982;81:93–7. doi: 10.1016/0002-9416(82)90032-x. [DOI] [PubMed] [Google Scholar]
- 4.Mizrahi E. Surface distribution of enamel opacities following orthodontic treatment. Am J Orthod. 1983;84:323–31. doi: 10.1016/s0002-9416(83)90348-2. [DOI] [PubMed] [Google Scholar]
- 5.Sudjalim TR, Woods M, Manton D. Prevention of white spot lesions in orthodontic practice: A contemporary review. Aust Dent J. 2006;51:284–9. doi: 10.1111/j.1834-7819.2006.tb00445.x. [DOI] [PubMed] [Google Scholar]
- 6.McIntyre JM. Dental caries-The major cause of tooth damage. In: Mount GJ, Hume WR, editors. Preservation and Restoration of Tooth Structure. Queensland: Knowledge Books and Software; 2005. pp. 21–6. [Google Scholar]
- 7.Mitchell L. An Introduction to Orthodontics. Oxford: Oxford University Press; 2007. pp. 4–5. [Google Scholar]
- 8.Ogaard B, Rolla G, Arends J. Orthodontic appliances and enamel demineralization. Part 1. Lesion development. Am J Orthod Dentofacial Orthop. 1988;94:68–73. doi: 10.1016/0889-5406(88)90453-2. [DOI] [PubMed] [Google Scholar]
- 9.Yuan H, Li J, Chen L, Cheng L, Cannon RD, Mei L. Esthetic comparison of white spot lesion treatment modalities using spectrometry and fluorescence. Angle Orthod. 2014;84:343–9. doi: 10.2319/032113-232.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reynolds EC, Walsh LJ. Additional aids to the remineralization of tooth structure. In: Mount GJ, Hume WR, editors. Preservation and Restoration of Tooth Structure. Queensland: Knowledge Books and Software; 2005. pp. 112–8. [Google Scholar]
- 11.Reynolds EC. Calcium phosphate-based remineralization systems: Scientific evidence? Aust Dent J. 2008;53:268–73. doi: 10.1111/j.1834-7819.2008.00061.x. [DOI] [PubMed] [Google Scholar]
- 12.Willershausen B, Schulz-Dobrick B, Gleissner C. In vitro evaluation of enamel remineralisation by a casein phosphopeptide-amorphous calcium phosphate paste. Oral Health Prev Dent. 2009;7:13–21. [PubMed] [Google Scholar]
- 13.Andersson A, Sköld-Larsson K, Hallgren A, Petersson LG, Twetman S. Effect of a dental cream containing amorphous cream phosphate complexes on white spot lesion regression assessed by laser fluorescence. Oral Health Prev Dent. 2007;5:229–33. [PubMed] [Google Scholar]
- 14.Trakyali G, Ozdemir FI, Arun T. Enamel colour changes at debonding and after finishing procedures using five different adhesives. Eur J Orthod. 2009;31:397–401. doi: 10.1093/ejo/cjp023. [DOI] [PubMed] [Google Scholar]
- 15.Kumar V, Itthagarun A, King N. The effect of casein phosphopeptide-amorphous calcium phosphate on remineralization of artificial caries-like lesions: An in vitro study. Aust Dent J. 2008;53:34–40. doi: 10.1111/j.1834-7819.2007.00006.x. [DOI] [PubMed] [Google Scholar]
- 16.Ten Cate JM, Duijsters PP. Alternating demineralization and remineralization of artificial enamel lesions. Caries Res. 1982;16:201–10. doi: 10.1159/000260599. [DOI] [PubMed] [Google Scholar]
- 17.Geiger AM, Gorelick L, Gwinnett AJ, Benson BJ. Reducing white spot lesions in orthodontic populations with fluoride rinsing. Am J Orthod Dentofacial Orthop. 1992;101:403–7. doi: 10.1016/0889-5406(92)70112-N. [DOI] [PubMed] [Google Scholar]
- 18.Ogaard B, Rølla G, Arends J, Ten Cate JM. Orthodontic appliances and enamel demineralization. Part 2. Prevention and treatment lesions. Am J Orthod Dentofacial Orthop. 1988;94:123–28. doi: 10.1016/0889-5406(88)90360-5. [DOI] [PubMed] [Google Scholar]
- 19.Willmot D. White spot lesions after orthodontic treatment. Semin Orthod. 2008;14:200–8. [Google Scholar]
- 20.Reynolds EC. Casein phosphopeptide-amorphous calcium phosphate: The scientific evidence. Adv Dent Res. 2009;21:25–9. doi: 10.1177/0895937409335619. [DOI] [PubMed] [Google Scholar]
- 21.Bröchner A, Christensen C, Kristensen B, Tranæus S, Karlsson L, Sonnesen L, et al. Treatment of post-orthodontic white spot lesions with casein phosphopeptide-stabilised amorphous calcium phosphate. Clin Oral Investig. 2011;15:369–73. doi: 10.1007/s00784-010-0401-2. [DOI] [PubMed] [Google Scholar]
- 22.Pliska BT, Warner GA, Tantbirojn D, Larson BE. Treatment of white spot lesions with ACP paste and microabrasion. Angle Orthod. 2012;82:765–9. doi: 10.2319/111611-710.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


