Abstract
Immunoglobulin G4–related disease is a systemic fibroinflammatory disease; pericardial involvement has occasionally been reported in publications. A 79-year-old man with biopsy-proven immunoglobulin G4–related disease with pleural involvement was admitted in acute heart failure, with imaging and hemodynamic studies consistent with constrictive pericarditis. He was treated with corticosteroids for 2 months with partial response manifest by decreases in pericardial thickening and immunoglobulin G4 levels. However, persistent constriction required pericardiectomy, leading to significant symptomatic improvement. (Level of Difficulty: Intermediate.)
Key Words: constrictive pericarditis, IgG4 related disease
Abbreviations and Acronyms: CP, constrictive pericarditis; IgG4-RD, immunoglobulin G4–related disease; TTE, transthoracic echocardiogram
Graphical abstract

Immunoglobulin G4–related disease is a systemic fibroinflammatory disease; pericardial involvement has occasionally been reported in publications. A…
History of Presentation
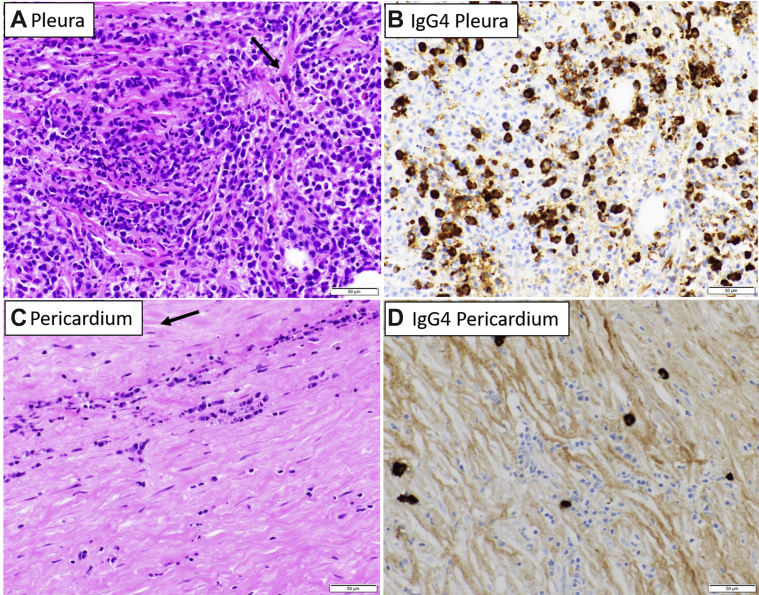
A 79-year-old man with a history of recurrent right-sided loculated pleural effusion presented with progressive dyspnea and was found to be in acute heart failure. Two months before admission he underwent video-assisted thoracoscopic surgery with pleural biopsy and mediastinoscopy with lymph node biopsy. Lymph node biopsy revealed a collagenized granuloma, and the pleural biopsy demonstrated moderate to marked lymphoplasmacytic inflammation and fibrosis with a focal storiform pattern. Most of the plasma cells tested positive for immunoglobulin G4 (IgG4) by immunohistochemical staining. On the basis of the presence of focal storiform fibrosis and numerous IgG4-positive plasma cells, the pleural disease was believed to be consistent with IgG4-related disease (Figures 1A and 1B).
Learning Objectives
-
•
To understand the physiology, pathology, and hemodynamics of CP.
-
•
To recognize IgG4-RD as a possible cause of CP and understand management options.
Figure 1.
Pleural and Pericardial Pathology
(A) Section of the pleural biopsy shows dense lymphoplasmacytic inflammation with focal storiform fibrosis (arrow). (B) Immunohistochemical stain for immunoglobulin G4 antibody shows numerous immunoglobulin G4–positive plasma cells. The patient subsequently presented with constrictive pericarditis. Pericardiectomy was performed after only partial clinical response to steroids. The pericardium shows (C) dense fibrosis with focal storiform pattern (arrow) and only mild lymphoplasmacytic inflammation with (D) few immunoglobulin G4–positive cells.
On this current presentation to the emergency department, he was afebrile, his heart rate was 96 beats/min, blood pressure was 117/76 mm Hg, and oxygen saturation was 94% on 3 l of oxygen through a nasal cannula. Examination was significant for jugular venous distention, decreased breath sounds in the right lung field, abdominal distention, and 3+ edema bilaterally. Laboratory data were significant for a creatinine concentration of 1.46 mg/dl similar to baseline, white blood cell count of 7.5 × 103/μl, hemoglobin of 13.2 g/dl, and platelet count of 189 × 103/μl. The electrocardiogram demonstrated sinus rhythm with an incomplete right bundle branch block and a left anterior fascicular block. Chest computed tomography was obtained and showed a large right-sided pleural effusion, a pericardial effusion with some degree of pericardial thickening (up to 6 mm), and a few subcentimeter mediastinal lymph nodes (Figure 2A). Pericardial calcifications were absent. A transthoracic echocardiogram (TTE) revealed a left ventricular ejection fraction of 55%, normal right ventricular function, and a prominent septal bounce without pericardial effusion (Figures 3A and 3B, Video 1). The study was of limited quality to evaluate tissue velocities or hepatic vein Doppler imaging adequately.
Figure 2.
Chest Computed Tomography
(A) Right-sided pleural effusion and pericardial thickening of 6 mm (arrow). (B) Two months after corticosteroid therapy, recurrent pleural effusion with decreased pericardial thickening (now 3 mm) (arrow) is present. Pericardial calcifications are not identified.
Figure 3.
Echocardiogram
(Aand B) Contrast-enhanced echocardiograms demonstrating septal bounce, or motion of the interventricular septum (arrows) toward the left ventricle in early diastole, more pronounced during deep inspiration.
Online Video 1.
Echocardiogram
Contrast-enhanced echocardiogram demonstrating septal bounce, or motion of the interventricular septum toward the left ventricle in early diastole, more pronounced during deep inspiration.
Past Medical History
The patient had a pleural effusion that was thought to be related to IgG4-RD, as well as chronic diastolic heart failure.
Differential Diagnosis
The differential diagnosis included constrictive pericarditis (CP) related to IgG4-RD, CP related to alternative causes (viral, idiopathic), chronic diastolic heart failure, and pulmonary hypertension.
Investigations
A diagnosis of IgG4-RD CP was suspected. Immunoglobulin levels were obtained, with a total IgG level of 2,854 mg/dl (normal range 768 to 1,632 mg/dl) and an IgG subclass 4 level of 306 mg/dl (normal range 1 to 123 mg/dl). Additional laboratory data were significant for an antinuclear antibody value of 1:320 (normal <1:80), a complement C3 level of 126 mg/dl (normal 80 to 180 mg/dl), and a C4 level of 18 mg/dl (normal 10 to 45 mg/dl). The patient underwent cardiac magnetic resonance, which demonstrated septal shudder and septal bounce (Figures 4A and 4B, Video 2). Simultaneous left- and right-sided heart catheterization demonstrated enhanced ventricular interdependence with inspiratory increase in right ventricular pressure and a simultaneous decrease in left ventricular pressures (Figure 5). At the time of catheterization, the mean pulmonary artery pressure was 17 mm Hg, with pulmonary vascular resistance of 1 WU. Additionally, the right and left ventricular end-diastolic pressures were equal at 18 to 20 mm Hg, and a dip-and-plateau pattern was noted. The patient was started on a regimen of prednisone, 60 mg orally daily, and he underwent diuresis over the course of 10 days with a plan to re-evaluate his clinical status over the next few months and to determine the need for pericardiectomy.
Figure 4.
Cardiac Magnetic Resonance
(Aand B) Cardiac magnetic resonance during normal breathing demonstrating septal bounce, or motion of the interventricular septum (arrows) toward the left ventricle in early diastole.
Online Video 2.
Cardiac Magnetic Resonance
Cardiac magnetic resonance during normal breathing demonstrating septal bounce, or motion of the interventricular septum toward the left ventricle in early diastole.
Figure 5.
Simultaneous Right and Left Ventricular Pressure Tracings
Ventricular discordance is demonstrated as an inspiratory increase in right ventricular (RV) pressure with a simultaneous decrease in left ventricular (LV) pressure (arrows). The opposite phenomenon occurs on expiration. The RV and LV end-diastolic pressures were equalized at 18 to 20 mm Hg. The mean pulmonary artery pressure is 17 mm Hg, with a pulmonary vascular resistance of 1 WU. A dip-and-plateau pattern is noted.
Management
Two months later he was readmitted with progressive dyspnea and weight gain. Repeat chest computed tomography demonstrated a large, right-sided pleural effusion with pericardial thickening slightly decreased from the previous study (3 mm from 6 mm) (Figure 2B), and his IgG 4 level had decreased to 117 mg/dl. Repeat TTE was significant for septal bounce unchanged from his initial study. He was therefore referred to cardiac surgery for pericardiectomy. The patient underwent phrenic-to-phrenic pericardial excision. Intraoperatively, the pericardium was thickened, with patches of calcification. Microscopically, the pericardium showed predominantly fibrosis, with focal suggestion of storiform fibrosis and only mild lymphoplasmacytic inflammation with very few IgG4-positive plasma cells (Figures 1C and 1D). Although the number of IgG4 plasma cells did not meet the published criteria for diagnosing IgG4-related disease, given the patient’s history of previous pleural involvement and the presence of elevated serum IgG and IgG4 levels before steroid treatment, a diagnosis of IgG4-related disease involving the pericardium was favored. Working with our rheumatology colleagues, we were unable to identify additional manifestations of the disease or other autoimmune conditions.
Discussion
Initially described as a disease of the pancreas, IgG4-RD is an immune-mediated fibroinflammatory condition that can affect virtually every organ system. Pathological findings include lymphoplasmacytic infiltration with a high ratio of IgG4-positive plasma cells to IgG-positive plasma cells (1, 2, 3, 4). Cardiovascular manifestations include aortitis, pericarditis, and coronary arteritis or periarteritis. The main therapy for IgG4-RD consists of corticosteroids, with prednisone at a dose of 30 mg/day to 1 mg/kg/day (2). Approximately one-half to two-thirds of patients respond within weeks of treatment (2,4).
There are scant published data to inform the management of CP caused by IgG4-RD, and the response to corticosteroid therapy in CP is unknown. Sekiguchi et al. (5) described a 29-year-old woman with biopsy-proven IgG4-RD manifest by pleural effusions requiring video-assisted thoracoscopic surgery and decortication who had evidence of CP by echocardiography, as well as pericardial thickening on computed tomography. After 3 months of corticosteroid treatment, imaging no longer showed constrictive physiology, and she was free of symptoms (5). Several case reports have noted resolution of constriction and improvement in symptoms following pericardiectomy. However, in those instances, IgG4-RD was usually diagnosed after pericardiectomy, patients were sicker and at times in shock, and steroid therapy was not attempted before surgery (3).
By contrast, our patient had biopsy-proven IgG4-RD of the pleura with CP demonstrated by TTE findings of septal shudder and bounce, cardiac magnetic resonance demonstration of the same, and invasive hemodynamics demonstrating ventricular discordance. An initial trial of corticosteroid therapy was attempted with partial response manifest by decrease in pericardial thickening and IgG4 levels. Similarly, Kondo et al. (6) described a case of a 78-year-old man with IgG4-RD leading to fibroinflammatory lesions of the pericardium, pleura, and bile ducts. After 1 month of steroid therapy, this patient had resolution of pleural effusions and improved liver function test results; however, CP persisted and required pericardiectomy (6). Although it is possible that more significant improvement would have been noted with a longer treatment course in our case, ongoing CP with recurrent limiting symptoms prompted surgery.
Follow-Up
After pericardiectomy, the patient’s central venous pressure dropped from 18 mm Hg to 10 mm Hg. He had an uncomplicated post-operative course and underwent steroid tapering. On 2-month follow-up, his anasarca had resolved, and his exercise tolerance had greatly improved.
Conclusions
We described a case of CP in a patient with biopsy-proven IgG4-RD of the pleura who demonstrated an incomplete response to corticosteroid therapy with resolution of CP following pericardiectomy. Our case highlights the need to consider IgG4-RD in cases of idiopathic CP. Although there are insufficient published data to inform the response to steroids in cases of CP secondary to IgG4-RD, a trial of corticosteroid treatment in stable patients with close monitoring of symptoms may be reasonable. The finding that a significant fibrotic component may limit steroid response emphasizes the importance of early diagnosis.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
Appendix
For supplemental videos, please see the online version of this paper.
References
- 1.Stone J.H., Zen Y., Deshpande V. IgG4-related disease. N Engl J Med. 2012;336:539–551. doi: 10.1056/NEJMra1104650. [DOI] [PubMed] [Google Scholar]
- 2.Mavrogeni S., Markousis-Mavrogenis G., Kolovou G. IgG4-related cardiovascular disease. The emerging role of cardiovascular imaging. Eur J Radiol. 2017;86:169–175. doi: 10.1016/j.ejrad.2016.11.012. [DOI] [PubMed] [Google Scholar]
- 3.Sekiguchi H., Horie R., Suri R.M., Yi E.S., Ryu H.J. Constrictive pericarditis caused by immunoglobulin G4-related disease. Circ Heart Fail. 2012:5e30–5e31. doi: 10.1161/CIRCHEARTFAILURE.111.966408. [DOI] [PubMed] [Google Scholar]
- 4.Matsumiya R., Hosono O., Yoshikawa N. Elevated serum IgG4 complicated by pericardial involvement with a patchy 18F-FDG uptake in PET/CT: atypical presentation of IgG4-related disease. Intern Med. 2015;54:2337–2341. doi: 10.2169/internalmedicine.54.4340. [DOI] [PubMed] [Google Scholar]
- 5.Sekiguchi H., Horie R., Utz J.P., Ryu J.H. IgG4-related systemic disease presenting with lung entrapment and constrictive pericarditis. Chest. 2012;142:781–783. doi: 10.1378/chest.11-2608. [DOI] [PubMed] [Google Scholar]
- 6.Kondo T., Uehara T. Immunoglobulin G4-related disease with fibroinflammatory lesions in the pleura, bile ducts and pericardium. CMAJ. 2016;188:972. doi: 10.1503/cmaj.160186. [DOI] [PMC free article] [PubMed] [Google Scholar]