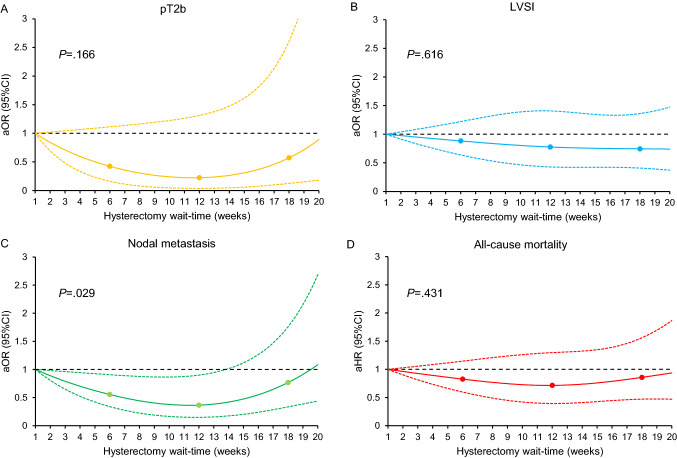
Fig. 1.
Associations between hysterectomy wait-time and oncologic outcomes and all-cause mortality (adjusted model). A total of 2,732 women with clinical stage IA cervical cancer who had primary hysterectomy were examined. Adjusted-odds ratio for pathological stage T2b (A), LVSI (B), and nodal metastasis (C), and adjusted-hazard ratio for all-cause mortality (D) are shown by week of hysterectomy wait-time. Waiting time was coded using restricted cubic spline transformation with clinically relevant cut-points at 6, 12, and 18 weeks. The Y-axis represents the effect size (adjusted-odds ratio or adjusted-hazard ratio). The X-axis represents the wait-time (week) from cervical cancer diagnosis to surgical treatment with hysterectomy. Week 1 is set as the reference. The solid line represents the estimate as adjusted-effect size. The dashed lines are corresponding 95% confidence interval. Three dots represent the knots. P values indicate the overall associations. For the surgical-pathological factors, adjusting factors were age, year, race/ethnicity, insurance status, average neighborhood household income, average neighborhood education level, year of diagnosis, comorbidity score, urban/rural type, histology type, tumor differentiation, stage, and hospital factors (location and setting). For all-cause mortality, lympho-vascular space invasion, pathological parametrial tumor involvement, and lymph node metastasis were additionally included as covariates in the multivariable Cox proportional hazard regression model